Year: 2014, Volume: 5, Issue: 3, July-September
Original Article
Cara L. Sedney, Terrence Julien, Jacinto Manon, Alison Wilson
Original Article
Virendra C. Patil, Kushal Choraria, Neeraj Desai, Sumit Agrawal
Original Article
Deepak Bandlish, Nilay Biswas, Sumit Deb
Original Article
Forhad Hossain Chowdhury, Mohammod R. Haque, Khandkar A. Kawsar, Mainul H. Sarker, Mahmudul Hasan, Atul H. Goel
Original Article
Abdul Rashid Bhat, Muhammed Afzal Wani, Altaf Rehman Kirmani, Altaf Umar Ramzan
Original Article
Salma Bensbaa, Loubna Agerd, Saïd Boujraf, Chadya Araab, Rachid Aalouane, Ismail Rammouz, Farida Ajdi
Original Article
Vikram Huded, Rithesh R. Nair, Devashish D. Vyas, Bhumir N. Chauhan
Case Report
Arvind G. Martin, Mutum Samarendra Singh, Badrisyah Idris, Jafri Malin Abdullah
Case Report
Andi Sadayandi Ramesh, Mahadevan Anita, Saini Jitender, Sampath Somanna
Case Report
Girish Baburao Kulkarni, Veerendrakumar Mustare, Masoom Abbas Mirza
Case Report
Swaroopa Pulivarthi, Byron Simmons, John Shearen, Murali Krishna Gurram
Case Report
T. M. Anoop, Nidhi Jain, Sreejith G. Nair, Geetha Narayanan
Case Report
Sumantra Sarkar, Madhumita Nandi, Rakesh Mondal, Sandip Kumar Mandal
Case Report
Pravin Salunke, Devi Prasad Patra, Sameer Futane, Ritambhara Nada
Case Report
Subhash Kumar
Case Report
Mehdi Darmoul, Atef Ben Nsir, Mohamed Kilani, Mohamed Nejib Hattab
Case Report
Abdul Qayyum Rana, Muhammad Saad Yousuf, Muhammad Zainuddin Hashmi, Zakerabibi Mohammed Kachhvi
Case Report
Sudhansu Sekhar Mishra, Sanjay Kumar Behera, Manmath Kumar Dhir, Satya Bhusan Senapati
Short Communication
Mark B. Detweiler
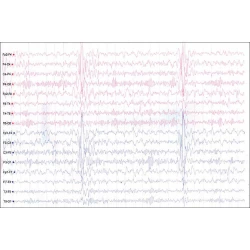
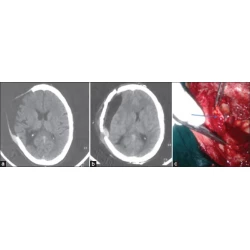
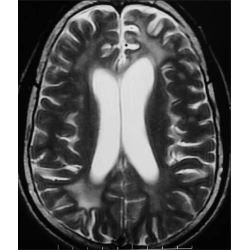
Images in Neurosciences
C. J. Suresh Chandran
Letters to the Editor
Omekareswar Rambarki, Alugolu Rajesh
Letters to the Editor
Mahendra Javali, Ramshekar Menon, Rahul Chakor
Letters to the Editor
Ather Muneer
Letters to the Editor
Khichar Shubhakaran
Letters to the Editor
Abdul Qayyum Rana, Mohamed Sufian Masroor, Beenish Ismail
Letters to the Editor
Thomas I. Lemon, Drew Davies




























Commentary
Commentary
Keerati Hongsakul
Full text |
|  PDF
PDF