Translate this page into:
Surgical Experience in Pediatric Patients with Chiari-I Malformations Aged ≤18 Years
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The objective of this study was to retrospectively study Chiari I malformation patients (<18 years) treated surgically.
Materials and Methods:
Chiari I malformation patients (<18 years) treated surgically at our institute were retrospectively studied.
Results:
During the study period between January 1999 and June 2011, fifty patients, aged ≤18 years with Chiari malformation, were treated surgically and formed the basis for this series. There were 21 female children (42%) and 29 male children (58%), with a female-to-male ratio of 1:1. At the last follow-up, oropharyngeal symptoms were improved in 33% (n = 3/9). Headache/neck/back pain improved in 69.56% of children (n = 16/23). Upper-extremity pain/weakness/numbness improved in 73.91% of children (n = 17/23). Ataxia improved in 66.66% of children (n = 4/6). Lower-limb weakness/hyperreflexia improved in 83.33% of children (n = 5/6). At follow-up, magnetic resonance imaging for patients with syrinx was available for 75% of patients (n = 30/50) and not available for 25% of patients (n = 10/40). Syrinx was diminished in size or resolved in 66.33% of patients (n = 19/30) and the remaining was same for 36.66% of patients (n = 11/30).
Conclusions:
The main goal of surgery is to arrest the progression of neurological deficits. Foramen magnum decompression with a lax duroplasty is the surgical procedure of choice.
Keywords
Chiari malformation
duroplasty
pediatric
INTRODUCTION
Chiari malformation Type I is identified by the caudal descent of the cerebellar tonsils which may or may not be associated with the presence of a syrinx; a degree of medullary descent and buckling of the lower medulla may also be present. In pediatric Chiari I malformation, female-to-male ratio has been variably reported as 1.5:1–1:1.5.[123] The average age among the pediatric patients is 11 years (range 1–19 years). Headache (40%–60%) is the common symptom of pediatric Chiari I malformation patients.[12345] It is reported as a heavy, crushing, or pressure-like sensation at the back of the head that radiates to the vertex, behind the eyes, and to the neck and shoulders which is accentuated by physical exertion and by Valsalva maneuvers (e.g., coughing, sneezing, or vomiting). Many patients also experience visual disturbances, such as blurring of vision, sensitivity to light, double vision, and visual-field deficits. Nearly 10%–21% of patients report a lower cranial nerve palsy.[6] Syrinx reported in pediatric Chiari I malformation ranges from 51% to 58%.[135] Patients with syringomyelia suffer with motor deficits more frequently than those without syringomyelia (ratio 7:1). Sensory symptoms are also more frequent in this group (ratio 4:1).[3] Associated diagnoses with pediatric Chiari I malformation reported are hydrocephalus (11%), neurofibromatosis Type 1 (5.5%), Sprengel's deformity (2.7%), idiopathic growth hormone deficiency (5.5%), basilar invagination (4%), and Klippel–Feil anomaly (5%).[15] Magnetic resonance imaging (MRI) is regarded very important for establishing the diagnosis and is helpful for identifying other related anomalies. Dynamic MRI also helps confirm abnormalities in cerebrospinal fluid (CSF) flow at the foramen magnum and the benefits of decompressive surgery in patients with the Chiari I malformation.[7] Ultrasonography is another useful study to identify the CSF circulation during surgery.
Objectives
The objective of this study was to retrospectively study the Chiari I malformation patients (<18 years) treated surgically.
MATERIALS AND METHODS
Charts of all patients who were surgically treated at the Department of Neurosurgery, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, Kerala, India, with the diagnosis of Chiari type I malformation with age ≤18 years were reviewed retrospectively from January 1999 to June 2011. Data were collected on patient age, sex, clinical symptoms and signs (oropharyngeal dysfunction, headache, scoliosis, motor symptoms, sensory symptoms, gait ataxia, and lower cranial nerve palsy) at the time of admission, MRI features including tonsillar descent, syrinx, and scoliosis, surgery (foramen magnum decompression, foramen magnum decompression with lax duroplasty, foramen magnum decompression with lax duroplasty and tonsillar resection, and any other surgery), and postoperative neurological complications (lower cranial nerve palsy, tracheostomy, elective ventilation, and wound infection). Patients’ condition was evaluated at 6 weeks and 6, 12, and 24 months after discharge and at last follow-up.
RESULTS
The results obtained from the study were expressed in the following section in tabular format. Numerical, continuous data were expressed with mean.
Demographics
During the study period between January 1999 and June 2011, fifty patients, aged ≤18 years with Chiari malformation, were treated surgically and formed the basis for this series. There were 21 female children (42%) and 29 male children (58%), with female-to-male ratio of 1:1. The average age of the patients was found to be 13.85 years, (range of 1.5–18 years). Regarding age and sex distribution, there were three patients <5 years of age, 7 patients between 6 and 10 years of age, 19 patients between 11 and 15 years, and 21 patients between 16 and 18 years of age.
Clinical characteristics
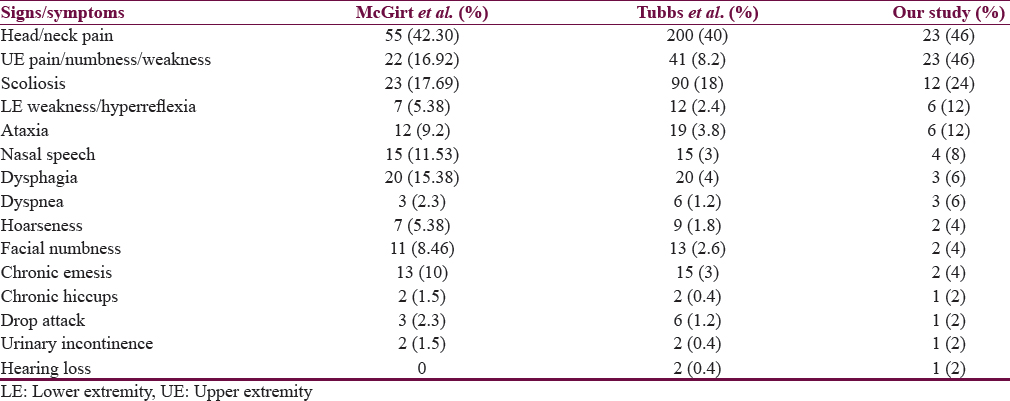
Clinical characteristics included the following: ataxia (6 [12%]), nasal speech (4 [8%]), dysphagia (3 [6%]), dyspnea (3 [6%]), hoarseness (2 [4%]), facial numbness (2 [4%]), chronic emesis (2 [4%]), chronic hiccups (1 [2%]), drop attack (1 [2%]), urinary incontinence (1 [2%]), and hearing loss (1 [2%]).
Magnetic resonance imaging
Syrinx was present in 80% of patients (n = 40). Most commonly involved segment in syrinx was cervico-dorsal in 77.50% (n = 31), only cervical in 17.50% (n = 7), only thoracic segment in 2.5% (n = 1), holocord syrinx in 2.8% of patients (n = 1). Scoliosis was present in 24% of patients (n = 12). Scoliosis was more common toward the right side (58.33% [n = 7]) and toward the left side (41.67% [n = 5]). Scoliosis was observed more commonly in male patients (66.66% [n = 14]) compared to female patients (33.33% [n = 7]). Scoliosis most commonly involved cervicodorsal region (75% [n = 8]), followed by cervical and thoracic region equally (12.50% [n = 2]) each.
Surgical procedure
Of the fifty patients with Chiari I malformation, 94% of patients (n = 47) aged ≤18 years underwent foramen magnum decompression with lax duroplasty, 2.0% of patients (n = 1) were treated with foramen magnum decompression with lax duroplasty and tonsillar resection (left tonsil was gliotic), 2.0% of patients (n = 1) were treated with foramen magnum decompression with lax duroplasty with C2–C3 posterior fusion (subluxation of C2–C3), and 2.0% of patients (n = 1) were treated with foramen magnum decompression with lax duroplasty with occipitocervical fusion with contour rod (reducible atlantoaxial dislocation). Indication of tonsillar resection was gliotic during intraoperative left tonsil and more elongated. Indication for C2–C3 posterior fusion was subluxation of C2–C3 and indication for occipitocervical fusion was reducible atlantoaxial dislocation.
Complications
Out of the fifty patients, tracheostomy was done in three patients, in two patients due to lower cranial nerve paresis, and in one patient for elective ventilation due to poor respiratory reserve preoperatively. All the three patients were referred to ENT surgeon for evaluation and decannulation of tracheostomy. All the three patients were doing well at 6-week follow-up. None of the patients developed wound infection. One patient developed left posterior inferior cerebellar artery territory infarct which was managed with anti-edema measures; one patient developed intermittent diplopia in postoperative period. Three patients developed fever which was managed with antibiotics (no CSF study was done).
Outcomes
-
At 6-week follow-up, there was no improvement in 28% (n = 14) of the total population. Oropharyngeal symptoms were improved in 33% of patients (n = 3/9). Headache/neck ache/back pain improved in 56.52% of patients (n = 13/23). Upper-extremity (UE) pain/weakness/numbness improved in 78.26% of patients (n = 18/23). Ataxia improved in 66.66% of patients (n = 4/6). Lower-limb weakness/hyperreflexia improved in 66.66% of patients (n = 4/6). Nearly 4% of patients (n = 2) developed intermittent diplopia at 6-week follow-up
-
At 6-month follow-up, headache/neck ache/back pain improved in five more patients, at 6 months, headache/neck ache/back pain improved in 78.26% of patients (n = 18/23). UE pain/weakness/numbness improved in three more patients, at 6 months, it improved in 91.30% of patients (21/23). Two patients with persistent lower cranial nerve dysfunction at 6 months lost to follow-up. No other symptoms were improved
-
At 12-month follow-up, a total of three patients were lost to follow-up and in one patient, lower-limb spasticity improved, at 12 months, in 83.33% of patients (n = 5/6), lower-limb weakness/hyperreflexia improved. One patient developed headache which was relieved earlier (managed on conservative treatment)
-
At 24-month follow-up, eight patients were operated before 2 years. Four patients were lost to follow-up. Four patients developed new upper-limb pain/weakness/numbness. One patient reported improvement in headache. At 24 months, 82.60% of patients (n = 19/23) reported improvement in headache
-
At the last follow-up, mean duration of follow-up was 45.52 months (minimum – 3 months, maximum – 155 months). At the time of last follow-up, seven patients were having no improvement of symptoms and four patients developed new symptoms of upper-limb pain/weakness/numbness. Two patients were referred to an orthopedician for scoliosis surgery. One patient was referred to a psychiatrist for multiple somatic complaints. At the last follow-up, oropharyngeal symptoms were improved in 33% of patients (n = 3/9). Headache/neck ache/back pain improved in 69.56% of patients (n = 16/23). UE pain/weakness/numbness improved in 73.91% of patients (n = 17/23). Ataxia improved in 66.66% of patients (n = 4/6)
-
Lower-limb weakness/hyperreflexia improved in 83.33% of patients (n = 5/6). At follow-up, MRI for patients with syrinx was available for 75% of patients (n = 30/50) and not available for 25% of patients (n = 10/40). Syrinx was diminished in size or resolved in 66.33% of patients (n = 19/30) and the remaining was same for 36.66% of patients (n = 11/30).
DISCUSSION
Clinical characteristics
In the present study, 46% of patients (n = 23/50) presented with headache/neck pain. In a series by Tubbs et al., headache/neck pain was the presentation in 40% of patients (n = 200/500). In a study by McGirt et al., 42.30% of patients (n = 55/130) presented with headache/neck pain. In a study by Menezes et al. on pediatric group, ≈40% of children had pain at presentation. In our study, the upper-limb pain/numbness/weakness was the presentation in 46% of patients (n = 23/50). In a series by Tubbs et al., upper-limb pain/numbness/weakness was present in 8.2% of patients (n = 41/500). In a study by McGirt et al., 16.92% of patients (22/130) presented with upper-limb pain/numbness/weakness. In a study by Menezes et al. on pediatric group, ≈80% of children had motor signs/symptoms. In our study, 24% of patients (n = 12/50) had scoliosis. In a series by Tubbs et al., scoliosis was present in 18% of patients (n = 90/500). In a study by McGirt et al., 17.69% of patients (n = 23/130) had scoliosis. In a study by Menezes et al. on pediatric group, scoliosis was present in ≈50% of patients [Table 1]. The management strategy follows a “top down” rule.[4689] If there is hydrocephalus, it is dealt first by CSF diversion procedure. If it does not ameliorate the symptoms, then foramen magnum decompression with a lax duroplasty is done to deal with the impaction of tonsils into the upper cervical canal. It opens the subarachnoid pathways.
CONCLUSIONS
Patients with a symptomatic Chiari malformation and/or a distended syrinx cavity should be candidates for surgery. The main goal of surgery is to arrest the progression of neurological deficits. Foramen magnum decompression with a lax duroplasty is the surgical procedure of choice.
In selected patients with milder symptoms, the trend toward earlier operation appears to improve long-term neurological outcomes. It is important to decompress the posterior fossa in the midline and to open the dura and explore for patency of the foramen of Magendie to ensure that there is CSF egress.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Institutional experience with 500 cases of surgically treated pediatric Chiari malformation type I. J Neurosurg Pediatr. 2011;7:248-56.
- [Google Scholar]
- Chiari malformation type I in children younger than age 6 years: Presentation and surgical outcome. J Neurosurg Pediatr. 2010;5:554-61.
- [Google Scholar]
- Treatment of Chiari I malformation in patients with and without syringomyelia: A consecutive series of 66 cases. Neurosurg Focus. 2001;11:E3.
- [Google Scholar]
- Symptomatic Chiari malformations. An analysis of presentation, management, and long-term outcome. J Neurosurg. 1989;71:159-68.
- [Google Scholar]
- Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg. 2003;99:291-6.
- [Google Scholar]
- Surgical Treatment of Hydromyelia. Delhi: CME Programme, NSI; 1982. p. :181-95.
- Cerebrospinal fluid flow waveforms: Analysis in patients with Chiari I malformation by means of gated phase-contrast MR imaging velocity measurements. Radiology. 1995;196:195-202.
- [Google Scholar]
- Symptomatic Chiari malformation in adults: A new classification based on magnetic resonance imaging with clinical and prognostic significance. Neurosurgery. 1991;28:639-45.
- [Google Scholar]
- Neural anomalies at the craniovertebral junction and their management. Prog Clin Neurosci. 1989;4:257-75.
- [Google Scholar]






