Translate this page into:
Vitamin D Deficiency in Children with Psychiatric Illness in a Tertiary Care Hospital in North India
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Vitamin D is increasingly recognized as important for brain health, apart from its role in endocrine and bone health. There is a growing recognition of worldwide “epidemic” of Vitamin D deficiency, and growing data from adult population illustrate the association between Vitamin D deficiency and psychiatric disorders. In children, its role is implicated in brain development, function, and psychiatric disorders.
Aim:
The aim of this study was to study the extent of Vitamin D deficiency in children and adolescents with psychiatric disorders.
Methodology:
Retrospective chart review of participants, who had attended the psychiatry outpatient department, was conducted to ascertain the extent of blood Vitamin D level requisition and its level.
Results:
Out of 836, 60 participants had received the requisition for blood Vitamin D level, and results were documented for 40 participants (males – 28; females – 12). No specific reason was cited for getting Vitamin D level done. The mean Vitamin D level was in the deficient range, i.e. 13.34 ng/ml with 80% of the sample having Vitamin D deficiency and 13% having insufficient Vitamin D level. More males had Vitamin D deficiency, however, the small number of females in the study limits the generalizability of the results. Among the diagnostic categories, neurodevelopmental disorders had lower mean Vitamin D level, with lowest Vitamin D for autism, i.e., 10.9 ng/ml.
Conclusion:
The cause-effect relationship between Vitamin D deficiency and childhood psychiatric disorders could not be derived from the study. However, it provides important initial data for the relationship between Vitamin D deficiency and childhood psychiatric disorders from India.
Keywords
Adolescents
children
deficiency
psychiatric illness
Vitamin D
INTRODUCTION
Vitamin D is increasingly being recognized as important for brain health, apart from its importance in endocrine and bone health.[1] Evidence is emerging implicating its role in brain development and function.[1] It affects early brain development by acting as a potent differentiating factor for brain cells by increasing neurite outgrowth, regulation of neurotrophic factors and reactive oxygen species, and downregulating calcium channels.[1] Growing data illustrate the association between Vitamin D deficiency and adult psychiatric disorders.[2] Western literature reports that about 1%–78% of the general population have Vitamin D insufficiency.[3] Lower Vitamin D level compared to controls was reported in a systematic review and meta-analysis in adults with depression[4] and schizophrenia.[5] A study reporting the lowest Vitamin D levels in patients with schizophrenia, and autism proposed that during the developmental period low Vitamin D predisposes to psychiatric illness and affects the mental health of adulthood.[6]
Literature showing the evidence of low Vitamin D in children and adolescents is also emerging. Vitamin D levels in 3 months–12 years old, apparently healthy children with minor ailments attending a private pediatric hospital in India reported that 40.24% had insufficient level, 25.44% had deficiency, and 34.32% had sufficient level, respectively.[7] The only study evaluating Vitamin D deficiency in children with psychiatric illness reports that 21% and 64% of the study cohort had deficiency and insufficiency, respectively.[8] A systematic review and meta-analysis report significantly lower Vitamin D level in children with autistic spectrum disorder (ASD), a neurodevelopmental disorder, compared to controls, suggesting that Vitamin D deficiency may be a risk factor for the development of ASD.[9] About 72% of adolescent-onset psychotic illness had low Vitamin D levels (mean Vitamin D – 20.4 ng/ml) in a cross-sectional study.[10]
Literature also suggests that the risk of developing certain psychiatric disorders may be reduced by the prevention of Vitamin D deficiency in early life or the treatment outcome may be improved by Vitamin D supplementation.[11] The risk of schizophrenia, later in life, among males, was reduced the following Vitamin D supplementation in early infancy in a Finnish cohort[12] and the core symptoms of autism improved after Vitamin D supplementation.[13] Another trial of 3 months Vitamin D supplementation in Vitamin D deficient, 106 ASD children reported improvement in scores on a childhood autism rating scale and autism behavior checklist subscales in 80.72% of the study population (2016).[14] Supplementation may have some role in adolescent-onset psychosis, depression, and attention deficit hyperactivity disorder.[1015] Therefore, early identification of Vitamin D deficiency and supplementation assumes importance in clinical practice.
Thus, this study aimed to evaluate the extent of Vitamin D deficiency in children and adolescents with psychiatric disorders and to ascertain any difference in the extent of Vitamin D deficiency across different disorders.
METHODOLOGY
A retrospective chart review was conducted to examine blood levels of Vitamin D [25(OH)D] in all children who had attended child and adolescent psychiatric (CAP) clinic from January 1, 2015 to October 31, 2015 of our institute. Case records were retrieved manually and looked for the prescription of Vitamin D level in the case records. All requests for getting Vitamin D level were made by the psychiatrist. A total of 836 children (new cases and follow-up cases) in the age group of 4–15 years had attended the CAP clinic from January 1, 2015 to October 31, 2015. Requisition for Vitamin D level was given to 60 patients, however, no specific reason was mentioned for getting it done, and no physical illness was recorded in the case notes. Among these, Vitamin D level of only 40 patients was available for this chart review. For determining Vitamin D deficiency or insufficiency, the parameters set by the endocrine society were used (<21–30 ng/ml-insufficiency level and <20 ng/ml is deficiency of Vitamin D). For patients with multiple diagnoses, Vitamin D level was counted for each diagnostic category to calculate the frequency and mean Vitamin D levels. Vitamin D level was compared across gender and global functioning. The Statistical Package for the Social Science Version 20 (SPSS for Windows, Version 20.0. Chicago, SPSS Inc.).
RESULTS
Sociodemographic and clinical profile
Majority of the study sample were boys (n = 28; 70%), with a mean age of around 10 years, and the majority were Hindus (77.5%) from urban background (72.5%). Most of them were ill for 4–5 months and majority (90%) had more than one diagnosis. The sociodemographic details and clinical profile are summarized in Table 1.
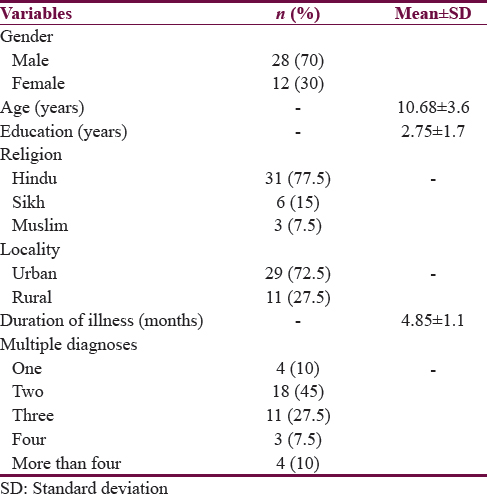
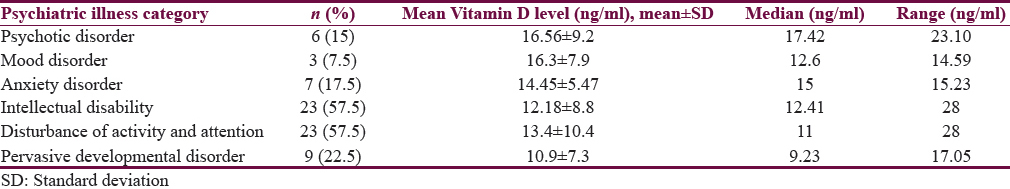
Table 2 summarizes the various diagnostic categories (according to International Statistical Classification of Diseases-10) considered in the study.

Vitamin D levels
The mean Vitamin D level for the sample was 13.34 ± 8.26 ng/ml (i.e. deficiency). Females in the study sample had a lower mean level (13.26 ± 10.7 ng/ml) than that in males (13.38 ± 7.19 ng/ml); however, the difference was not significant. About 80% (n = 32) of the study sample had Vitamin D deficiency (<20 ng/ml) and around 13% had insufficient (21–30 ng/ml) Vitamin D level. Comparison of deficient and insufficient level across the gender revealed that more males (n = 24) had deficiency compared to females (n = 8), and the difference was statistically significant (P = 0.02). However, this result cannot be generalized given the small number of females in the study group. These results are summarized in Table 3.

Vitamin D level across diagnostic categories
The mean Vitamin D level across various diagnostic categories was in deficient range as shown in Table 4a, with the lowest mean for autism, i.e., 10.9 ± 7.3 ng/ml, followed by intellectual disability 12.18 ± 8.8 ng/ml, and hyperkinetic disorder 13.4 ± 10.4 ng/ml. Table 4b depicts the number of participants with deficient and insufficient Vitamin D level in each diagnostic category.

DISCUSSION
This study found that a high percentage of children and adolescents with psychiatric disorders have Vitamin D deficiency. Only 7.5% of the children had Vitamin D in the normal range. The only study in healthy Indian children reports that ~34.32% of the study population had Vitamin D level in the normal range.[7] This variability in the findings of the two studies could be due to the fact that while the current study deals with Vitamin D level in children and adolescents with psychiatric disorders, and the study by Angurana et al.[7] deals with Vitamin D level in apparently healthy children (65.68% of whom have low [deficiency and insufficiency taken together] Vitamin D level). Not only Indian children but also a substantial population of healthy European children and adolescents are reported to be Vitamin D deficient.[16] It may be speculated that the chances of having normal Vitamin D level decrease when a child develops psychiatric illness, or, in other words, may be, low Vitamin D level adversely affects the brain development, playing a role in the development of psychiatric illness.[1718] Moreover, the findings of 15% of children and adolescents having normal level in the study by Zhang et al.[8] may be comparable given the geographical differences in the two places where the studies were conducted.
Furthermore, a higher percentage of Vitamin D deficiency (80%) in children and adolescents was found in our study compared to the findings of the West, where 21% had Vitamin D deficiency.[8] However, taken together, 92.5% of the study population had low Vitamin D comparable to 85% of the study population in the West.[8] This could be because Indians have reduced the ability for cutaneous Vitamin D synthesis owing to possible differences in Vitamin D binding and degradation; and single nucleotide polymorphisms located in or near genes involved in synthesis, transport, activation, or degradation of Vitamin D may influence serum Vitamin D concentrations.[18] Thus, some authors suggest a higher dose of Vitamin D supplementation in Indian children, more so for extraskeletal benefits.[18]
Although Vitamin D deficiency was prevalent across all diagnostic categories, lower mean Vitamin D level was found for neurodevelopmental disorders (intellectual disability, pervasive developmental disorder, and disturbance of activity and attention). The lowest mean Vitamin D level in the current study was found for pervasive developmental disorders (10.9 ± 7.3 ng/ml), followed by intellectual disability (12.18 ± 8.8 ng/ml). A similar finding is present in the literature reporting the lowest mean Vitamin D level for ASD.[6910] It may be presumed that more is the severity of Vitamin D deficiency, more is the chance that it affects brain development severely, thereby possibly having an important role in neurodevelopmental disorders. Although this has not been appropriately tested statistically in this paper, a similar inference was drawn from the studies reported in a review by Föcker et al. where an inverse relationship is documented between Vitamin D levels and the severity of psychiatric disorders in children and adolescents.[17] No study has specifically looked into Vitamin D level in intellectual disability, to the best of our knowledge. The findings from Vitamin D supplementation trials in children and adolescents suggest a role of Vitamin D in the pathogenesis of mental disorders in childhood and adolescence demonstrating that it may have preventive and therapeutic role including that in ASD.[1418] This study did not look into the role of Vitamin D supplementation.
No gender differences were found in the mean Vitamin D level, although more males had Vitamin D deficiency compared to females and this difference was statistically significant. However, a small number of females in the present study should be kept in mind while interpreting the results. Another interesting finding which emerges is that the neurodevelopmental disorders which are more common in males had lower mean Vitamin D level and more males had Vitamin D deficiency in this study. It may be because, in our study, majority of children had neurodevelopmental disorders. Nonetheless, it may be important for both pediatricians and psychiatrists catering to children with neurodevelopmental disorders to look for Vitamin D deficiency.
The important limitations of the study are as follows: small sample size, retrospective design, absence of control group, lack of detailed information about the comorbid physical illness, reason for requesting Vitamin D level, details about sun exposure, skin color, dietary habits, and nutritional status were not available in case records.
CONCLUSION
The cause-effect relationship between low serum Vitamin D level and children with psychiatric disorders cannot be derived, based on the retrospective study design; however, it provides important initial data from India. Given the finding that only 7.5% of children had normal Vitamin D level, clinicians should have a higher suspicion of low Vitamin D in children, and adolescents with psychiatric disorders. However, in future, large prospective study designs with more controlled variables will allow more precise analysis to determine the prevalence of low Vitamin D, as well as to derive conclusions about the association between low Vitamin D and childhood psychiatric disorders.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Developmental Vitamin D deficiency causes abnormal brain development. Psychoneuroendocrinology. 2009;34(Suppl 1):S247-57.
- [Google Scholar]
- Hypothesis: Is low prenatal Vitamin D a risk-modifying factor for schizophrenia? Schizophr Res. 1999;40:173-7.
- [Google Scholar]
- Implications of a new definition of Vitamin D deficiency in a multiracial us adolescent population: The National Health and Nutrition Examination Survey III. Pediatrics. 2009;123:797-803.
- [Google Scholar]
- Vitamin D deficiency and depression in adults: Systematic review and meta-analysis. Br J Psychiatry. 2013;202:100-7.
- [Google Scholar]
- Correlation between total Vitamin D levels and psychotic psychopathology in patients with schizophrenia: Therapeutic implications for add-on Vitamin D augmentation. Ther Adv Psychopharmacol. 2014;4:268-75.
- [Google Scholar]
- Low serum levels of 25-hydroxyvitamin D (25-OHD) among psychiatric out-patients in Sweden: Relations with season, age, ethnic origin and psychiatric diagnosis. J Steroid Biochem Mol Biol. 2010;121:467-70.
- [Google Scholar]
- Prevalence of Vitamin D deficiency in apparently healthy children in North India. J Pediatr Endocrinol Metab. 2014;27:1151-6.
- [Google Scholar]
- Do children with mental disorders have higher prevalence of hypovitaminosis D? F1000Res. 2013;2:159.
- [Google Scholar]
- Serum concentration of 25-hydroxyvitamin D in autism spectrum disorder: A systematic review and meta-analysis. Eur Child Adolesc Psychiatry. 2016;25:341-50.
- [Google Scholar]
- Vitamin D deficiency and psychotic features in mentally ill adolescents: A cross-sectional study. BMC Psychiatry. 2012;12:38.
- [Google Scholar]
- Reduced serum levels of 25-hydroxy and 1,25-dihydroxy Vitamin D in Egyptian children with autism. J Altern Complement Med. 2010;16:641-5.
- [Google Scholar]
- Vitamin D supplementation during the first year of life and risk of schizophrenia: A Finnish birth cohort study. Schizophr Res. 2004;67:237-45.
- [Google Scholar]
- Core symptoms of autism improved after Vitamin D supplementation. Pediatrics. 2015;135:e196-8.
- [Google Scholar]
- Vitamin D status in autism spectrum disorders and the efficacy of Vitamin D supplementation in autistic children. Nutr Neurosci. 2016;19:346-51.
- [Google Scholar]
- Is high prevalence of Vitamin D deficiency a correlate for attention deficit hyperactivity disorder? Atten Defic Hyperact Disord. 2014;6:73-8.
- [Google Scholar]
- Vitamin D in the healthy European paediatric population. J Pediatr Gastroenterol Nutr. 2013;56:692-701.
- [Google Scholar]
- Vitamin D and mental health in children and adolescents. Eur Child Adolesc Psychiatry. 2017;26:1043-66.
- [Google Scholar]






