Translate this page into:
Is Crush Cytology of Central Nervous System Lesions Relevant in Surgical Practice Today?
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Intraoperative crush cytology is a useful tool for diagnosing the lesions of the central nervous system (CNS). However, because of the development of newer and better imaging techniques, it is important to evaluate if crush cytology is still relevant in neurosurgical practice.
Aims:
We evaluated the crush cytology smears in a series of cases where neurosurgical intervention was performed. We studied the role of crush cytology in the intraoperative diagnosis. We report a series of cases where intraoperative crush cytology helped the surgeon revise the surgery during the operation.
Materials and Methods:
A small portion of all CNS lesions was taken intraoperatively and the tissue was crushed between two slides. The slide was stained using the toluidine blue, Leishman stain, Pap stain and a routine H & E stain. The slides were the evaluated.
Results:
We evaluated the 50 cases of CNS lesions. We found that intraoperative crush cytology is particularly important in differentiating between neoplastic and nonneoplastic CNS lesions. It may also help in differentiating lymphomas from high-grade gliomas. Finally, crush cytology may help the surgeon in delineating the lesions during surgery.
Conclusion:
We conclude that crush cytology remains relevant in neurosurgical practice today and it should be adopted in all neurosurgical centers as a routine diagnostic technique.
Keywords
Crush cytology
central nervous system tumors
intraoperative diagnosis
INTRODUCTION
The concept of intraoperative cytology in the evaluation of central nervous system (CNS) lesions was first started by Eisenhardt and Cushing in 1930.[1] Crush cytology was further described by Russel et al., who pioneered the concept of the “wet film technique” in the diagnosis of lesions of the CNS.[2] Since it is a simple and rapid technique, it is a very useful tool in the intraoperative diagnosis of CNS lesions.
Several studies have been done evaluating the value of crush cytology in the diagnosis of CNS lesions. In a study of 326 cases, Jaiswal et al. noted that in 83.7% of cases, there was a concordance between the intraoperative crush cytological diagnosis and the final histopathological diagnosis. They also showed that the accuracy was the most for glioblastomas, meningiomas, and schwannomas and much less in cases of oligodendrogliomas.[3] In another study, 306 cases were evaluated, and the concordance between the cytological and histopathological diagnosis was found to be 93%.[4]
Although considerable literature is available on the concordance between cytology and histopathology in CNS lesions, not much literature is available on the value of crush cytology for the operating surgeon during the operation. By this, we mean that there are few studies which evaluate the relevance of the diagnosis obtained on crush cytology to the surgeon during the operation. For example, in many CNS tumors, the surgeon may not be sure if he is within the lesion despite the specialized neuroimaging techniques. In such cases, a small tissue fragment analyzed by the crush technique may be invaluable in telling the surgeon if he is within the lesion.
It is widely believed that high resolution and specialized neuroimaging techniques would obviate the need for any intraoperative consultation. However, our experience over 2 years has shown that intraoperative consultation continues to be relevant. Modification and planning of CNS surgeries can be done by the neurosurgeon when he has an intraoperative diagnosis available.[5] This is why the intraoperative squash preparation is a simple and accurate tool which can be of immense help to the surgeon.
MATERIALS AND METHODS
In all cases of CNS lesions, a small amount of tissue was removed intraoperatively, and the fresh unfixed material was sent to the laboratory. This material was gently crushed between two slides. The slide which was used for crushing was at a right angle to the slide on which the material was placed. The crush preparation was stained using the toluidine blue stain, a Leishman stain, the Pap stain, and a routine H and E stain.
The remaining tissue was processed for routine paraffin section study. The H and E stain was used in all cases. In some cases, additional immunohistochemical stains were used to confirm the diagnosis.
RESULTS
There were 25 females and 25 males in the study. The mean age was 48.77 years with an age range between 19 and 75 years.
The distribution of cases and the concordance in the diagnosis is as shown in Table 1.
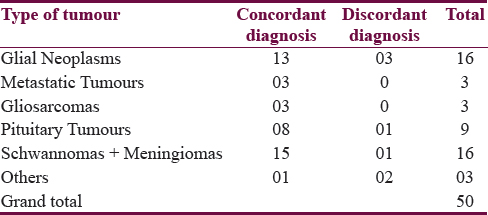
A total of 16 cases of gliomas were reported in this study based on the clinical and radiological examination. However, there were three cases where a wrong diagnosis was offered on crush cytology. The percentage of offering a wrong diagnosis on crush cytology was 18.75%.
Case reports
Case 1
The clinico-radiological diagnosis offered was a glioma/lymphoma. On crush cytology, the case was reported as a lymphoma based on the dyscohesive cell pattern. The cells showed a high N:C ratio and scanty cytoplasm. The cells appeared monomorphic and minimal pleomorphism was seen. Mitotic activity was visualized. On histopathology, there was a diffuse arrangement of the cells. The cells were small to medium sized and appeared atypical with round to polygonal hyperchromatic nuclei and inconspicuous nucleoli. A few bizarre cells with hyperchromatic nuclei were also seen. No vascular proliferation was seen, and the cells did not show a perivascular predilection pattern. The diagnosis offered on histopathology was glioma/primitive neuroectodermal tumors. Immunohistochemistry showed positivity for glial fibrillary acidic protein. The final diagnosis was a Grade IV astrocytoma.
Case 2
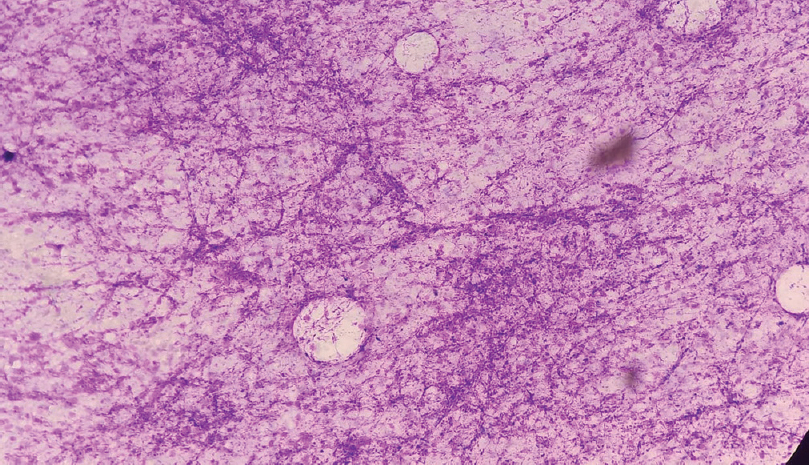
The clinico-radiological diagnosis was a low-grade glioma, and the same was confirmed on crush cytology. However, the histopathology offered was reactive glial proliferation favored over low-grade glioma [Figure 1].
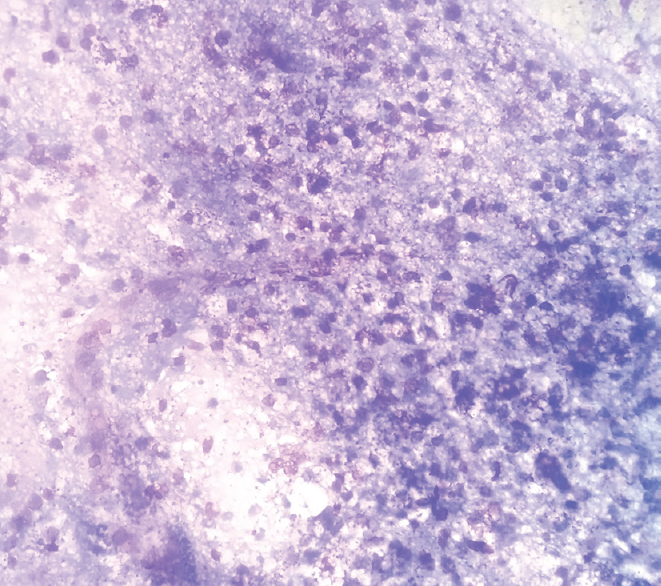
- Crush cytology of Case 3. The diagnosis offered on crush cytology was a high-grade glioma based on the presence of atypical cells and background necrosis. The final diagnosis was a granulomatous lesion of the brain with well-formed granulomas and necrosis. It is important not to confuse the atypical cells with epithelioid cells. In addition, it is important to note that in the case of crush cytology, necrosis is not necessarily equated with a high-grade glioma
Case 3
In the third case, the clinico-radiological diagnosis offered was an intracranial space occupying lesion (ICSOL) which was not described further. The diagnosis offered on crush cytology was a high-grade glioma based on the presence of necrosis and vascular endothelial cell proliferation. However, histopathology showed large areas of necrosis and focal granulomas, which was suggestive of a granulomatous lesion favoring tuberculosis [Figure 2].
- Crush cytology of Case 2. The diagnosis offered was a low-grade glioma on clinic radiological examination as well as on crush cytology. Note the increase in cellularity and a vascular proliferation which is seen on ×40. The nuclei appear relatively bland. The final diagnosis was a reactive gliosis. It is difficult to differentiate between a low-grade glioma and a reactive proliferation since the crush cytology may appear very similar
There were three cases which showed the presence of metastatic lesions in the brain. In one case, the surgeon wanted to confirm that he was in the lesion. The initial crush cytology smear showed only normal cerebellar tissue which allowed the surgeon to change his approach. A repeat cytology was sent which confirmed the presence of metastatic carcinoma cells. This helped the surgeon to remove the lesion while preserving the normal cerebellar tissue.
In a second case, the ICSOL was reported as a brain abscess based on the clinical and radiological picture. However, the cytology showed extensive areas of necrosis with fragments of metastatic deposits of a papillary carcinoma. The presence of metastatic deposits was confirmed on histopathology.
We had 16 cases of schwannomas and meningiomas. There was a discrepancy in one of the cases. This was a case of a suprasellar mass which was reported radiologically as a pituitary adenoma. The crush cytology showed a mixed cell population with a few spindle cells and scattered squamous cells. No fluid or necrosis was seen in the background. The diagnosis offered on crush cytology was a craniopharyngioma. However, the histopathology showed typical features of a meningothelial meningioma, and the diagnosis was revised accordingly. We did not see any other discrepancies between the crush cytology and the histopathology in this subgroup.
There were three cases where the clinico-radiological diagnosis offered was a high-grade glioma. However, the crush cytology in all the three cases was suggestive of a gliosarcoma. The diagnosis of a gliosarcoma was confirmed in all the three cases on histopathological examination.
We reported nine cases of pituitary tumors. In one case, a diagnosis of pituitary tumor was offered on the clinico-radiological examination which was confirmed on crush cytology. However, the histopathology showed very scanty tissue where only olfactory mucosa was seen. However, the final diagnosis was pituitary adenoma based on the crush cytology.
We also saw two cases of mesial temporal sclerosis which were diagnosed as normal brain parenchyma on crush cytology. One case of radionecrosis of the brain was diagnosed as necrotic material on crush cytology.
We attempted to perform a statistical analysis on our results. However, since this was a descriptive study, no valid statistical analysis could be performed.
DISCUSSION
Crush cytology has been reported to be an excellent adjunct in the evaluation of CNS lesions. Since crush preparations preserve the cytology of CNS lesions, they are probably better in the diagnosis of CNS lesions than frozen sections where the cytological detail is not preserved. Cahill and Hidwegi reported that the crush cytology provided a diagnosis in 29 out of the 32 cases which were included in their study.[6] The diagnostic accuracy of crush smears in this study was 90%, which was equivalent to other studies.[2789101112] However, crush cytology has its own limitations, some of which we encountered in the present study.
We reported a case of a high-grade glioma as a lymphoma. High-grade gliomas are known to show a high cellularity with considerable cytological heterogeneity. Usually, the cells are in close to the blood vessels. Endothelial cell proliferation is seen with glomeruloid bodies, cellular pleomorphism, and necrosis.[13] In our case, pleomorphism and necrosis were marked. There were also a large number of mitotic figures. However, the classical fibrillary background was not seen, a feature which led us to believe that the lesion was a lymphoma and not a glioma. Krishnani et al. evaluated 365 crush cytology specimens of the CNS and reported that discordance between crush cytology and histopathology in the diagnosis of lymphomas was very high.[14] Out of the series of 334 cases, they encountered nine lymphomas which were diagnosed on histopathology. Out of these nine cases, only two were correctly diagnosed on crush cytology and three cases were reported as small round cell tumor. Based on the abundant gliofibrillary matrix spreading out from the blood vessels, two cases were misdiagnosed as high-grade astrocytomas in crush cytology. In contrast, Firlik et al. quoted a high diagnostic accuracy for Hodgkin lymphoma.[15] We suggest that a diagnosis of a lymphoma should be offered with caution on crush cytology. A diagnosis of a high-grade glioma should always be offered as a differential diagnosis since the cytology may appear identical in both the cases.
One case of a granulomatous lesion of the brain was wrongly reported as a high-grade glioma. The diagnosis was based on the combination of large areas of necrosis and the absence of well-formed granulomas. Instead, the epithelioid cells in the ill-formed granulomas were wrongly interpreted as malignant astrocytes showing spindle-cell morphology. Similar discrepancies have been reported in literature.[1617] We stained one of the unstained crush smears using the Ziehl–-Neelsen (ZN) stain. Although no acid-fast bacilli (were seen), the ZN stain highlighted the granulomas magnificently. We suggest that the ZN stain should always be included in the panel of stains for crush cytology.
On the other hand, one case which was diagnosed both radiologically as well as intraoperatively as a tubercular abscess was correctly diagnosed as a case of metastatic deposits in the brain on crush cytology. The difference in interpretation was based on the cell morphology and not the presence or the absence of necrosis. Clearly malignant cells were seen in this case which confirmed the diagnosis.
It is reiterated that the diagnosis should not be made based on the background necrosis or the presence of vascular proliferation both of which may create a confusion between a high-grade glioma and a granulomatous lesion with extensive necrosis. Efforts should be made to identify the cell morphology which gives the diagnosis. Differentiating between a neoplastic and a granulomatous lesion is of paramount importance to the surgeon since the extent of surgery is dictated by the diagnosis.
Another interesting case was of a metastatic deposit from carcinoma breast to the left cerebellum. The lesion was very small and located in left cerebellar hemisphere just lateral to the midline at a considerable depth. A midline suboccipital Craniotomy was done, and the tumor was approached through the vermis. Based on the crush cytology report, the approach was revised, and the lesion was approached through the left cerebellar hemisphere. The tumor was then reached, reconfirmed by crush and the entire metastatic deposit resected. In this case, crush cytology helped the surgeon in completely removing the metastatic tumor and prevented future redo-surgery.
There was one case which was reported as a craniopharyngioma in which the diagnosis was revised to a meningioma. More care in evaluating the spindle cells would probably have prevented this error.
CONCLUSIONS
To summarize, our study suggests that crush cytology is a useful adjunct to the diagnosis in neurosurgical practice. The use of the ZN stain must be highlighted. In addition, it is important to remember that although crush cytology is a useful intraoperative technique, preoperative evaluation of the clinical and radiological findings is essential in arriving at the correct diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Diagnosis of intracranial tumors by supravital technique. Am J Pathol. 1930;6:541-52.7.
- [Google Scholar]
- The wet film technique in the diagnosis of intracranial tumours: A rapid method. J Path Bact. 1937;45:501-5.
- [Google Scholar]
- Intraoperative squash cytology of central nervous system lesions: A single center study of 326 cases. Diagn Cytopathol. 2012;40:104-12.
- [Google Scholar]
- Smear preparation of intracranial lesions: A retrospective study of 306 cases. Diagn Cytopathol. 2011;39:582-92.
- [Google Scholar]
- High diagnostic accuracy of cytologic smears of central nervous system tumors. A 15-year experience based on 4,172 patients. Acta Cytol. 2002;46:667-74.
- [Google Scholar]
- Crush preparations of lesions of the central nervous system. A useful adjunct to the frozen section. Acta Cytol. 1985;29:279-85.
- [Google Scholar]
- Squash preparation and frozen section in intraoperative diagnosis of central nervous system tumors. Acta Cytol. 1998;42:1149-54.
- [Google Scholar]
- Cytopathology of the central nervous system. Part I. Utility of crush smear cytology in intraoperative diagnosis of central nervous system lesions. Acta Cytol. 2006;50:608-16.
- [Google Scholar]
- Imprints, smears, and frozen sections of brain tumors. Neurosurgery. 1991;29:575-9.
- [Google Scholar]
- Needle aspiration cytology of intracranial lesions. A review of 84 cases. Acta Cytol. 1982;26:779-86.
- [Google Scholar]
- The histological accuracy of the smear technique for neurosurgical biopsies. J Neurosurg. 1973;39:82-8.
- [Google Scholar]
- Evaluation of the sqash smear technique in the rapid diagnosis of central nervous system tumors: A cytomorphological Study. ISPUB. 2010;11:1.
- [Google Scholar]
- Intraoperative squash cytology: Accuracy and impact on immediate surgical management of central nervous system tumours. Cytopathology. 2012;23:308-14.
- [Google Scholar]
- Use of cytological preparations for the intraoperative diagnosis of stereotactically obtained brain biopsies: A 19-year experience and survey of neuropathologists. J Neurosurg. 1999;91:454-8.
- [Google Scholar]
- Squash preparation: A reliable diagnostic tool in the intraoperative diagnosis of central nervous system tumors. J Cytol. 2010;27:81-5.
- [Google Scholar]
- Frozen section discrepancy in the evaluation of central nervous system tumors. Arch Pathol Lab Med. 2007;131:1532-40.
- [Google Scholar]






