Translate this page into:
Oral Health Behavior and Treatment Needs among Drug Addicts and Controls in Amritsar District: A Case-controlled Study
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Substance and drug abuse is associated with severe psychosocial problems, violence and health complications.
Aims:
The aim of the study was to evaluate and compare the oral hygiene status and sugar eating patterns among drug addicts with their age, gender and socio-economic status matched controls.
Settings and Design:
The present study comprised of two groups-Group A comprised of 100 drug addicts and Group B included 100 controls. The study sample were interviewed and subjected to a comprehensive intra-oral examination.
Methods and Material:
Standardized methods of evaluation were performed using mouth mirror, dental probe, explorer and WHO probe.
Statistical Analysis:
The data was subjected to statistical analysis using Chi Square test and student t-test.
Results and Conclusions:
CPITN index revealed bleeding in 56% addicts and calculus in 20% addicts. The mean DMFT of group A was 5.71 as compared to 2.45 in group B. The frequency of sugar consumption was found to be high in addicts as compared to the controls. Significant P values (< 0.001) of DMFT index, periodontal status and frequency of sugar consumption were obtained on statistical analysis. The caries status was found to be poor in addicts, but the periodontal treatment needs were similar for both group A and B. Oral health promotion should be undertaken in drug rehabilitation centers for overall success of withdrawl treatment.
Keywords
Community periodontal index for treatment needs index
Decayed
Missing
and Filled Teeth index
drug addicts
oral hygiene status
substance abuse
substance misuse
INTRODUCTION
”Drug addiction” is a chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite harmful consequences.[1] According to a UN report, one million heroin addicts are registered in India, and unofficially, there are as many as five million.[2] In the Punjab Opioid Dependency Survey, conducted by the National Drug Dependence Treatment Centre, All India Institute of Medical Sciences, pointed out that there are about 8.6 lakh opioid users and about 2.3 lakh opioid-dependent people in Punjab alone.[3]
Substance abusers become both physically and psychologically dependent on the drug.[4] It can weaken the immune system, increasing susceptibility to infections, cause cardiovascular conditions, liver damage, seizures, and stroke. Drug abusers are at high risk of contracting infections such as HIV, viral hepatitis (hepatitis B and hepatitis C), and infective endocarditis.[5] They are susceptible to a variety of oral diseases such as generalized dental caries, periodontitis, candidiasis, xerostomia, altered taste sensation, mucosal dysplasia, oral ulceration, bruxism, leukoplakia, and oral carcinoma.[56] In addition to the direct effects of drugs on oral health, it may aggravate oral problems indirectly.[7] Poor oral hygiene, craving for sweets, neglect to seek dental care, irregular eating patterns, and poor nutrition are prevalent among addicts.[89]
To motivate the drug addicts to maintain their oral hygiene, the current status of their oral hygiene practices needs to be assessed. The aim of the study was to evaluate and compare the oral hygiene status among drug addicts with their age, gender, and socioeconomic status-matched controls. The aim of this study was also to assess their oral hygiene behavior and sugar-eating pattern.
MATERIALS AND METHODS
The case–control study comprised two groups. Group A included 100 male drug addicts who were randomly selected from a de-addiction center and voluntarily agreed to take part in the study. Females were excluded from the study as only eight of them were admitted to the de-addiction center at the time of the study. Patients with a history of only alcohol or tobacco abuse or history of systemic illness were excluded from the study. Group B (controls) comprised 100 age, gender, and socioeconomic status-matched males visiting the Oral Medicine department. Patients with a history of addiction or any systemic illness were not included in the control group. The participants ranged between 18 to 50 years.
The purpose of this study was explained to all the participants. The addicts were assured about the privacy of the personal data, and informed consents were obtained from them and their treating doctor. Data were collected by interviewing the patient personally with a validated questionnaire which included demographic data, information related to socioeconomic status, detailed history of addiction, and medical illnesses. The interview and dental examination were conducted by a trained dental student. The patient's addiction history was also confirmed from the case history file obtained from the de-addiction center. All the participants were interviewed regarding the history of oral hygiene habits and frequency of sugar consumption. History of the habit of clenching or grinding of teeth, smoking or tobacco consumption, and dryness of mouth was also obtained.
This was followed by a complete oral and dental examination. Xerostomia and attrition of teeth were noted. Standardized methods for clinical evaluation were used for caries and periodontal status. The caries status was assessed using the Decayed, Missing, and Filled Teeth (DMFT) index with a mouth mirror, dental probe, and explorer. The “D” component included carious teeth, filled teeth with recurrent decay, root stumps, and temporary fillings. The “M” component included teeth lost due to caries. The teeth lost due to trauma, congenitally missing teeth, unerupted teeth, and teeth extracted for orthodontic purposes were not scored. The “F” component described the teeth filled due to caries.
The periodontal status was recorded using the community periodontal index for treatment needs (CPITN). A WHO probe was used to record the probing measurements on the index teeth (11, 31, 16/17, 26/27, 36/37, 46/47). The tip of the probe has a 0.5-mm ball and millimeter markings at 3.5, 8.5, 11.5, and color coding at 3.5–5.5 mm and 8.5–11.5 mm. The appropriate code for each sextant was determined with respect to the following criteria:
-
Code X: When only one or no teeth are present in a sextant
-
Code 0: No sign of disease
-
Code 1: Gingival bleeding on slight provocation
-
Code 2: Presence of supra- or subgingival calculus
-
Code 3: Pathological pocket up to 5 mm
-
Code 4: Pockets more than 5mm depth.
The study groups were allocated to appropriate treatment needs (TNs):
-
TN0: No need of periodontal treatment
-
TN1: Need of improving personal oral hygiene behavior
-
TN2a: Need for scaling and improving personal oral hygiene behavior
-
TN2b: Need for scaling and root planing and improvement of personal oral hygiene behavior
-
TN3: Complex treatment (deep scaling, root planing, and more complex surgical procedures).
The subjects demonstrating only bleeding on slight provocation without the presence of apparent calculus were included in Code 1 while those with bleeding along with calculus were included in Code 2.
Statistical analysis
The collected data from both the groups were imported to Statistical Package for the Social Sciences for Windows software, version 17.0 (Chicago III). The standard descriptive methods, such as the mean, standard deviation, median, frequency, minimum and maximum, were applied to determine the characteristics of the sample. The Chi-square test was used to compare the categorical demographic variables between the two groups. Furthermore, the Student's t-test was applied to compare the mean DMFT between the two groups. Based on the mean DMFT, power analysis was done, the effect size was calculated to be 1.196, taking alpha error 0.05, power achieved was found to be 98.55%, hence justifying the sample size. The confidence interval was set to 95%, and P < 0.05 was considered statistically significant.
RESULTS
The mean age of addicts was 30.8 years, and in the control group, it was 29.8 years. The main drug of abuse was heroin and opium, and main route of drug administration was oral. Most addicts were abusing multiple drugs, and all except 16 were cigarette smokers. All the participants were from good socioeconomic background, and their education status was at least higher secondary. Table 1 shows the comparison of the oral hygiene behavior and frequency of eating sugary products between Groups A and B.
| Group A, n (%) | Group B, n (%) | P | |
|---|---|---|---|
| Oral hygiene maintenance | |||
| Oral hygiene aids | |||
| Toothbrush | 100 (100) | 100 (100) | - |
| Finger | - | - | - |
| Toothpaste | 100 (100) | 100 (100) | - |
| Toothpowder | - | - | - |
| Neem stick | - | 12 (12.0) | <0.001** |
| Mouthwash | 4 (4.0) | 4 (4.0) | 1.000 (Ns) |
| Floss | 12 (12.0) | - | <0.001** |
| How often | |||
| Once a day | 80 (80.0) | 80 (80.0) | 1.000 (Ns) |
| >Once a day | 20 (20.0) | 20 (20.0) | |
| Clean tongue | |||
| Yes | 72 (72.0) | 76 (76.0) | 0.519 (Ns) |
| No | 28 (28.0) | 24 (24.0) | |
| Change toothbrush | |||
| 3 Months | 60 (60.0) | 60 (60.0) | 0.030* |
| 6 Months | 12 (12.0) | 16 (16.0) | |
| >1 Year | 28 (28.0) | 24 (24.0) | |
| Sugar consumption | |||
| Frequency of eating sugary products | |||
| 1-4 Times a week | 0 (0) | 64 (64) | <0.001** |
| Once or twice a day | 12 (12.0) | 32 (32.0) | |
| 3-4 Times a day | 40 (40.0) | 4 (4.0) | |
| >5 Times a day | 48 (48.0) | 0 (0) | |
| Periodontal status | |||
| Noticed smell | |||
| Yes | 44 (44.0) | 24 (24.0) | <0.001** |
| No | 56 (56.0) | 76 (76.0) | |
| Noticed bleeding | |||
| Yes | 64 (64.0) | 12 (12.0) | <0.001** |
| No | 36 (36.0) | 88 (88.0) | |
| Access to dental care | |||
| Last time visited dentist | |||
| Within 1 year | 52 (52.0) | 60 (60.0) | <0.001** |
| 1-2 Years | 4 (4.0) | 16 (16.0) | |
| >2 Years | 16 (16.0) | 4 (4.0) | |
| Never | 28 (28.0) | 20 (20.0) |
*Significant, **highly significant. Ns: Not significant
Oral hygiene maintenance
Patients in both groups were using toothbrush and toothpaste, out of which 80% were using it once daily and 20% more than once a day. In addition, mouthwash was used by four patients in each group. Twelve patients in Groups A and B used floss and neem stick, respectively, as an additional oral hygiene aid. Twenty-eight percent of the drug addicts even reported using the same toothbrush for more than 1 year. Although all Group A addicts were using toothbrush at least once daily and some were using floss and mouthwash additionally, they had poor oral hygiene.
Frequency of eating sugary products
There was an increased tendency of eating sugary products among the drug addicts. Eighty-eight percent of the addicts were consuming sugar products more than three times per day as compared to 4% in Group B. This was statistically highly significant (P < 0.001). One patient from Group A even reported of consuming 15–20 candies at a time after every drug dose [Figure 1].
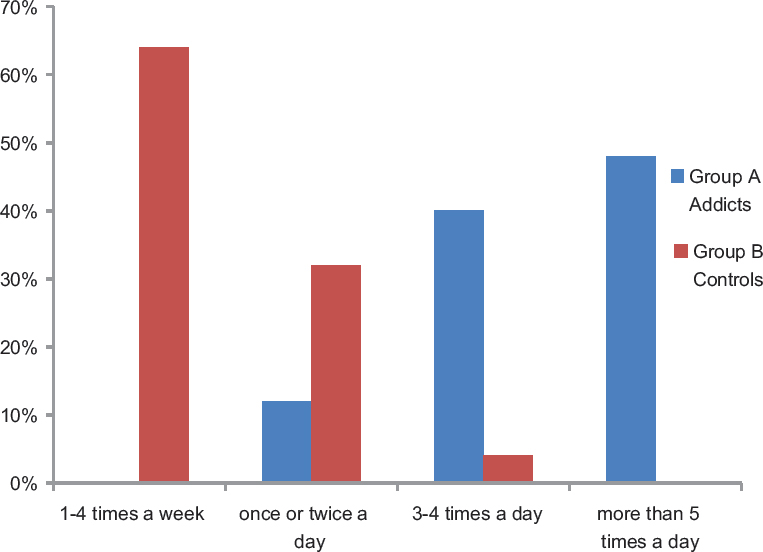
- Frequency of eating sugary products in Group A (addicts) and Group B (controls)
Periodontal status
Forty-four percent in Group A and 24% in Group B gave a history of halitosis while 64% in Group A and 12% in Group B noticed bleeding from gums. This was also statistically highly significant (P < 0.001) [Figure 2].

- Foul smell and bleeding from gums as noticed by Group A and Group B
CPITN index was performed for the evaluation of periodontal status. None of the patients in Group A demonstrated healthy gingiva, in comparison to 24% of patients in Group B. Fifty-six percent of patients in Group A and 32% in Group B demonstrated bleeding on slight provocation of the gingiva. These findings are an indicator that all the patients in Group A and 76% in Group B required change in oral hygiene behavior (TN1) and 44% of patients in both Groups A and B required improvement in oral hygiene habits and oral prophylaxis (TN2a) [Table 2].
| Code | Identification | Group A (addicts) | Addicts percentage prevalence | Group B (controls) | Controls percentage prevalence |
|---|---|---|---|---|---|
| 0 | H | 0 | 0 | 24 | 24 |
| 1 | B | 56 | 56 | 32 | 32 |
| 2 | C | 20 | 20 | 44 | 44 |
| 3 | P1 | 24 | 24 | 0 | 0 |
| 4 | P2 | 0 | 0 | 0 | 0 |
| TN code | Addicts (%) | Controls (%) | |||
| Percentage TN1 (B + C + P1 + P2) | 100 | 76 | |||
| Percentage TN2 | 44 | 44 | |||
| Percentage TN3 | 0 | 0 | |||
TN0: No need for periodontal treatment, TN1: Need for improvement of personal oral hygiene, TN2a: Need for scaling and improving personal oral hygiene behavior, TN2b: Need for scaling and root planing and improvement of personal oral hygiene behavior, TN3: Complex treatment involving deep scaling, root planing, and more complex surgical procedures
Caries index
The DMFT index was performed to assess the caries status between the two groups. The mean DMFT of Group A was 5.71 as compared to 2.45 in Group B. This was statistically highly significant (P < 0.001). The mean difference between the DMFT of both the groups was 3.26 [Table 3].
| Group | n | Range | Mean | SD | Mean difference | t# | P# |
|---|---|---|---|---|---|---|---|
| A (Drug Addicts) | 100 | 0-14 | 5.71 | 3.748 | 3.260 | 8.246 | <0.001** |
| B (Controls) | 100 | 0-5 | 2.45 | 1.258 |
#Student’s t-test: **P<0.001; Highly significant. SD: Standard deviation
Access to dental care
Twenty-eight percent drug addicts reported that they had never visited a dentist and 16% had not visited within the past 2 years. Although 52% of drug addicts had visited the dentist in the past 1 year, they had poor oral hygiene.
DISCUSSION
The oral health practices among drug addicts are neglected and have been addressed insufficiently.[10] There is limited information concerning the circumvention of oral disorders in alcoholics and drug abusers in India. Our study between drug abusers and controls represents the oral hygiene practices and objective assessment of caries and periodontal status among the Indian population. The oral health status and the attitude of drug addicts toward oral health were found to be poor in our study.
The drug addicts included in the study sample reported high levels of oral disease which can be attributed to improper oral hygiene practices and negligence. Although the patients were using toothpaste and toothbrush as the main oral hygiene aid, only 20% were following the recommended twice daily regime. In addition, 12 patients of Group A reportedly used floss and four used mouthwash. These findings were contradictory to what has been observed in earlier studies conducted by Shekarchizadeh et al.,[7] Sheridan et al.,[9] Molendijk et al.,[11] and Morio et al.[8] All of them found a decreased frequency of brushing in addicts and only handful of them practiced proximal cleaning.
Another study conducted by Barbadoro et al.[12] involving Italian alcohol-addicted patients reported the frequency of brushing twice daily or more in 54% of addicts, which was much higher than our finding.
The patients in the rehabilitation center were from sound socioeconomic background; hence, they could afford the drugs and were aware of various additional oral hygiene aids. Sixty percent of the addicts changed their toothbrush within 3 months while 28% of them used the same toothbrush for more than a year.
A study conducted by Shekarchizadeh et al.[7] in 2013 revealed that 73% of the addicts consumed sugary products once daily or more often. Our study revealed that the frequency of sugar consumption among addicts was found to be much higher. Eighty-eight percent of the addicts consumed sugary products more than three times a day. It was in the form of carbonated drinks, candies, and table sugar. The addicts gave a history of sugar craving, especially immediately after the drug use. This high frequency of sugar consumption among the drug addicts could be attributed to a high DMFT index among them.
In Group A, 64% and 12% of patients from Group B reported bleeding from gums. Although there was little difference in regard to brushing frequency, significant statistical value was found in the addicts (P < 0.001).
The drug addicts in our study brushed their teeth at least once daily as compared to other studies in which the addicts reported less frequent cleaning of teeth.[789] This further strengthens and reinforces the fact that opioids can cause immunosuppressant effects and alter the microbial profile leading to periodontal disease.[51314]
The results of the study conducted by Singh et al.[4] showed the presence of calculus in 48% of patients, 61% had bleeding on probing, and 59% had shallow periodontal pockets among drug addicts under withdrawal treatment in Punjab. The results obtained in our study are similar to the above findings; calculus being present in 20% addicts, 58% had bleeding on probing, and 24% had pockets <5 mm. Khocht et al.,[15] in their study, on alcoholics, stated that they were unable to practice basic dental hygiene adequately because of impaired motor activity. Bleeding, shallow pockets, and deep pockets were found as the highest Community Periodontal Index finding in 42%, 44%, and 12% of drug users, respectively, in a study conducted by Gupta et al.[16] Thus, impaired motor activity among drug addicts could also be attributed to poor oral hygiene.
Alcohol dependence and substance abuse are associated with increased risk of caries and periodontitis.[1117] Our study also showed that drug addicts had more decayed teeth as compared to controls. The mean DMFT was found to be 5.71 in drug addicts as compared to 2.45 in controls. The caries index was found to be high among the drug abusers as quoted by Gupta et al.[16] (mean DMFT in addicts: 3.34), Singh et al.,[4] and Reece.[18] High rates of generalized caries, particularly on smooth and cervical surfaces of teeth, have been associated with opioid use and can be attributed to improper eating patterns, general personal neglect, cravings for sweet food, and xerostomia induced by the drug.[5192021]
As stated by Sheridan et al.,[9] poor access to dental treatment is the main cause of the greater level of oral problems in drug users. Fifty-two percent of the drug addicts in our study had visited the dentist within 1 year, and 28% had never visited a dentist. The low attendance of the addicts in dental clinics could be attributed to the analgesic and mental detachment effects of drugs and the dental care being sought only for extreme pain.[2223] Scheutz stated that heightened dental fear and low self-esteem could be another reason for reduced dental visits.[24]
CONCLUSION
The present study is a comparative one between the drug abusers and controls of the same age group to relate the onset and severity of dental problems. It has been noted in previous studies that the results have been formulated solely on the basis of patient interviews.[6915] Our study design is both subjective and objective, as both interview and dental examination were performed. Moreover, standardized and universally recognized dental indices were recorded. In most earlier studies, the authors have used scoring criteria which are not universally used.[718] This study design can also be used for larger sample sizes efficiently.
In this study, high DMFT and CPITN scores were found in drug addicts as compared to controls. Irregular eating patterns, craving for sugary substances after drug intake, irregular dental visits, and failure to show up for appointments were found to be the contributing factors for poor oral hygiene among the addicts. Sugar consumption in addicts was found to be very high, explaining the high DMFT scores. Although the caries status was found to be poor in addicts, the periodontal TNs were similar in both the groups.
The drug rehab facilities can help in changing the patient's perception of oral hygiene practices and this, in turn, adds to the success of withdrawal treatment.[7] In addition to general health promotion, various oral health promotion programs should be undertaken in such settings, as it assists them in constructing a nonaddict identity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors are grateful to Bhatia De-addiction Center, Amritsar and Mr. Gurinder Singh for statistical analysis.
REFERENCES
- NIDA. Media Guide. National Institute on Drug Abuse Website. Available from: https://www.drugabuse.gov/publications/media-guide
- [Google Scholar]
- Punjab Opioid Dependence Survey: Brief Report. Available from: http://www.pbhealth.gov.in/scan0003%20(2).pdf
- Evaluation of oral health status among drug addicts in rehabilitation centre. IAIM. 2016;3:65-9.
- [Google Scholar]
- Drug users: Oral health-related attitudes and behaviours. Br Dent J. 2005;198:219-24.
- [Google Scholar]
- Oral health behavior of drug addicts in withdrawal treatment. BMC Oral Health. 2013;13:11.
- [Google Scholar]
- Comparing diet, oral hygiene and caries status of adult methamphetamine users and nonusers: A pilot study. J Am Dent Assoc. 2008;139:171-6.
- [Google Scholar]
- Dental health and access to dental treatment: A comparison of drug users and non-drug users attending community pharmacies. Br Dent J. 2001;191:453-7.
- [Google Scholar]
- Improvement of knowledge, attitude, and behavior about oral health in a population of alcohol addicted persons. Alcohol Alcohol. 2008;43:347-50.
- [Google Scholar]
- AIDS, drugs of abuse and the immune system: A complex immunotoxicological network. Arch Toxicol. 1991;65:609-17.
- [Google Scholar]
- Opioids, opioid receptors, and the immune response. Drug Alcohol Depend. 2001;62:111-23.
- [Google Scholar]
- Dental care and oral disease in alcohol-dependent persons. J Subst Abuse Treat. 2009;37:214-8.
- [Google Scholar]
- Oral health status of a group of illicit drug users in Delhi, India. Community Dent Health. 2012;29:49-54.
- [Google Scholar]
- Five-year evaluation of a dental care delivery system for drug addicts in Denmark. Community Dent Oral Epidemiol. 1984;12:29-34.
- [Google Scholar]
- Dentition of addiction in Queensland: Poor dental status and major contributing drugs. Aust Dent J. 2007;52:144-9.
- [Google Scholar]
- High sugar intake in a group of women on methadone maintenance in South Western Sydney, Australia. Addiction. 1996;91:1053-61.
- [Google Scholar]
- Diet and opiate addiction: A quantitative assessment of the diet of non-institutionalized opiate addicts. Br J Addict. 1989;84:173-80.
- [Google Scholar]
- Anxiety and dental fear in a group of parenteral drug addicts. Scand J Dent Res. 1986;94:241-7.
- [Google Scholar]






