Translate this page into:
See-Saw Relationship and its Reversal after Immunotherapy in a Case of Graves’ Disease with Coexisting Myasthenia Gravis
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The unique association of myasthenia gravis (MG) with Graves’ disease in clinical practice emphasizes that one autoimmune disease can coexist with another or many. The relationship between these two entities has remained controversial till date. Some authors have reported a see-saw relationship between these two entities, MG waning with hyperthyroidism and waxing with treatment of hyperthyroidism. Treatment of both these disorders concurrently may be challenging at times as treatment for one entity may worsen the other. The use of beta-blockers and steroids for Graves’ disease may worsen myasthenic weakness. Antithyroid drugs can worsen myasthenia probably by immunomodulatory effects. We report a case of Graves’ disease coexisting with MG in a reciprocal relationship which was subsequently reversed after immunotherapy.
Keywords
Antithyroid drugs
Graves’ disease
myasthenia gravis
seesaw
INTRODUCTION
The association of thyrotoxicosis and myasthenia gravis (MG) was first described in 1899 by Remak, and subsequently in 1908, Rennie described a similar association.[1] The see-saw relationship (i.e., treating thyrotoxicosis worsens myasthenia) between these two entities was described by McEachern and Parnell[2] in 1948. In 1954, Maclean and Wilson observed a similar relationship.[3] Some clinicians (Kowallis et al., 1942; Carson and Keynes, 1942; Sheldon and Walker, 1946; Millikan and Haines, 1953; Silver and Osserman, 1957)[4] experienced either reverse seesaw or no interaction between these two entities. The exact relationship is still obscure and variable.
CASE REPORT
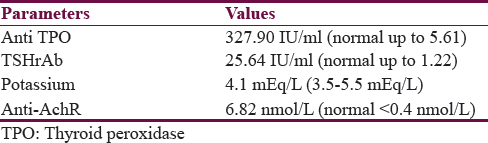
A 45-year-old fisherman was admitted for bilateral proptosis, redness of both eyes, and excessive tearing for a month. He also had a significant weight loss, profuse sweating, and frequent loose stools. On examination, he had complete external ophthalmoplegia with a clinical activity score (CAS) of 7 and diffusely enlarged goiter. His free T3 (28.63 pg/ml) and free T4 (>7.7 ng/dl) were high with suppressed TSH (0.003 mIU/ml) [Table 1]. The patient was diagnosed to have Graves’ disease, and antithyroid drugs were started (carbimazole 10 mg tid and propranolol 40 mg bd for attenuating sympathetic overactivity (heart rate 118/min, palpitations, and profuse sweating). After 2 weeks of antithyroid drug treatment, he developed dysphagia, hoarseness of voice, nasal speech, and proximal muscle weakness of both upper and lower limbs which worsened toward the evening, and these symptoms were not present at the time of admission. Apart from the features of thyrotoxicosis, the patient had partial ptosis and symmetric proximal weakness of all four limbs in the Medical Research Council Grade of 4 [Figure 1]. Tone was normal, and deep tendon reflexes were elicited normally. Although gag sensation was intact on both sides, he had diminished palatal movements. As these clinical features suggested coexisting MG repetitive nerve stimulation (RNS) of facial muscles was done which showed decremental response. Neostigmine drug trial was also given which turned out to be positive. He scored 21 out of 39 in quantitative MG (QMG) on initial evaluation. His complete blood count and renal and liver profile were within normal range. His potassium and creatine phosphokinase levels were normal. Antithyroid peroxidase and thyrotropin receptor antibodies were positive. Antiacetylcholine receptor antibody was in the range of 6.82 nmol/L (normal <0.4 nmol/L). His computed tomography of thorax did not show thymic enlargement along with carbimazole and pyridostigmine 60 mg 6th hourly was started while propranolol was stopped in view of its potential to worsen myasthenia. Prednisone was started in a low dose of 20 mg per day for immunosuppression in myasthenia.

- The patient with thyrotoxicosis features
Despite the therapy, his symptoms steadily worsened to imminent myasthenic crisis, and his QMG score was 27 at this time. Prednisone was withheld, and intravenous (iv) immunoglobulin was given in the dose of 0.4 g/kg/day for 5 days. After immunotherapy, the patient QMG score improved to 16 [Figure 2]. He showed further improvement after reduction in carbimazole dose to 5 mg tid and his QMG score improved to 11. His thyroid eye disease symptoms also improved with a CAS of 2. After 1 month of immunotherapy, carbimazole was re-escalated to 10 mg thrice daily without any worsening of myasthenic symptoms. Carbimazole has the potential for worsening myasthenia and hence initially dose was reduced. However, after immunotherapy, we were able to escalate the carbimazole dose without worsening of myasthenia.

- After treatment with antithyroid drugs and immunotherapy
DISCUSSION
The coexistence of Graves’ disease with MG is known for more than a century. The exact relationship between these two entities is yet unclear. It is said to be a common genetic mechanism operating between these two and a common autoimmune target in ocular muscles. HLADQ3 was found to have a coexistence in 5 out of 6 patients with both these entities in a Japanese study.[5] Chemokine C-X-C motif ligand 10 along with its receptor (C-X-C motif) receptor 3 amplifies host immune response that perpetuates the autoimmune process.[6] Two to three percent of Graves’ suffer from MG whereas two to seventeen percent of MG can have Graves’.[7]
Variable time of occurrence of these entities was reported. The occurrence of thyrotoxicosis followed by myasthenia was noted in 48%, simultaneous onset in 20%, and MG followed by Graves’ in 32%.[8] Unpredictable disease fluctuations with the routine treatment protocols were also reported. We experienced see-saw phenomenon in our patient as described by McEachern and Parnell.[2] Worsening of myasthenic symptoms with the treatment of thyrotoxicosis, i.e., the see-saw phenomenon was also observed in our case. We believe antithyroid drugs unmasked the underlying MG.
The exact mechanism of the see-saw phenomenon is unclear. Antithyroid drugs methimazole and carbimazole exhibit additional immunomodulatory effect apart from suppressing thyroid hormone production. Proliferating cell nuclear antigen (PCNA) is a protein molecule that regulates cell apoptosis. Cells with low PCNA undergoes apoptosis. Methimazole and carbimazole decrease PCNA predisposing cells for destruction.[9] In our case, we suspected carbimazole-induced worsening as he showed marked improvement with decrease in dose. Usage of corticosteroids,[10] beta-blockers,[11] and benzodiazepines in thyrotoxicosis can also affect neuromuscular transmission and worsen myasthenic symptoms. Ocular signs can create diagnostic confusion in cases of concomitant MG in Graves’.[12] In other words, emergence of neuromuscular and bulbar symptoms during the treatment of thyrotoxicosis should alert the physician to suspect coexisting MG.
In our case, myasthenic symptoms surfaced after adding antithyroid drugs and led to imminent myasthenic crisis. After iv immunoglobulin therapy, the symptoms of MG stabilized. Re-escalation of antithyroid drug after immunotherapy did not produce any worsening of myasthenia. This shows that immunotherapy has reversed the see-saw relationship which we experienced initially.
Thyrotoxic myopathy, a close differential diagnosis, is relatively rare compared to MG. The absence of diurnal variation, negative RNS study, absence of response to neostigmine, and bulbar symptoms of lesser severity are some features that help to distinguish it from MG. Thyrotoxic myopathy and thyrotoxic hypokalemic paralysis (more common in Asians) are to consider along with MG in a case of muscular weakness in the background of thyrotoxicosis.
CONCLUSION
Coexistence of MG should be suspected if neuromuscular weakness is encountered during the treatment of thyrotoxicosis. Close monitoring is required when treating such patients with antithyroid drugs, steroids, benzodiazepines, beta-blockers, and dose adjustments may be needed. We experienced the see-saw relationship described in literature and its reversal following immunotherapy in our patient. In case of a reciprocal relationship scenario like ours, one can resort to immunotherapy like iv immunoglobulin which will help in optimizing antithyroid drugs. We report this case for the rarity of the association and therapeutic intricacies when treating these entities concurrently.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Myasthenia gravis associated with Graves’ disease in Japan. Jpn J Med. 1987;26:2-6.
- [Google Scholar]
- The relationship to hyperthyroidism to myasthenia gravis. J Clin Endocrinol Metab. 1948;8:842-50.
- [Google Scholar]
- See-saw relationship between hyperthyroidism and myasthenia gravis. Lancet. 1954;266:950-3.
- [Google Scholar]
- Reverse ‘see-saw’ relationship between Graves’ disease and myasthenia gravis; clinical and immunological studies. J Med Dent Sci. 2005;52:43-50.
- [Google Scholar]
- Grave's disease associated with myasthenia gravis: a case report. Intern Med Inside. 2014;2:4.
- [Google Scholar]
- Harrison's Principles of Internal Medicine. Myasthenia Gravis and Other Disorders of Neuromuscular Disorder. (19th ed). Newyork City: McGraw-Hill Publishing Company; 2015. p. :2701.
- [Google Scholar]
- The thyroid gland in relation to neuromuscular disease. AMA Arch Intern Med. 1953;92:5-39.
- [Google Scholar]
- Effect of orally administered antithyroid thioureylenes on PCNA and P53 expression in psoriatic lesions. Int J Dermatol. 1995;34:280-3.
- [Google Scholar]
- Prednisone-induced worsening of neuromuscular function in myasthenia gravis. Neurology. 1986;36:729-32.
- [Google Scholar]
- Hickam's dictum: Myasthenia gravis presenting concurrently with Graves’ disease. BMJ Case Rep 2017 2017 pii: bcr-2017-220153
- [Google Scholar]






