Translate this page into:
Clinical Spectrum of Central Nervous System Tuberculosis and the Efficacy of Revised National Tuberculosis Control Program in its Management
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Tuberculosis (TB) is a major global problem and poses a threat which is of considerable magnitude, with an estimated one-third of the population infected with TB bacillus.
Aim:
The aim of this study is to study the treatment outcomes in patients with various forms of neurological TB treated with the standardized Revised National TB Control Program (RNTCP), directly observed treatment short-course (DOTS).
Materials and Methods:
Patients diagnosed to have TBM, tuberculoma with or without spinal arachnoiditis (central nervous system tuberculosis-TB [CNS-TB]) were categorized as per the RNTCP guidelines and received DOTS Category I or Category II thrice-weekly intermittent treatment as deemed appropriate.
Results:
The outcome of management with the standard RNTCP DOTS regimen was that a success rate (treatment completed) of 75%, the default rate of 6.6%, and a mortality of 3.3%. The target fixed by the RNTCP is to achieve a cure rate of 85%. We were able to document successful completion of treatment in 75% which is close to the target fixed by RNTCP. The default rate is 6.6% which quite negligible when compared to the unsupervised therapy which has a default rate of 50%.
Conclusion:
The most important factor in predicting the outcome of treatment in CNS-TB is early diagnosis and the timing of initiation of antituberculous treatment. Early initiation of treatment is associated with better treatment outcomes.
Keywords
Directly observed therapy central nervous system tuberculosis
intermittent regimen
tuberculosis
tuberculous meningitis
INTRODUCTION
Tuberculosis (TB) is a major global problem and poses a threat which is of considerable magnitude, with an estimated one-third (over 2 billion) of the population[1] infected with TB bacillus. Annually about 8 million individuals around the world develop TB, and 70,000 of these patients acquire TB meningitis. In immunocompetent individuals, CNS-TB accounts for about 1% of all cases of TB and 6% of extrapulmonary TB.[2]
The incidence of TB infection in general population will reflect the incidence of CNS-TB as they are directly proportional. About 10% of all patients with TB have been estimated to have CNS involvement.[3] The various manifestations of CNS-TB are included under three major clinical categories: chronic tuberculous meningitis (TBM), tuberculoma brain, spinal tuberculous arachnoiditis. The existing effective treatment regimens have a case fatality ratio remains high at 15%–40%.[4] The emergence of multiple drug resistance TB and human immunodeficiency virus (HIV) coinfection has further complicated this issue.
The Revised National TB Control Programme (RNTCP) of the Government of India based on the internationally recommended “directly observed treatment short-course” (DOTS) strategy was launched in 1997. Since then, it has emerged as the standard of care for patients with TB in India. The entire country (over a billion population, in 632 districts/reporting units) was covered by March 2006 by the RNTCP. In India, more than 11 million patients have been treated since the inception of the RNTCP.[4]
Data regarding the efficacy of the RNTCP treatment regimens in patients with CNS-TB in the field setting is sparse. Documenting the effectiveness of these standardized treatment regimens in patients with neurological TB will be a valuable addition to the available evidence.
Aim
The aim of this study is to study the treatment outcomes in patients with various forms of CNS-TB treated with the standardized RNTCP DOTS treatment.
MATERIALS AND METHODS
All patients diagnosed to have CNS-TB in the Outpatient Departments of Neurology and Medicine including intensive care wards of the same. At the Rajiv Gandhi Government general Hospital, Chennai, Tamil Nadu, was prospectively studied. The patients included in the study were those diagnosed to have TBM, tuberculoma with or without spinal arachnoiditis. The patients who were excluded were hypersensitivity to anti-TB drugs, presence of secondary immunodeficiency states, such as HIV infection, organ transplantation, malignancy, currently receiving cytotoxic therapy, or have received it within the last 3 months, pregnancy and lactation, patients with cardiac disease, impaired renal functions (estimated glomerular filtration rate <60 ml/min/1.73 m2 L, liver diseases, serum bilirubin >1.5 mg/dl, and serum transaminases, alkaline phosphatase more than 1.5 times the upper limit of normal), patients with positive viral markers for hepatitis A, B, C, and E viruses, patient with hematological abnormalities (total leukocyte count ≤3000/mm3; platelet count less ≤100,000/mm3, patient with history of alcoholism or drug abuse, and patients unwilling to participate in the study. Informed consent was obtained from all the patients for participation in the study. In all of them, a detailed history was taken, and a thorough physical examination was done. Baseline hemogram was done to rule out hematological abnormalities. Serum bilirubin, serum aspartate aminotransferase, serum alanine aminotransferase, and serum alkaline phosphatase were tested at baseline to rule out abnormal hepatic functions.
In all patients, lumbar puncture was performed, and the cerebrospinal fluid (CSF) total count, lymphocyte count, protein, and sugar levels were estimated at the time of initial evaluation.
At the time of initial evaluation, plain and contrast-enhanced computed tomography of the brain was done in all patients, and 1.5-tesla magnetic resonance imaging (MRI) (plain and contrast) was done in selected patients with CNS-TB. During the follow-up visits, imaging investigations were repeated when clinically indicated. All patients with CNS-TB were categorized as per the RNTCP guidelines and received DOTS Category I or Category II thrice-weekly intermittent treatment as deemed appropriate. New patients with CNS-TB treated under.
Drug regimen Category 1:2 (H, R, E, Z)3//4 (HR)3 with the extension of continuation phase for 3 months (total 9 months).
-
H - Isoniazid 300 mg
-
R - Rifampicin 450 mg
-
E - Ethambutol 1200 mg
-
Z - Pyrazinamide 1500 mg
-
S - Streptomycin 750 mg.
Prefix denotes the number of months and the suffix the number of doses per week). The first 2 months of treatment was the intensive phase followed by the continuation phase for 7 months. The continuation phase of treatment was further extended in selected patients as per the need. Previously treated patients, treatment after interruption, defaulters, were treated with Category II regimen 2 (HRZES)3 +1 (HRZE)3 +5 (HRE)3 with the extension of continuation phase for 3 months. The continuation phase of treatment was further extended in selected patients as per the need. The treatment outcomes were defined as per the RNTCP guidelines as “treatment success” (defined as a patient who has either been cured or has completed treatment) and “default” (patients whose treatment was interrupted for two consecutive months or more). New cases who manifested clinical, radiological, and bacteriological deterioration in spite of 5 months of adequate treatment were termed as “treatment failure.”
RESULTS
A total of 72 patients diagnosed to have neuro-TB were evaluated. Of the 72 patients, 60 patients who satisfied the inclusion criteria were recruited for the study after obtaining consent, and they were followed up. Twelve patients were excluded from the study due to other associated comorbidities such as cardiac illness, renal, hepatic illness, immunocompromised state, and hematological abnormalities. The age distribution of patients enrolled in the study is shown in Table 1. The age group of the enrolled patients was in the range of 14–59. The mean age was 28 years, with 27 patients (45%) in 20–29 age group. Overall CNS-TB has male preponderance with a ratio of male/female 1.86:1. The various forms of presentation of CNS-TB are shown below in Table 1.
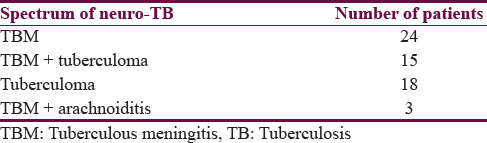
Of the varied manifestations of CNS-TB, 24 patients had TBM (40%), and 15 patients had tuberculoma with TBM. The common symptoms of presentation in patients with TBM in our study were headache and fever which are the cardinal symptoms for the diagnosis of TBM. The common signs included altered sensorium, seizures, focal deficits in the form of hemiparesis, and cranial nerve palsy. A total of 10 patients with TBM with and without tuberculoma had papilledema. Tuberculoma (18 patients - 30%) ranks second next to TBM among the spectrum CNS-TB. The common presenting signs and symptoms of tuberculoma were seizures followed by headache, fever, and focal deficits. The common presentation in patients with TBM and tuberculoma is the headache, fever, altered sensorium, seizures, and focal deficit. Three cases of TBM with spinal arachnoiditis (presented with features of basal menigitis and arachnoiditis) were enrolled. The clinical manifestations of the patients were fever, headache, and seizures. Physical examination revealed neck stiffness, optic atrophy, bilateral VI cranial nerve palsy, and paraplegia.
The patients with TBM were staged according to MRC staging. The British Medical Research council distinguishes three clinical stages of TBM based on three parameters.
-
Level of consciousness
-
Focal neurological deficits
-
Presence of seizures, meningism, and behavioral changes.
The clinical staging on admission in 42 patients is shown in Table 2.

The CSF examination findings in 42 patients with TB meningitis are shown in Table 3. In none of the patients, we were able to document TB bacilli in the CSF.

CSF TB PCR, gene Xpert were not done in our patients due to logistical reason. The CSF opening pressure measurement was not done. Presence meningeal enhancement was the most common imaging finding in 20 patients (83.33%) of the patients with isolated TBM. Followed by hydrocephalus in 16 patients (66.66%), basal exudates in 9 (37.5%), and infarcts in 4 patients (16.6%). In patients with TBM with tuberculoma, the most common abnormality was the meningeal enhancement in 8 patients (53.33%) followed by basal enhancement in 6 (40%), hydrocephalus in 3 (20%), and infarcts in 3 (20%). In patients with TBM and spinal arachnoiditis, all the three patients had hydrocephalus, meningeal enhancement, and basal exudates [Table 4]. The complications encountered are listed in Table 5.


Among 18 cases of tuberculoma, 12 cases had solitary lesions, and 6 cases had multiple lesions. In patients who presented with TBM and tuberculoma (n = 15), multiple tuberculoma was seen in 12 cases and solitary lesions in 3 cases.
Brain biopsy was not done in our patients. The diagnosis was more a clinicoradiological diagnosis.
All the 60 patients enrolled in this study were new cases of TB and hence entitled to receive Category I Anti-tuberculous therapy (ATT) and steroids according to the prescribed protocol.
Among the 60 patients followed up, 6 patients lost to follow-up (four cases of TBM ± tuberculoma ± arachnoiditis and two cases of isolated tuberculoma), and four cases defaulted drugs (two cases of TBM and two cases of tuberculoma). Among the 50 patients who were regularly followed up, six patients’ level of sensorium worsened (two patients progressively worsened since admission). Subsequent imaging in these patients showed worsening of the grade of hydrocephalus for which VP shunt was done in five patients. On subsequent follow-up, these patients developed shunt dysfunction, shunt infection, increase in the size of the tuberculoma and two patients out of five succumbed to death in the 3rd month of treatment. In addition, these patients required anti-edema measures. Two patients showed improvement, and they required 12 months of ATT, and they finally completed treatment successfully. In one patient, there was tuberculous abscess formation, and drainage of the abscess was done through a frontal burr hole. Later, this patient developed bilateral hemorrhagic infarct due to cerebral venous sinus thrombosis at the 7th month of ATT, communicating hydrocephalus with features of raised intracranial pressure. Finally, this patient was considered to be a treatment failure case given occurrence clinical and radiological worsening after 7 months of ATT. In 18 cases of tuberculoma, 12 were solitary lesions, and a minimal regression of the lesions was noted. In six cases with multiple lesions, two cases defaulted treatment, two cases lost to follow- up, and in the remaining two patients there was a worsening of symptoms with increasing frequency of seizures and imaging showed an increase in the size of lesions and occurrence of new lesions. These cases were given 12 months of ATT. These cases were labeled as treatment failure.
Two patients (3.3%) in our study developed anti-TB drug-induced hepatotoxicity. The first-line drugs were stopped, and the patient was treated with ethambutol till the liver functions normalized. The first-line drugs could be successfully reintroduced in both the patients.
Patients who presented with isolated tuberculoma (n = 18) 12 had solitary, and six had multiple lesions. Among the 14 patients who completed follow-up showed two developed new lesions, and there was an increase in the size of the preexisting lesions in two patients, the outcome of treatment in these two patients was treatment failure. In the remaining 12 patients, a radiological resolution was observed in only six patients.
Of the 42 patients diagnosed to have only TBM, nine cases were in Stage 1 illness and the rest, 33 patients were in the advanced stages of illness. The treatment outcomes were also good in those with Stage 1 illness, whereas those in Stage 2 and Stage 3 had defaulters, deaths, and failure as treatment outcomes.
DISCUSSION
The incidence of tuberculous infection in India is very high contributing to one-fifths of the global burden of TB. Our institute is a tertiary care center catering to the health needs of the Chennai, Southern India. We have an RNTCP unit functioning in our hospital. Cases were diagnosed based on clinical examination and available investigations. Highly probable cases of neuro-TB were registered under DOTS and drugs were issued, and the patients were subsequently followed up at monthly intervals.
A total of 60 patients of new cases of neuro-TB were registered and followed up prospectively. The demographic profile of the patients registered was that the affected were in the age group of 10–59 patients. Majority of the affected were in the age group 20–29. There is a male predominance in the distribution of the illness, whereas the WHO reports an equal distribution among males and females. The sex distribution males are more affected than the females.
The clinical manifestation of our patients was protean. Patients diagnosed as highly probable cases of TBM (according to Ahuja et al., criteria)[5] All had the mandatory clinical features of fever and headache of more than 2 weeks duration. Patients were referred to us with a prolonged duration of fever ranging from 2 weeks to 3 months being treated by the primary care physicians after evaluation for causes of fever. Majority of these patients did not have system localization at the beginning of the fever and on investigating were found to be positive for Widal and leptospirosis and was treated accordingly. The occurrence of vague symptoms and lack of significant signs and symptoms pertaining to nervous system leads to the fallacy in the diagnosis. Patients on arriving at our hospital had the florid symptoms and signs pertaining to the nervous system without much difficulty in diagnosis. Lack of awareness of this life-threatening illness is another cause for lack of early diagnosis and late referral. Patients are referred here after an occurrence of altered sensorium, focal deficits, seizures, and visual impairment.
All patients diagnosed to have tuberculoma presented with seizures. Seizures were more common in tuberculoma than the other forms of neuro-TB spectrum. On detail inquiry about the semiology of the seizures, the predominant seizure type was focal seizures, followed by focal with secondary generalizations. Maduranth has reported seizures to be the predominant manifestation in patients with tuberculoma.[6] Arsen[7] has reported seizures in 85% of patients with tuberculoma. Gulati et al. have reported that the most common cause of focal seizure was tuberculoma.[8]
Swash and Oxbury have reported a history of TB in about 50% of our patients.[9] This must be due to our rigid inclusion criteria which included only new cases of TB. Focal deficits were in the form of hemiparesis, hemiplegia, and cranial nerve palsies.
Our study reports vision impairment in 14% of the entire spectrum of neuro-TB. The range of vision impairment ranges from legal blindness to functional impairment of vision. None of them at presentation had volunteered this problem. Sinha et al.[10] reported that 27% of TBM patients had decreased vision due to optochiasmatic arachnoiditis (OCA). Anupriya A et al.[11] report a figure of 14% with OCA. In view of the occurrence of this problem in the significant portion of the patients, it has to be anticipated though this problem is not volunteered. We had not come across cases of etham butol-induced optic neuropathy. Choreoathetoid movements were the initial presentation of tuberculoma in 5 % of patients. Alarcón et al. has also documented choreoathetoid movement to be the presenting manifestation of tuberculoma.[12]
The spectrum of neuro-TB includes TBM (with or without tuberculoma and spinal arachnoiditis) and isolated tuberculoma. In our study, 65% (39 patients) of the spectrum comprises of TBM (with or without associated tuberculoma). Two studies have documented 70%–80% of cases of neuro-TB spectrum to be TBM (with or without tuberculoma/arachnoiditis).[13]
Clinical staging of the illness as per MRC grading done showed that the majority of our patients were in Stage 2 (15 patients - 35%) and 3 (18 patients - 43%) of illness at presentation. In TBM the only and single most important physician governed factor irrespective of the treatment regimen which decides the outcome of the illness is the clinical stage of the illness. Ahmadinejad documented 14.6% in Stage I, 34.4% in Stage II, and 51% in Stage III TBM 17. They found that age and the clinical stage of the illness[6] were prognostic factors which decided the outcome.[14]
CSF protein estimation at presentation in patients with TBM (with or without tuberculoma/arachnoiditis) revealed elevated proteins. The levels being 33% (14 patients) had mild elevation (<100 mg/dl), 38% (16 patients) had moderate elevation (101–500) and 28% (12 patients) had severe elevation (>501). Nearly 88% of patients who presented in Stage 2 and Stage 3 of illness had moderate-to-severe elevation of proteins. This shows that those who presented in advanced stages had higher levels of CSF proteins. CSF sugars were normal by 55% and reduced <2/3rd in 45% of patients. No correlation was found between the CSF sugars and the severity of illness. In contrary, Hosoglo has found a correlation between the severity of the illness and CSF sugar levels.[15] 76% of the patients showed a tuberculous range of lymphocytic pleocytosis. In our study, we were not able to document the microorganism in the biological fluid. The golden standard in the diagnosis of TBM is detection of tubercle bacilli in CSF (by smear or culture), and large volumes of CSF have to be centrifuged and examined. Bacteriological diagnosis was made in 107 of 132 adults with clinically suspected TBM.[11]
Our study revealed that the most common finding on imaging in patients with TBM (with or without tuberculoma/arachnoiditis) to be meningeal enhancement (31 patients - 75%), hydrocephalus (22 patients - 52%), basal exudates (18 patients - 42%), infarcts (7 patients - 7%), and granulomas (15 patients - 35%). Two studies have revealed basal enhancement of the meninges (particularly in the per mesencephalic cisterns), hydrocephalus, infarction edema often located periventricular, and mass lesions due to associated tuberculoma or tuberculous abscess, to be imaging abnormalities in descending order.[1617] A study revealed that hydrocephalus was the single most common abnormality seen by computerized tomography scan in 52%–80% of patients with TBM. Goyal et al. studies revealed that enhancement of the meninges is seen in approximately 60% of patients with TBM which may be localized or diffuse.[18] Two large community-based studies analyzed the imaging findings in patients with TBM and found that hydrocephalus was found in 78%, basal enhancement was found in 38% infarcts in 15%–30%, and tuberculoma in 5%–10% of the patients.
The common site of location of this tuberculoma is parietal and frontal lobe. Multiple tuberculoma were more common than solitary tuberculoma. The location of tuberculoma in the infratentorial compartment was less frequent. In our study, we have documented a single case of brain-stem tuberculoma in an adolescent girl who presented with choreoathetotic movements. The distinctive MRI features of noncaseating granulomas, caseating granulomas with the solid or liquid center was made out.
In our study, only 6 out of 60 patients required surgical intervention. The procedures done on these patients were ventriculoperitoneal (VP) shunt and drainage of the abscess. VP shunt was done in patients with TBM and hydrocephalus. Patients with TBM and hydrocephalus were staged from 1 to 4. Of the five patients who underwent the shunting procedure, two patients were in Stage 2 of illness and three were in Stage 3 of the illness. The outcome of the procedure was that patients who underwent the shunting procedure in Stage 3 illness succumbed to the lot of complications such as shunt dysfunction, shunt infection requiring shunt revision. Regarding the outcome of the patients treated with surgical intervention out of 6 patients, two died, four patients were labeled as treatment failure, as they continued to develop worsening of clinical features apart from shunt-related complications. The outcome of surgical intervention (VP Shunting procedure) in patients with advanced stages of TBM and hydrocephalus is not associated with high mortality and hence the utility of these procedures is debatable.[19]
Nearly 75% of those treated with RNTCP regimen were rendered asymptomatic after completion of treatment. Treatment failure was 8.33%, and death rate was 3.33%. In 16.66%, we lost to follow-up as patients did not turn up for their monthly follow-up.
The primary goal of RNTCP is to achieve a cure rate of 85% (in spectrum positive ¨C pulmonary tuberculosis cases) and the secondary goal is case detection of 70%. RNTCP focuses mainly on pulmonary TB, and the same targets are maintained for extrapulmonary TB. To document a cure, we need to document the presence of the microorganism in the biological fluid and also its clearance after completion of treatment. We were not able to document the microorganism in any of our cases. The diagnosis was done based on prevalidated criteria, and we were able to see clinical and radiological improvement after treatment which is defined as treatment completed or successful treatment. Although we were not able to document a cure of 85%, we were able to demonstrate a successful treatment in 75% of the patients which is close to the target.
CONCLUSION
TBM patients present in the advanced stage (Stage 2 and Stage 3) of the illness. The most common complication of TBM is hydrocephalus, and the most devastating complication of neuro-TB is visual impairment due to OCA. CSF proteins correlated with clinical severity of illness and it can be used to prognosticate the adverse outcome. Early diagnosis of neurological TB is important because the timing of initiation of anti-TB treatment is the most important variable for predicting the outcome in these patients. A high index of clinical suspicion coupled with a battery of imaging and CSF laboratory investigations are required to confirm the diagnosis as it is exceptionally difficult to ascertain histopathological/microbiological proof.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Tuberculosis: Current situation, challenges and overview of its control programs in India. J Glob Infect Dis. 2011;3:143-50.
- [Google Scholar]
- Centers for Disease Control. Reported Tuberculosis in the United States, 2004. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control; September; 2005.
- Chronic meningitis. In: Neurological Infections; Major Problems in Neurology. Vol 16. Philadelphia: W.B. Saunders; 1998. p. :169-248.
- [Google Scholar]
- Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India. TB India 2010. RNTCP Status Report. New Delhi: Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare; 2010.
- Diagnostic criteria for tuberculous meningitis and their validation. Tuber Lung Dis. 1994;75:149-52.
- [Google Scholar]
- Neurological tuberculosis. In: Sharma SK, Mohan A, eds. Tuberculosis (2nd ed). New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2009. p. :304-29.
- [Google Scholar]
- Two hundred and one cases of intracranial tuberculoma treated surgically. J Neurol Neurosurg Psychiatry. 1958;21:308-11.
- [Google Scholar]
- Clinical Neurology. London: Churchill Livingston; 1991.
- Vision impairment in tuberculous meningitis: Predictors and prognosis. J Neurol Sci. 2010;290:27-32.
- [Google Scholar]
- Tuberculous optochiasmatic arachnoiditis. Neurol India. 2010;58:732-5. doi: 10.4103/0028-3886.72194
- [Google Scholar]
- Movement disorders in 30 patients with tuberculous meningitis. Mov Disord. 2000;15:561-9.
- [Google Scholar]
- Tuberculous meningitis: Many questions, too few answers. Lancet Neurol. 2005;4:160-70.
- [Google Scholar]
- Tuberculous meningitis in an urban medical center. Medicine (Baltimore). 1987;66:317-26.
- [Google Scholar]
- MRI in tuberculous meningoencephalitis: Report of four cases and review of the neuroimaging literature. J Neurol. 1991;238:340-4.
- [Google Scholar]
- Imaging appearance of pachymeningeal tuberculosis. AJR Am J Roentgenol. 1997;169:1421-4.
- [Google Scholar]
- Management of hydrocephalus in patients with tuberculous meningitis. Neurol India. 2009;57:368-74.
- [Google Scholar]






