Translate this page into:
Economic Cost of Schizophrenia in a Nigerian Teaching Hospital
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
This study evaluated the economic cost of schizophrenia in Nigerian patients and identified factors that influence cost.
Methods:
A total of 100 participants with schizophrenia were assessed using the modified economic cost questionnaire, the mini-international neuropsychiatric interview, the positive and negative syndrome scale, the Liverpool University Neuroleptic side-effect rating scale, and the global assessment of functioning scale. Associations between sociodemographic characteristics, illness-related variables and direct, indirect, and total costs of schizophrenia were assessed.
Results:
The average annual total, direct, and indirect costs of the treatment were $818.48, $349.59, and $468.89, respectively, per patient. The direct cost constituted 42.7%, while the indirect cost was 57.3% of the total costs of treatment. Hospitalization was the leading contributor to the direct cost, while productivity loss was a major component of the indirect cost.
Conclusion:
Schizophrenia is an expensive disease in Nigeria, measures to reduce hospitalization could significantly reduce the cost of illness to the patient and their relatives.
Keywords
Cost of illness
direct cost
economic burden
indirect cost
productivity loss
total cost
INTRODUCTION
Schizophrenia is a chronic mental disorder that is associated with significant and long-lasting health, social and financial/economic burden, on patients, their families, other caregivers, and the wider society.[1] Schizophrenia is estimated to affect about 24 million people worldwide with a peak age of 15–45 years.[2] The economic effects of this disorder extend beyond the utilization of health and personal social services but also include its associated morbidity and mortality.[34] Schizophrenia has been shown to place a substantial economic burden on the health system and society in general.[5]
Several studies have been carried out to estimate these costs in the developed countries.[5] In England, the total societal cost of schizophrenia was estimated at £6.7 billion in 2004/2005 prices.[6] Of this amount, about £2 billion (approximately 30%) constituted the direct cost of care while the remainder constituted the indirect cost. The cost of lost productivity for individuals with schizophrenia due to unemployment, absenteeism, and premature mortality was estimated to be £3.2 billion, while the cost of lost productivity for careers was estimated to be £32 million.[6] The cost of informal care and private expenditures borne by family members was approximately £615 million.[6] Similarly, in the United States of America, the cost of schizophrenia in 2013 was estimated to be $155.7 billion, of which the total direct health-care cost was estimated at $37.7 billion, the direct nonhealth-care cost was $9.3 billion, and the total indirect costs were $117.3 billion.[7] The largest components of cost were attributed to unemployment (38%), productivity loss due to caregiving (34%), and direct health-care cost (24%).
Even though mental health problems are a significant cause of morbidity, the general Nigerian population (including policymakers) does not see mental conditions as a valid health problem with significant implications of budgeting and mental health-care funding.
There is a dearth of research in Africa, investigating the economic cost of schizophrenia. Only two studies had assessed the economic cost of schizophrenia in Nigeria, and both were conducted over a decade ago. The mean total cost of schizophrenia per patient was found to be N2951.4 ($35.9) over a 6-month period.[8] Amoo and Ogunlesi also reported the mean total cost of treating inpatients with schizophrenia to be N11,337 ($85.9), direct cost was N9882 ($74.9), and indirect cost was N3604 ($27.3) over a 1-year period.[9] The study by Suleiman et al. looked specifically at only outpatient costs and did not consider hospitalization costs, while Amoo and Ogunlesi restricted their participants to inpatients and assessed only hospitalization costs.[89]
The general aim of the present study is to update knowledge by doing a comprehensive assessment of the cost of treatment of participants with schizophrenia using a standardized instrument over a period of 1 year. Furthermore, this study explored the various factors that may be associated with the cost of treatment of schizophrenia in the Nigerian population. Therefore, the specific objectives of this study were as follows: (1) to assess the direct, indirect, and total costs of schizophrenia using a bottom-up approach, (2) highlight the various components of the direct, indirect, and total costs, and (3) to identify the factors associated with this cost.
METHODS
Ethics
The approval of the research protocol was obtained from the Ethics and Research Committee of the Obafemi Awolowo University Teaching Hospital (OAUTHC), Ile-Ife with protocol number ERC/2011/12/08 and International registration number IRB/IEC/0004553. Written informed consent was obtained from all patients and caregivers after the aim of the study had been explained to them. All participants gave a consent to publish the results of the study.
Study design
This study was cross-sectional and the study period was for a 1-year period (March 2011–March 2012) conducted at the outpatient clinic of the mental health unit of the OAUTHC, Ile-Ife, Osun State, Nigeria. A total of 100 patients who had previously been diagnosed as having schizophrenia were consecutively recruited into the study. The diagnosis of schizophrenia was confirmed using the mini-international neuropsychiatric interview, English version 5.0.0 (lifetime diagnosis). They also had to be stable and on antipsychotic medication for at least 1 year. Patients caregiver was simultaneously recruited if they were at least 18-year-old, the most important source of care for the patient for at least 1 year and free from major medical or psychiatric conditions that could affect their level of functioning. Totally 100 caregivers were identified and recruited into the study.
Cost assessment
Study instrument and identification of costs
-
The modified economic cost questionnaire – this was adapted from the economic cost questionnaire developed by Yeh.[10] This questionnaire was used to estimate the direct and indirect costs and was filled by a psychiatrist who carefully went through the details in the case notes over the past year. It assessed the following:
-
Sociodemographic characteristics of the patient, that is, age, sex, marital status, level of education, address, employment status, and participation in health insurance scheme
-
The direct costs components assessed included (a) inpatient costs, (b) outpatient costs, (c) day hospital costs, (d) medication fees, (e) emergency treatment costs, (f) laboratory investigations, (g) cost of private health facilities, and (h) cost of private home care services. The details of hospitalization in the past 1 year were checked from the case notes, and the cost was calculated by multiplying the number of days spent on admission by the daily price rate of hospital admission and the amount spent on outpatient attendance was calculated by multiplying the number of times the patient attended the outpatient unit over the last year which was checked from the case notes and multiplied by the consultation fees. Details of interventions in the community, day hospitals, emergency treatment, private health facilities, and private home care services were ascertained from the patients and their caregivers. These were quantified in terms of duration and payments made
-
The indirect costs included the amount spent on transportation, time costs (amount of time spent waiting in transport services, amount of time spent travelling to the hospital, amount of time spent waiting before seeing the doctor [waiting time], the amount of time spent waiting for medications, the amount of time spent at traditional/religious centers, the amount of money spent for care at the traditional/religious centers, and the amount of time spent on transportation to traditional/religious centers), productivity loss, the cost of legal services, and damages due to illness behavior. The human capital method was used to estimate the monetary value of healthy time using minimum wage rates in Nigeria
-
Illness-related characteristics of the patient, that is, age at onset of illness, duration of illness, number of admissions due to illness, age at first admission, time since last admission, and duration of admission in the last year.
-
Other instruments
2. Positive and negative syndrome scale (PANSS) was used to assess symptom severity[11]
3. Liverpool University Neuroleptic Side-Effect Rating Scale (LUNSERS) was used to assess medication side effects[12]
4. Global assessment of functioning (GAF) scale was used to assess current functioning.[13]
Instruments used to assess caregivers
5. The amount of time spent by the caregiver staying with the patient during hospitalization, at the traditional or religious center, the amount of time spent accompanying the patient to the hospital, traditional or religious center, and cost of their transport to the hospital, traditional or religious center was assessed as part of indirect costs to the patient
6. Sociodemographic characteristics of the caregiver, that is, age, sex, marital status, level of education, address, and employment status.
Statistical analysis
The statistical product and service solution version 21 (SPSS 21)[14] program was used for statistical analysis. Correlations between cost (direct, indirect, and total) and the variables (sociodemographic- and illness-related variables) were studied using Pearson's product moment correlation coefficient. Multiple linear regression analysis with the stepwise method was used to explore the significant factors (sociodemographic- and illness-related variables) associated with the direct, indirect, and total costs of patients with schizophrenia. The level of statistical significance was taken as P < 0.05 at all levels of analyses, and statistical tests were two tailed.
RESULTS
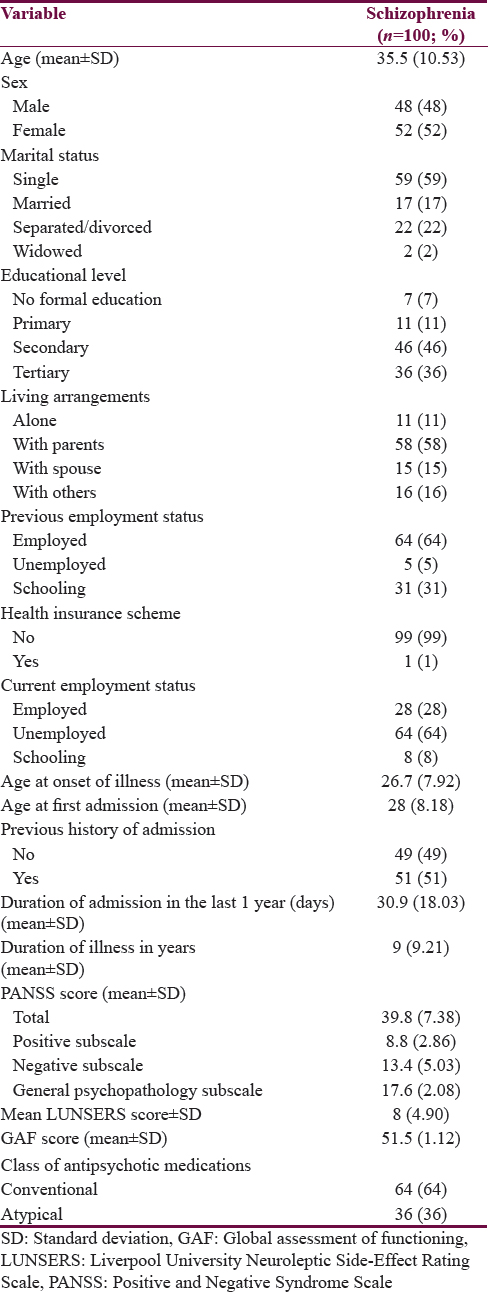
The mean age of patients was 35.5 years (±10.53), only one (1%) patient with schizophrenia had health insurance. The mean age of onset of illness was 26.6 years (±7.92), while the mean duration of illness was 9.0 years (standard deviation [SD] ±9.21). The mean duration of admission in the last 1 year was 30.9 days (SD ± 18.03). The mean number of admissions was 1.0 (SD ± 1.32). About 64% of participants were on conventional antipsychotics, while 36% were on atypical antipsychotics. The mean PANSS score was 39.8 (±7.38) for the whole scale, 8.8 (±2.86) for the positive subscale, 13.4 (±5.03) for the negative subscale, and 17.6 (±2.08) for the general psychopathology subscale. The mean LUNSERS score was 8.0 (±4.90) [Table 1].
The mean total annual cost was $818.5 (±684.35). The mean annual direct cost was $349.6 (±296.04) which constituted 42.7% of the total cost. The largest component of the direct costs was accounted for by medications; this constituted 51.2% of the direct cost and 21.9% of the total cost. This was followed by inpatient admission (21% of direct cost and 9% of total cost) and religious treatment (14.2% of direct cost and 6.1% of total cost) [Table 2].

The mean annual indirect cost was $468.9 (±489.93) which was 57.3% of the total cost. For the indirect cost, productivity loss (39.1% of the indirect cost and 22.3% of the total cost) accounted for the highest proportions. This was followed by transportation cost which constituted 23.1% of the indirect cost and 13.2% of the total cost [Table 3]. Appendix 1

A moderate positive correlation was observed between the direct, indirect, and total costs, and duration of admission, while a weak positive correlation was noted between all subtypes of cost and PANSS-positive scores [Table 4].

The duration of admission was the only variable that significantly predicted the economic cost in terms of the direct, indirect, and total costs [Table 5].

DISCUSSION
Our findings showed that schizophrenia is a costly disease in Nigeria just as in developed countries. The mean total, direct, and indirect costs per patient was $818.48, $349.59 (42.7%), and $468.89 (57.3%). Nigeria is Africa's most populous country with an estimated population of 186 million people.[15] Given the prevalence rate of 0.4%, the Nigerian population estimated to be living with schizophrenia is about 1.86 million people and the national cost of schizophrenia estimated as $609 million.[16] This is a large estimate and indicates a huge economic burden of schizophrenia in a developing country; however, larger studies are needed to obtain more reliable estimates.
The mean total cost of schizophrenia in the present study is lower compared to findings from other countries, in China, it was $2586.21, while in the US, it was $44,773 per patient.[1718] This may be accounted for by the absence of cost components such as estimates for homeless shelter, research, training, premature mortality, and suicide in the Nigerian context. However, considering that 70.8% of the Nigerian population lives on <1 dollar per day, the cost of schizophrenia is relatively high.[19]
The direct cost per patient with schizophrenia in this study was 42.7% of the total cost and this finding is similar to those from other studies which reported direct costs ranging from 48.5% to 53.2% of the total cost.[20] The cost of medications was the single largest contributor to direct costs in this study which is in contrast to findings from other studies that identified in-patient admission as the single largest contributor to the direct costs of treating schizophrenia.[2021] The proportion of the direct cost due to medication cost found in this study was comparable to that found in previous studies from Nigeria and Taiwan.[822] However, it was higher than what the majority of studies have reported in which costs of medications make up a relatively minor proportion of the direct and total costs.[2123] The high costs of medications may be explained by high exchange rates of drug importation, lack of medication subsidy by the government, and out-of-pocket health-care financing by patients. Only 10% of the Nigerian population are covered by the Nigerian National Health Insurance Scheme (NHIS), most of whom are formal sector workers who can usually afford healthcare.[24] The economic burden on patients with schizophrenia may be increased by other social factors such as the already higher rates of unemployment among them and the absence of social welfare packages in the country.
Inpatient care was the second largest contributor to direct cost. This is consistent with findings from higher income countries in which inpatient admission contributed significantly to the direct cost for patients with schizophrenia.[20] The high cost of inpatient care in developed countries may reflect the impact of medical comorbidities such as intensive care which is not a frequent component of mental healthcare in Nigeria. In contrast, the high cost of inpatient care in this present study reflects the low coverage of health insurance with consequent out-of-pocket payment. This indicates the need for cheaper alternatives such as case finding and early treatment, community mental health services, and integration of mental health into the primary health-care services.
The indirect cost was 57.3% of the total cost, and this was similar to previous reports on patients with schizophrenia which estimated the indirect cost to range from 46.8% to 51.5%.[20] Productivity loss for both patients with schizophrenia and their caregivers as well as unemployment in patients still contributed to the huge percentage of the indirect cost. This also represents a significant drain on the country's resources and indicates a need to prioritize the mental health needs of the population.
In those, who accessed complementary and alternative treatment, the costs of religious and traditional treatments were high. This indicates the perception of the possible etiology of schizophrenia and the pathway to healthcare. Studies in Nigeria have shown that majority of the population (about 70%) seek mental healthcare from non-Western means such as religious organizations and traditional healers due to the strong belief in supernatural factors as the cause of mental illness.[2425] This is important for policy formulation and intersectoral collaborations, in which traditional and religious leaders may be taught how to identify and know when to refer a patient with schizophrenia to the hospital, especially when they are not responding to the treatments given. Such referral pathways need to be strengthened as they can potentially reduce the economic burden of schizophrenia.
Productivity loss in patients with schizophrenia constituted the largest percentage for the indirect costs. The percentage of patients with schizophrenia who were unemployed was 64% compared to 5% of them who were unemployed before the onset of illness. A large part of the global economic impact of mental illness stems from the difficulties encountered by people with schizophrenia in finding and keeping paid employment.[21] About a third of all sickness absence from work has been attributed to common mental disorders, and there are also large impacts on productivity at the workplace.[262728] In the case of schizophrenia, the most important feature of indirect costs is the loss of productivity resulting from patient morbidity and mortality (i.e., loss of ability to work).[21] With a low average age of illness onset combined with the chronic nature of schizophrenia, the loss of productivity for the national economy can be very high. In the US and Canada, productivity loss was estimated to be about $1.23 billion and $1.03 billion, respectively, while in the UK, it was estimated to be between £78.8 million and £1.7 billion.[29303132]
The average cost to the caregivers for patient with schizophrenia was also high; this highlights the high dependence on family members to provide care in our environment. With its chronic course and early onset, schizophrenia can have substantial psychological and economic impacts not only on people with the illness but also on their families. A five-country European study reported that family caregivers for adults with schizophrenia spent on average from 6 to 9 h per day providing support,[33] and the most common impacts reported were constraints on social activities, negative effects on family life, and feelings of loss. These indirect costs may constitute only a small proportion of the total cost of schizophrenia, but their impact on some families can be large, although difficult to measure accurately.[34] In Nigeria, two studies found that financial impoverishment constituted the greatest source of burden to families, followed by the effect on family routine and family interaction.[35]
In this study, illness, severity, and duration of admission were found to positively predict the direct, indirect, and total costs in patients with schizophrenia. This may be due to the need for inpatient care which contributed significantly to the direct costs of illness. Patients presenting for the first time often show acute psychotic symptoms that require hospitalization, while the treatment for people with repeated relapses is also still predominantly hospital-based across most parts of the world.
Schizophrenia is a potentially devastating illness with a tremendous impact on the lives of both patients as well as the caregivers and it is conceptualized as a lifelong disorder.[36] Severity of illness has also been identified by a number of studies as a factor responsible for high-economic burden.[3738] The higher the severity of the symptoms, the longer the period required to control the symptoms and stabilize the patient and hence, the higher the economic burden. Another study which evaluated 404 patients from five study centers found that negative symptoms were associated with higher total costs and costs for inpatient, day care, residential care, and community services but with lower costs for outpatient care.[39]
In this study, the duration of admission was the single most important factor that predicted cost at all levels for both schizophrenia and asthma. This means that measures that reduce hospitalization, for example, community treatment of mental illness, can be of immense contributions.
In interpreting the findings from this study, the following limitations have to be considered. The study was conducted in a single center and may not be representative of the economic burden of participants with schizophrenia in other parts of Nigeria. Patients may also be prone to recall bias; however, the majority of the information was cross-checked in the case notes of the patients. The productivity loss figures used in this study are estimates, at best, due to lack of objective methods of measurement.
Conclusion and Implications for policy
Our findings indicate that schizophrenia is a costly disease in Nigeria, as such efforts to increase the coverage of the NHIS will be beneficial. Despite the existence of the NHIS in Nigeria, since 2005, only 10% of the population are covered which are the formal sector workers. In a country, where 70.6% live on <1 dollar per day and 92.4% on <2 dollars per day increased NHIS coverage will substantially reduce the economic costs of schizophrenia. Our findings also suggest that strategies to reduce inpatient care will reduce the cost of illness for schizophrenia. These include active case finding which will lower the costs of treatment by reducing the need for admission and facilitate outpatient care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We sincerely appreciate the immense contributions of Late Prof. Femi Fatoye who supervised and participated in this research but passed on before the work could be published.
REFERENCES
- The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, and Risk Factors in 1990 and Projected to 2020. Boston MA: Harvard University Press; 1996.
- [Google Scholar]
- Cultural and demographic factors of schizophrenia. Int J Psychosoc Rehabil. 2006;10:89-103.
- [Google Scholar]
- World Health Organisation. The World Health Report. Mental Health Report: New Understanding, New Hope. Geneva: World Health Organisation; 2001. p. :33-4.
- Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA. 2004;291:2581-90.
- [Google Scholar]
- Global economic burden of schizophrenia: A systematic review. Neuropsychiatr Dis Treat. 2016;12:357-73.
- [Google Scholar]
- The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77:764-71.
- [Google Scholar]
- Financial cost of treating out-patients with schizophrenia in Nigeria. Br J Psychiatry. 1997;171:364-8.
- [Google Scholar]
- Financial cost of treating Nigerian in-patients with schizophrenia. Afr J Med Med Sci. 2005;34:15-23.
- [Google Scholar]
- The economic cost of severely mentally ill patients. Chin J Ment Health. 1997;10:1-15.
- [Google Scholar]
- The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261-76.
- [Google Scholar]
- A self-rating scale for measuring neuroleptic side-effects. Validation in a group of schizophrenic patients. Br J Psychiatry. 1995;166:650-3.
- [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed). Washington, DC: American Psychiatric Publishing; 1994.
- IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp;
- U.S. Census Bureau. United States Census Bureau QuickFacts. California: U.S. Census; 2016. p. :1-9.
- Global Burden of Schizophrenia in the Year 2000. Version 1 Estimates. California: World Health Organization; 2001. p. :1-11.
- An investigation of economic costs of schizophrenia in two areas of China. Int J Ment Health Syst. 2013;7:26.
- [Google Scholar]
- The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77:764-71.
- [Google Scholar]
- United Nations Development Programme. Human development report 2006. J Gov Inf. 2006;28:839-40.
- [Google Scholar]
- The functionality and economic costs of outpatients with schizophrenia in Taiwan. Psychiatry Res. 2008;158:306-15.
- [Google Scholar]
- Assessment of costs and benefits of drug therapy for treatment-resistant schizophrenia in the United Kingdom. Br J Psychiatry. 1993;162:38-42.
- [Google Scholar]
- Expanding health insurance scheme in the informal sector in Nigeria: Awareness as a potential demand-side tool. Pan Afr Med J. 2017;27:52.
- [Google Scholar]
- Psychiatric research in nigeria: Bridging tradition and modernisation. Br J Psychiatry. 2004;184:536-8.
- [Google Scholar]
- Lay beliefs regarding causes of mental illness in Nigeria: Pattern and correlates. Soc Psychiatry Psychiatr Epidemiol. 2008;43:336-41.
- [Google Scholar]
- Mental health and absence from work: New evidence from the UK quarterly labour force survey. Work Employ Soc. 2003;17:731-42.
- [Google Scholar]
- The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med. 2001;43:218-25.
- [Google Scholar]
- The economic burden of schizophrenia: Conceptual and methodological issues, and cost estimates. In: Moscarelli M, Rupp A, Sartorius N, eds. Handbook of mental health economics and health policy. Handbook of mental health economics and health policy. Vol 1. Schizophrenia; Oxford, England: John Wiley & Sons; 1996. p. :321-34.
- [Google Scholar]
- Cost of schizophrenia to UK society. An incidence-based cost-of-illness model for the first 5 years following diagnosis. Pharmacoeconomics. 1999;15:597-610.
- [Google Scholar]
- Burden on the families of patients with schizophrenia: Results of the BIOMED I study. Soc Psychiatry Psychiatr Epidemiol. 1998;33:405-12.
- [Google Scholar]
- Cost effectiveness of day and inpatient psychiatric treatment: Results of a randomised controlled trial. BMJ. 1997;314:1381-5.
- [Google Scholar]
- The burden of schizophrenia on the family. A study from Nigeria. Br J Psychiatry. 1992;161:779-82.
- [Google Scholar]
- Dementia Praecox and Paraphrenia. New York: Krieger Publishing Company; 1971.
- The analysis of the cost structures of the treatment of schizophrenia by means of standardized assessment instruments. Psychiatr Pra×. 2001;28(Suppl 2):S102-8.
- [Google Scholar]
- Comparing patterns and costs of schizophrenia care in five European countries: The EPSILON study. European psychiatric services: Inputs linked to outcome domains and needs. Acta Psychiatr Scand. 2002;105:42-54.
- [Google Scholar]
- Associations between negative symptoms, service use patterns, and costs in patients with schizophrenia in five European countries. Clin Neuropsychiatry. 2008;5:195-205.
- [Google Scholar]
APPENDIX 1
Time cost for employed patients, medical services = ([days spent on admission × 8 h/day] + [one-way travel time × 2] + [time spent for OPD treatment + (one-way travel time × 2) × number of OPD visits]) × average hourly income* Time cost for employed patients, nonorthodox services = ([days spent at traditional treatment + days spent at religious treatment + days spent at alternative treatment × 8 h/day] + [(one-way travel time to traditional treatment + one-way travel time to religious treatment + one-way travel time to alternative treatment) × 2]) × average hourly earnings* Time cost for employed caregivers, medical services = ([number of admission visits × h spent] + [one-way travel time × 2] + [(time spent for OPD treatment + (one-way travel time × 2)] × number of OPD visits]) × average hourly income* Time cost for employed caregiver, nonorthodox services = ([number of visits to traditional treatment + number of visits to religious treatment + number of visits to alternative treatment × h spent] + [(one-way travel time to traditional treatment + one-way travel time to religious treatment + one-way travel time to alternative treatment) × 2]) x average hourly earnings* Productivity loss for unemployed patient, medical services = ([days spent on admission × 8 h/day] + [one-way travel time × 2] + [time spent for OPD treatment + (one-way travel time × 2) × number of OPD visits]) × 24.44** Productivity loss for unemployed patients, nonorthodox services = ([number of visits to traditional treatment + number of visits to religious treatment + number of visits to alternative treatment × 8 h/day] + [(one-way travel time to traditional treatment + one-way travel time to religious treatment + one-way travel time to alternative treatment) × 2]) × 24.44** Productivity loss for unemployed caregivers, medical services = ([number of admission visits × h spent] + [one-way travel time × 2] + [time spent for OPD treatment + (one-way travel time × 2) × number of OPD visits]) × 24.44** Productivity loss for unemployed caregivers, nonorthodox services = ([number of visits to traditional treatment + number of visits to religious treatment + number of visits to alternative treatment × h spent]) + [(one-way travel time to traditional treatment + one-way travel time to religious treatment + one-way travel time to alternative treatment) × 2]) × 24.44** Transportation = (one-way fare × 2 x number of OPD visits) + (one-way fare for admission × 2) + (one-way fare for emergency visit × 2) + (one-way fare for private hospital visit × 2) + (one-way fare for religious medicine × 2) + (one-way fare for alternative medicine × 2) + (one-way fare for traditional medicine × 2)
*Average hourly income = income per month divided by average working days in a month (22 days) and hours in a day (24 h). This was used for those who were employed
**minimum wage divided by the hours per month multiplied by the unemployment rate (18000/[8*22])*0.23. This was used for the unemployed






