Translate this page into:
A Treatable Encephalopathy in a Peritoneal Dialysis Patient - Cefepime-Induced Encephalopathy
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a patient with end-stage renal disease on peritoneal dialysis, who developed encephalopathy after receiving a few doses of cefepime. He recovered clinically and electroencephalographically after having discontinued the culprit agent and undergone hemodialysis. This case highlights the importance of promptly recognizing this reversible encephalopathy, which can lead to the avoidance of unnecessary workup, reduce the length of hospital stay, and thereby improve the patients’ outcome.
Keywords
Cefepime
encephalopathy
myoclonus
peritoneal dialysis
triphasic waves
INTRODUCTION
Cefepime is a fourth-generation cephalosporin antibiotic, which has been used extensively in the hospital settings. Its neurotoxicity effects in patients with renal failure or normal renal function have been reported. However, the reports on cefepime-induced encephalopathy in peritoneal dialysis patients are scarce.
CASE REPORT
A 66-year-old male was admitted with a 1-week history of fever and treated for urinary tract infection. His creatinine level upon presentation was 16.4 mg/dL. His past medical history included stroke and end-stage renal disease, for which he was on continuous ambulatory peritoneal dialysis (CAPD) for the past 2 years. He was started on intravenous (IV) ceftriaxone 1 g daily for 3 days and subsequently escalated to IV cefepime 1 g bd (non-CAPD dose) as fever remained unsettled. Fever resolved with day 2 of cefepime, and he felt better in general. On day 3 of cefepime, he was found to be less responsive and confused. In total, he had received 5 g of cefepime before he became neurotoxic.
He did not obey commands and had no verbal output on examination. His vital signs were stable with no fever. He had myoclonic jerks. His pupils were bilaterally equal and reactive. He had no neck stiffness or long-tract signs. Apart from stable anemia, repeated full blood count did not show any leukocytosis. C-reactive protein level was not elevated. There were no electrolyte imbalances. Renal function profile was static. Urgent brain computed tomography showed no new infarcts or hemorrhage. Lumbar puncture was performed with an opening pressure of 15 cm H2O. The cerebrospinal fluid count and biochemistry were within normal limits. His electroencephalography (EEG) [Figure 1] showed background slow activity with generalized triphasic waves. Cefepime was identified as the culprit of confusion and immediately stopped. He was resumed with his CAPD regime.
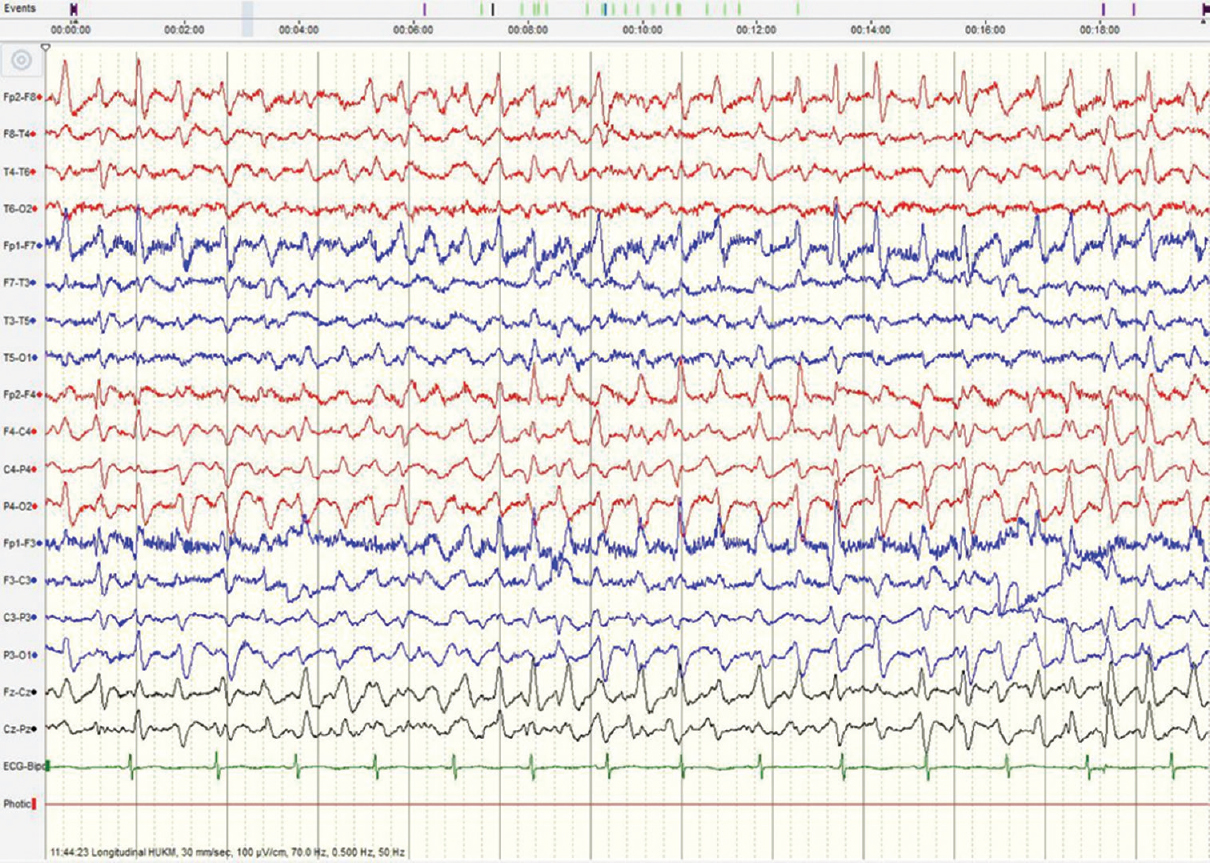
- Electroencephalography shows triphasic waves with no alpha rhythm
On day 7 of admission, he became drowsier with Glasgow Coma Scale (GCS) of 9/15 with E2, V2, and M5, and was transferred to the intensive care unit (ICU) for closer observation. Urgent magnetic resonance imaging of the brain revealed no significant abnormalities apart from his old infarcts.
CAPD was converted to hemodialysis on admission to ICU. Postdialysis, he became more alert and responsive. In subsequent days, his GCS returned to full. A repeated EEG [Figure 2] on day 8 of illness showed theta activity with resolution of triphasic waves. He was subsequently transferred back to the general ward and resumed with CAPD. He remained well upon clinic review.
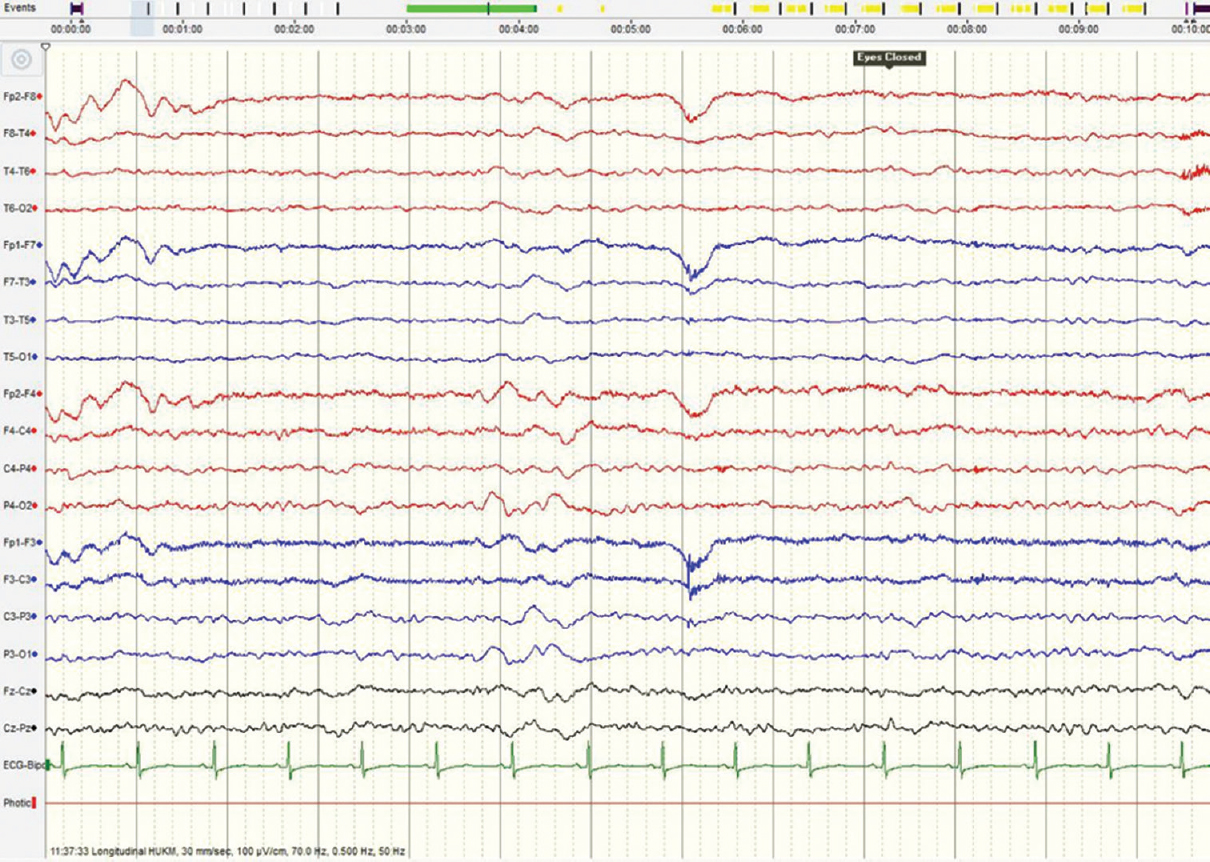
- Electroencephalography shows the resolution of triphasic waves
DISCUSSION
There are many causes for a hospitalized individual to develop encephalopathy, namely sepsis, uremia, hypoxia, toxins, metabolic disorders, hepatic failure, alcohol withdrawal, and last but not least, antibiotic-related encephalopathy. Antibiotic-associated neurotoxicity is an underrecognized etiology, in particular, the use of cefepime.[1]
Cefepime is a fourth-generation cephalosporin antibiotic, which has been used widely to treat hospital-acquired infections. Its neurotoxicity effects in patients with renal failure or normal renal function have been reported.[2345] However, only a few reports were on patients with peritoneal dialysis. According to a literature review performed by Lin et al., a total of five peritoneal dialysis patients with cefepime-induced neurotoxicity had a good outcome.[6] The exact mechanism of cefepime-related neurotoxicity is not clearly understood. Inhibition of gamma-aminobutyric acid (GABA) releases from nerve terminals, competitive inhibition of GABA binding to receptor sites, and increased excitatory amino acids are the proposed mechanisms for developing the neurotoxicity.[7] The clinical manifestations of cefepime-induced encephalopathy include nonconvulsive seizures (60%), myoclonus (33%), seizures (30%), and psychosis (3%); with a median of 4 days to develop toxicity.[8] About 55% of the patients have epileptiform discharges, while 64% demonstrate slowing and triphasic waves on the EEG.[8] Patients’ profile, such as elderly age, renal failure, and preexisting neurological disorders, increases the risk factors for developing cefepime-induced neurotoxicity, similar to in our case.
Management involves immediate withdrawal of cefepime and with or without short-term hemodialysis. CAPD is less efficient at removing cefepime compared with hemodialysis, as demonstrated in our patient. This is believed due to two main reasons, namely, the drug clearance through CAPD is less compared with hemodialysis, and the half-life of cefepime is much longer in CAPD patients. Our case is the first CAPD case reported to have benefited rapidly from a short-term hemodialysis.
Although the incidence of central nervous system adverse side-effects of cefepime is reported at 1%, clinicians should have a high index of suspicion of cefepime-induced neurotoxicity in patients, especially with high-risk factors such as renal impairment. Early recognition of this potentially reversible encephalopathy can avoid unnecessary workup, reduce length of hospital stay, and thereby reduce hospital costs and confer better treatment outcome in patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cefepime neurotoxicity in the Intensive Care Unit: A cause of severe, underappreciated encephalopathy. Crit Care. 2013;17:R264.
- [Google Scholar]
- Severe but reversible encephalopathy associated with cefepime. Neurophysiol Clin. 2000;30:383-6.
- [Google Scholar]
- Cephalosporin-induced nonconvulsive status epilepticus: Clinical and electroencephalographic features. Epilepsia. 2005;46:1550-2.
- [Google Scholar]
- Cefepime-induced encephalopathy with triphasic waves in three Asian patients. Ann Acad Med Singapore. 2007;36:450-1.
- [Google Scholar]
- Cefepime-induced encephalopathy with normal renal function. Oxf Med Case Reports. 2016;2016:118-20.
- [Google Scholar]
- Cefepime-related encephalopathy in peritoneal dialysis patients. J Chin Med Assoc. 2011;74:87-90.
- [Google Scholar]
- Relationship between structure and convulsant properties of some beta-lactam antibiotics following intracerebroventricular microinjection in rats. Antimicrob Agents Chemother. 1995;39:232-7.
- [Google Scholar]






