Translate this page into:
Extramedullary Tanycytic Ependymoma in a 12-Year-Old Boy
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Tanycytic Ependymomas (TE), rare WHO Grade II ependymomas,[1] are primarily found in the intramedullary spinal cord[23] of adults or within intraventricular regions of children's brains.[23] TEs are rarely found on the extramedullary spinal cord[23] and are more frequently seen in the cervical/cervicothoracic spinal cord than the thoracic, lumbar, or cauda equine.[23] A confident diagnoses of spinal cord TEs requires immunohistochemical (IHC) stain[234] in conjunction with clinical presentation and light microscopy. The treatment is generally surgical,[2] and postsurgical prognosis is good with tumor regrowth rarely seen.[2]
A 12-year-old boy presented with 3 months of intermittent low back pain that radiated bilaterally to his upper thighs. His neurological examination was nonfocal and uneventful except for positive bilateral straight leg raising test. A lumbar spine magnetic resonance imaging (MRI) revealed an intradural, extramedullary mass at L1–L3 region, inferior to the conus medullaris and inside the cauda equina. Homogeneous enhancement and mass effect were also observed on the cauda equina roots [Figure 1a and b]. The patient underwent L1-L2-L3 osteoplastic laminectomies for gross total resection (GTR). Intraoperative visualization showed the tumor within the subarachnoid space and attached to the filum terminale and a few nerve roots [Figure 2a]. Intraoperative neurophysiological monitoring was used to ensure safe detachment of nerves from tumor. The tumor was removed in one piece [Figure 2b] with frozen sections sent for biopsy. Filum terminale could not be visualized clearly, and no nerve roots were sacrificed.
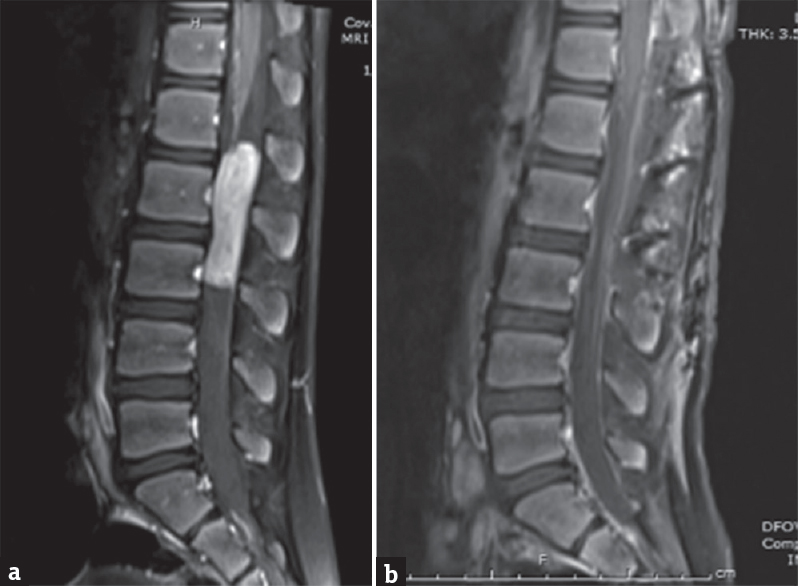
- Preoperative (a) and postoperative (b) sagittal post contrast magnetic resonance imagings

- Intraoperative pictures showing before (a) and after (b) gross total resection
Light microscopy of H and E stained sections demonstrated spindle cell neoplasms of lowtomoderate cellularity with vacuolated cells [Figure 3] and illdefined perivascular pseudorosettes [Figure 4] on light microscopy. High-grade features such as increased mitoses or necrosis were not observed. IHC stains were positive for glial fibrillary acidic protein [Figure 5] and dot-like positivity for epithelial membrane antigen [Figure 6].

- Vacuolated Cells on Hematoxylin and Eosin Stain at 400x

- Inconspicuous Pseudorosettes on Hematoxylin and Eosin Stain at 100x

- Glial Fibrillary Acidic Protein Stain on Immunohistochemical Stain at 400x

- Epithelial Membrane Antigen Stain on Immunohistochemical Stain at 200x
Postoperative MRIs confirmed GTR with no remaining lesions or neurological deficits [Figure 1b]. After consulting with pediatric neurooncology and discussing with parents, the boy received prophylactic proton therapy to the tumor bed. A 2 years’ follow-up showed neither recurrence of the tumor nor neurological deficits.
Rare features of the TE were encountered. TEs are not generally seen in the pediatric population and most incidences are reported in adults − mean age between 40 and 42-year-old.[23] If present in children, TEs are more likely to be found in the brain's intraventricular regions[2] or the intramedullary cervico/cervicothoracic region[23] of the spinal cord. In contrast to the mean age and location, this patient was 12-year-old, and his TE was in the extramedullary cauda equina. Only three other cases of a pediatric spinal TEs have been reported, with one involving an extramedullary TE in the cauda equina of a 10-year-old girl.[145]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The cytogenetic basis for classifying ependymomas. J Neuropathol Exp Neurol. 1978;37:103-18.
- [Google Scholar]
- The clinical features and surgical outcomes of spinal cord tanycytic ependymomas: A report of 40 cases. World Neurosurg. 2017;106:60-73.
- [Google Scholar]
- Pediatric tanycytic ependymoma of the cauda equina: Case report and review of the literature. J Child Neurol. 2008;23:451-4.
- [Google Scholar]
- Spinal tanycytic ependymoma associated with neurofibromatosis type 2 – Case report. Neurol Med Chir (Tokyo). 2001;41:513-6.
- [Google Scholar]





