Translate this page into:
Clinical Case Presentation on Absence Seizures Diagnosis and Treatment Care Services and Outcomes in an Adult Patient
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Absence seizures are often associated with impaired or loss of consciousness clinically proved to have an impact on motor and cognitive abnormalities of the nerve cells of the brain. Seizure admits several etiopathophysiological events leading to several neurofunctional changes in the reticulothalamocortical circuitry zones of the central nervous system. This paves the episodes of absence seizure events. A clinical case report of absence seizure in a 25 years age adult patient came to the hospital with impaired consciousness. The brain magnetic resonance imaging scanning of the patient detected a small focal flair hypertensive area in the right parasellar region close to cavernous sinus with mild flair hypersensitivity in the left cavernous sinuses, right maxillary, and ethmoid sinusitis. The electroencephalogram of the brain showed normal waves with electrode artifacts was observed. The patient was confirmed with absence seizures, and he was treated with oxcarbazepine 150 mg twice daily. The patient was recovered from seizure and discharged with medications. He was called for follow-up examination once in 3-month period.
Keywords
Absence seizures
artifacts
ethmoid sinusitis
hypersensitivity
impaired consciousness
INTRODUCTION
Seizure is a short episode of abnormal electrical activity in the brain with intense electrical signals.[1] Typically, absence seizure lasts from few seconds to minutes with the loss of consciousness and no any marked convulsions, often occur in children aged <10 years.[12] Absence seizures explicit behavioral arrest, unresponsiveness, cyclic blinking of eyelids, suddenly stopped speech and movement, mouth chewing, lip smacking, and rubbing fingers. The diagnosis includes complete blood count test, brain computerized tomography scan, magnetic resonance imaging (MRI), electroencephalogram, and cerebrospinal fluid examination which provides the evidence and demonstrates clearly the origin of seizure lesions in the brain. The prevention and management of the absence seizure can be done using phenytoin and carbamazepine with the ketogenic diet.[3456]
CASE REPORT
Mr. VA, a 25 year old male patient with an episode of absence seizures, was presented to the general medicine with loss of consciousness lasted for 2–4 min, giddiness, and dimness of vision. The patient reported that he regained from his loss of consciousness after few minutes, however, the giddiness persisted. The patient had no vomiting, involuntary movements, headache, fever, urinary incontinence, and palpitations.
Family history
His family history had that his mother suffered from generalized tonic–clonic seizures and developed intense erythematous patch under the right eye spreading over the right cheek. She took phenobarbitone, iron, and vitamin supplements.
Past medical history details
Mr. VA is a bachelor male with no any history of head injury, neurological illness, and drug abuse. He experienced the episode of absence seizure characterized by loss of consciousness and impaired memory quite sometime in the past 2 years. He said that he remained unresponsive and unable to recall his events after retrieved from the episode and experienced baseline memory disturbances. The patient's past medical history showed no any chronic diseases include diabetes mellitus, hypertension, and cardiovascular problems. Similar to his mother, the patient had intense erythematous patch under the right eye spreading over the right cheek with no numbness or itching.
General examination reports
The patient was conscious, oriented, afebrile, pulse rate of 82 bpm, and with normal respirations. His blood pressure was normal, and the cardiovascular sounds S1 and S2 were normal. The chest X-ray revealed normal, and the electrocardiogram showed no ST-T changes with any sinus rhythm. P/A was soft, no organomegaly and no pallor/icterus/cyanosis/pedal edema were seen.
Hematology laboratory examinations exhibited hemoglobin 14.7 g/dl, packed cell volume 42%, white blood cells 10,300/cum, neutrophils 83%, eosinophils 6%, basophils 2%, lymphocytes 12%, monocytes 2%, red blood cells 4.7 × 106/mm3, erythrocyte sedimentation rate 30/h, mean corpuscular volume 89 fl, mean corpuscular hemoglobin 31 pg/cell, mean corpuscular hemoglobin concentration 35 g/dl, and platelets of 234,000 cells/cum.
Serum electrolytes values were found to be normal. Blood sugar test reported fasting blood sugar was 107 mg/dl, random blood sugar was 170 mg/dl, postprandial blood sugar level was 150 mg/dl, and capillary blood glucose was 84 mg/dl. HbA1C was also found within normal. Liver function test reported that elevated alkaline phosphatase 71 international units/liter, and other parameters were found to be normal. Renal function test detected normal values; however, a slightly elevated uric acid level was found to be l4.3 mg/dl. His cholesterol test revealed all the parameters were found to be normal.
Neurological investigation reports
The patient's central nervous system examination revealed normal higher functions with no motor sensory deficits and bilateral plantar flexor. The electroencephalogram of the brain showed that the electrical waves remained normal with some electrode artifacts confirming the detection of absence seizure [Figure 1].
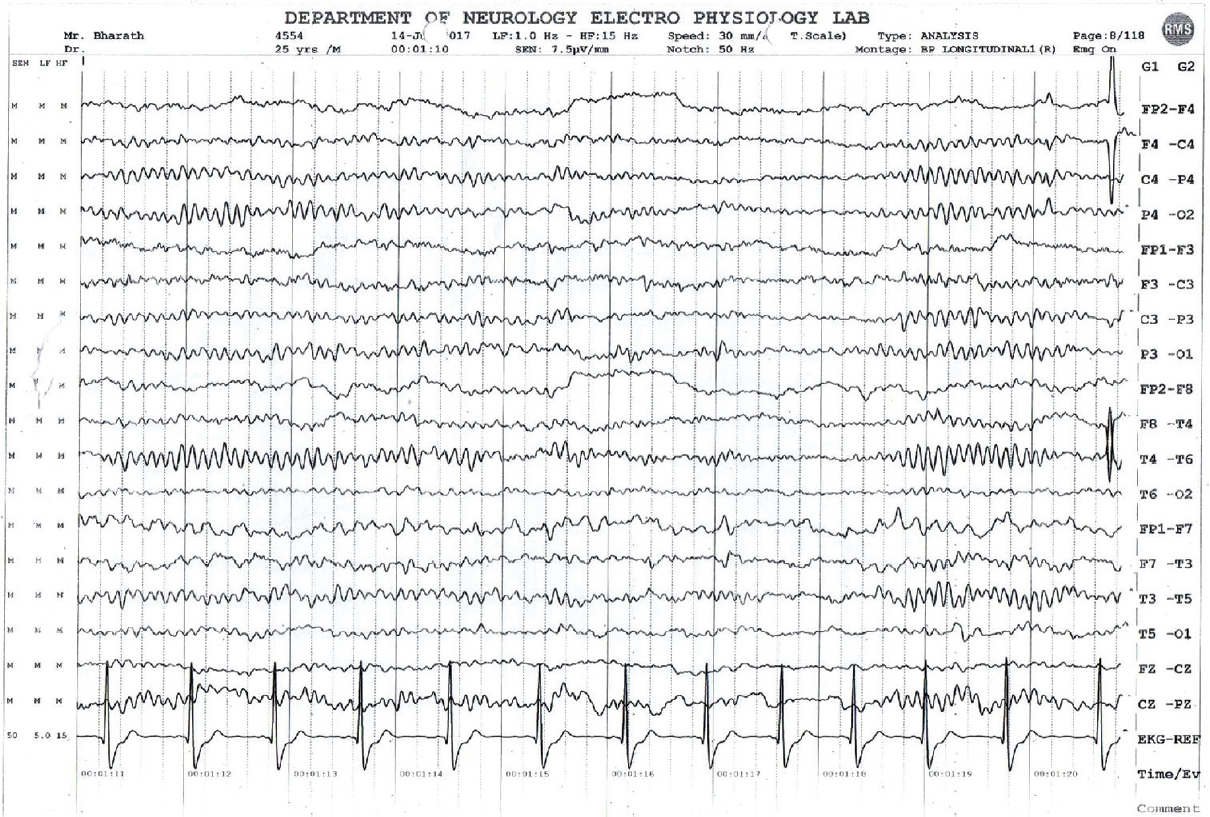
- Electroencephalogram of the brain
The patient's brain MRI scan revealed the presence of small focal flair hypertensive area in the right parasellar region close to cavernous sinus and mild flair hypersensitivity in the left cavernous sinus. The MRI scans also revealed right maxillary and ethmoid sinusitis and no blooming restrictions were noted[7] [Figure 2 and Table 1]. Patient medications chart.

- Magnetic resonance image scan of the brain

DISCUSSION
The above clinical findings and laboratory tests reported that the patient was detected with the episodes of absence seizures. In the case, the patient was presented with absence seizures which progressively associate with temporary loss of consciousness.[8] The etiology represented that there was an increase in the cerebral blood flow, increased intracranial pressure which ultimately provokes the development of seizure; it was evident in the case of Mr. VA. The patient's pathophysiology revealed neuronal changes which led to changes in the reticulothalamocortical circuitry which may be associated with genetic liability exhibiting absence seizure.[9] Patient has not incurred any kind of symptoms in his childhood, however it was manifested recently. A study by Avanzini et al., showed an increased oscillatory activity in the reticulothalamocortical circuitry proved to be the cause for the absence seizure which has made a promising diagnostic tool in this patient.[910]
Since the patient's mother had seizure and had not underwent any proper treatment which may be due to the economic status which may be the reason conjoined with genetic liability in this case.[11]
As reported by Thomas et al. sudden withdrawal of drugs, such as diazepines, psychotropic, antidepressant drugs, autoimmune diseases, brain accidents, and electrolyte disturbances being a factor which imposes the incidences of absence seizures.[56789101112]
After 1 week of hospital stay, the patient was treated with the drugs as shown in Table 1. He was thoroughly monitored and found that his vital signs were normal. He responded well to the medications, and diet intake was normal. He showed positive improvement in his conditions and showed no further seizure incidences. The patient was advised for stress management, adequate rest, and regular sleeping with healthy diet. The patient was asked for a follow-up every 3 months, and he was then discharged from the hospital.[21314] On his first follow-up visit, he was quite normal and taken the discharge medications regularly, and he reported no any new episode of seizures. An effective preventive measure toward the patient's health status can prevent the risk factors which ultimately improves better quality of life, as reported by Nutthaya Vongkasamchai et al.[15]
CONCLUSION
The pathophysiological mechanisms underlying epilepsy are autism spectrum disorder (ASD) resistance and sudden ASD dose reduction can trigger withdrawal response of seizure; hence, dose reduction or removal should be done gradually. Effective understanding of pathophysiological mechanisms, drug targeting, antiepileptogenesis, and genetics can provide a better understanding of epilepsy and its management. New molecular drug target, pharmacogenomics, and documentation of the individual patient's report can improve the treatments effectively.[1617]
Clinical pharmacist should be positioned in the clinical practice to identify the risk factors for seizure origin, early diagnosis, and treatment can reduce the healthcare cost. Initiating awareness programs on disease prevention and management, regular patient follow-up care, and medication adherence can reduce the individual's disease burden and hospital revisit which can ultimately promote health-related quality of life. Regular implementation of these practices among healthcare team can reduce the individual's healthcare cost and hospital revisit.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to thank Dr. K.S. Lakshmi, Dean, SRM College of Pharmacy, SRM Institute of Science and Technology, for her encouragement and support.
REFERENCES
- Review article: Convulsive and non-convulsive status epilepticus: An emergency medicine perspective. Emerg Med Australas. 2009;21:352-66.
- [Google Scholar]
- Voltage-gated calcium channels in the etiopathogenesis and treatment of absence epilepsy. Brain Res Rev. 2010;62:245-71.
- [Google Scholar]
- Absence status epilepsy: Delineation of a distinct idiopathic generalized epilepsy syndrome. Epilepsia. 2008;49:642-9.
- [Google Scholar]
- ‘De novo’ absence status of late onset: Report of 11 cases. Neurology. 1992;42:104-10.
- [Google Scholar]
- Typical absence status epilepticus as late presentation of idiopathic generalized epilepsy in an elderly patient. Seizure. 2009;18:82-3.
- [Google Scholar]
- Absence status epilepsy: Delineation of a distinct idiopathic generalized epilepsy syndrome. Epilepsia. 2008;49:642-9.
- [Google Scholar]
- Recurrent absence status epilepticus: Clinical and EEG characteristics. Seizure. 2002;11:310-9.
- [Google Scholar]
- Cortical versus thalamic mechanisms underlying spike and wave discharges in GAERS. Epilepsy Res. 1996;26:37-44.
- [Google Scholar]
- Evolving concepts on the pathophysiology of absence seizures: The cortical focus theory. Arch Neurol. 2005;62:371-6.
- [Google Scholar]
- High-frequency changes during interictal spikes detected by time-frequency analysis. Clin Neurophysiol. 2011;122:32-42.
- [Google Scholar]
- Absence status in the adult. New results including computerized transverse axial tomography. Eur Neurol. 1978;17:121-8.
- [Google Scholar]
- De novo absence status of late onset: report of 11 cases. Neurolog. 1992;42:104-10.
- [Google Scholar]
- Absence and myoclonic status epilepticus precipitated by antiepileptic drugs in idiopathic generalized epilepsy. Brain. 2006;129:1281-92.
- [Google Scholar]
- Prevalence of provocative seizures in persons with epilepsy: A longitudinal study at Khon Kaen University Hospital, Thailand. Neurol Res Int 2015 2015 659189
- [Google Scholar]
- Sleep, epilepsy and thalamic reticular inhibitory neurons. Trends Neurosci. 2005;28:317-24.
- [Google Scholar]
- Absence status in the elders as a late complication of idiopathic generalized epilepsies. Epileptic Disord. 2007;9:39-42.
- [Google Scholar]






