Translate this page into:
Collaborative Tele-Neuropsychiatry Consultation Services for Patients in Central Prisons
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Tele-medicine helps to provide clinical care comparable to in-person treatment in various clinical settings. It is a novel system of healthcare delivery in both low-resource settings and sites where adequate medical care continues to pose greatest challenge like in prison's in India and worldwide.
Aim:
To study the sociodemographic and clinical profile of patients from Central Prisons, having received collaborative Tele-Neuropsychiatric Care.
Methodology:
Psychiatry, neurology, and neurosurgery specialists provided tele-neuropsychiatry consultation through Specialist–Doctor–Patient model as part of the state-run program for the two central prisons from July 1, 2014, to June 30, 2016. A retrospective file review was done of the tele-neuropsychiatry case records at Tele-Medicine Centre, Located at Tertiary Neuro Psychiatric centre of South India.
Results:
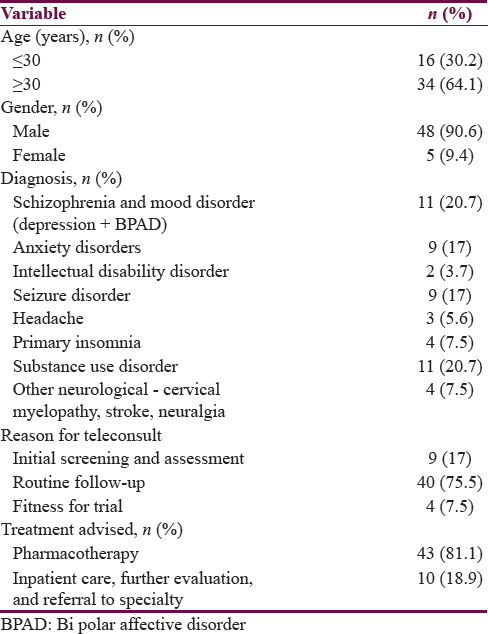
A total of 53 patients were provided tele-neuropsychiatric consultation over 2-year period. Of these, 48 (90.6%) were male and 34 (64.1%) were aged more than 30 years. In total, 20.7% of them had severe mental illness, i.e., schizophrenia and mood disorders, 20.7% with substance use disorder (alcohol and cannabis), 17% had anxiety disorders while 17% with seizure disorder. Nearly 81.1% of patients (inmates) were advised pharmacotherapy while 18.9% were suggested further evaluation of illness and inpatient care at the higher center.
Conclusion:
The collaborative care was successful in delivering psychiatry, neurology, and neurosurgery consultation with a Specialist–Doctor–Patient model to prison inmates.
Keywords
Mental health
prison
Specialist–Doctor–Model
Tele-Psychiatry
Tele-Medicine
INTRODUCTION
In India, the prison population has been steadily increasing in the last decade. A majority of the prison population are male, and approximately, two-thirds are pretrial detainees. Officially 277,304 prisoners can be housed in 1276 establishments throughout the country; however, as of 2007, the prisons accommodated 376,396 inmates, contrary to the official capacity (representing an occupancy rate of 135.7%).[1] Therefore, along with overcrowding, adequate medical care continues to be the greatest challenge in prisons in India. As per the recent report by Institute for Criminal Policy Research (ICPR) and National Crime Records Bureau (NCRB) 2015, the Indian prison population is estimated to be around 419,623.[1]
A recent study from South India by Kumar et al. showed one-third had normal health status, but the majority of them, i.e., 63.6% had a morbid health condition. In addition, they found that 84% had anemia, 18% with ascariasis, 14.6% suffered respiratory tract infections and 8.7% with musculoskeletal and connective tissue disorders.[2] Similar to the high prevalence of medical illness, mental illness (MI) was also noted to have an equally greater prevalence among inmates of prisons. Furthermore, a few countries have a greater number of mentally ill patients in prisons than in psychiatric hospitals.[345678]
There are few studies from India assessing the prevalence rate of psychiatric illness among detainee's in prison. A study from central jail Amritsar found that the current prevalence of psychiatric illness among the convicted prisoners to be 23.8% after excluding substance abuse. Among these, prisoners 56.4% were having a history of substance abuse/dependence before incarceration and the most common substance of abuse was alcohol.[5] Similarly, in another study from Kota central jail, the prevalence of psychiatric disorders after excluding substance use was found to be 33%.[3] A recent study from Kozhikode District Jail revealed 21.5% having psychiatric illness and 47.1% with substance use disorder (SUD).[9] In all above three studies (representing different regions of the country), SUD surfaced to be the most common diagnosis, followed by Anxiety Disorder and Depressive Disorders.[359] However, the above independent study findings are not in line with NCRB (India) 2015 Report, which discloses only 5,203 inmates with an MI out of 419,623, i.e., only 1.2% of the total inmates suffered a psychiatric ailment.[1] This is most probably due to selective reporting of severe MI, which are on treatment and may not have taken into account SUD and common mental disorder.
As MI is found to be higher in prison inmates than the general population the etiology is multifaceted.[5] It ranges from environmental stress; psychosocial factors to substance use.[678] In addition, studies have consistently shown a significant treatment gap and delay in referral when it comes to seeking medical help and/or psychiatric evaluation for prisoners.[10] This is probably due to lack of resource, overcrowding in prisons, and deficient workforce to address the needs.
Treatment gap in prison can be reduced using an effective tool like tele-medicine as suggested from previous literature. Tele-medicine care provides clinical services which are comparable to the in-person treatment in various clinical settings. It is a novel system of health care delivery in low-resource settings with low cost to care. A recent study finding from a Government-run Tele-Medicine center showed that tele-neurorehabilitation services were feasible, effective, and less resource intensive in delivering quality tele-medicine care.[11]
It is on this background that the Tele-Medicine Centre at National Institute of Mental Health and Neuro Sciences (NIMHANS), Bengaluru, had started providing tele-psychiatry, tele-neurology, tele-neurosurgery services from July 1, 2014, to June 30, 2016, to the inmates of two central prison through Karnataka State Wide Area Network (KSWAN). The aim of this study was to review the sociodemographic and clinical parameters of inmates from these Central Prisons, who had received collaborative tele-neuropsychiatric care over a 2-year period.
METHODOLOGY
Study population
We conducted a retrospective case file review of tele-neuropsychiatric services from July 1, 2014, to June 30, 2016, at Tele-Medicine Centre, located at Tertiary Neuro Psychiatric centre of South India.
Data collection
The files were retrieved from both tele-records of tele-medicine center and medical records department. An average of 15–30 min was spent to extract data from each case file.
Model of tele-neuropsychiatry service
Tele-neuropsychiatry service was provided through Hub and Spoke Model using electronic health record-based, synchronous video conference mode. It is a collaborative-care model, where a medical officer from the central prison (Spoke Centre), who desires to seek tele-neuropsychiatry consultation from specialists of Psychiatry/Neurology/Neuro-Surgery from Tertiary Neuro Psychiatric centre of South India for the inmates would contact the tele-medicine technician at tele-medicine center. The basic sociodemographic and clinical details of patients (inmates) would then be entered in their Electronic Health Record maintained through KSWAN. The technician would then fix an appointment based on the availability of specialist at (Hub Centre). The patients were then seen or discussed with respective central prison medical officer in live, real-time video conference mode. The average time for a single consultation ranged from 15 to 20 min. The central prison doctors would then provide treatment to their central prison patients based on the consensus drawn at the end of the consultation.
Ethical considerations
The Institutional Ethical Committee of NIMHANS, Bengaluru, has approved the study.
Statistical analysis
Sociodemographic and clinical parameter were analyzed using descriptive statistical methods.
RESULTS
A total of 53 patients received tele-neuropsychiatric consultation over a 2-year period. Table 1 describes the demographic and clinical profile of patients who received outpatient-based collaborative tele-neuropsychiatry consultations. 48 (90.6%) were male while the majority, 34 (64.1%) were aged more than 30 years. Overall, 20.7% of them had schizophrenia and mood disorders, 20.7% had SUD (alcohol and cannabis), 17% with anxiety disorders, and 17% had a seizure disorder. All of the consultations were found useful, with 81.1% of patients (inmates) being advised pharmacotherapy while 18.9% were suggested further evaluation of illness and inpatient care at the higher center.
DISCUSSION
To the best of our knowledge, this study represents the first collaborative tele-neuropsychiatric service given to prison population in India. The majority of patients (inmates) who sought collaborative tele-neuropsychiatric care were male aged more than 30 years. This study has been conducted during the same period as National Prison data of 2015. Hence, the sample is representative of the National (India) Prison inmate data where 4,01,789 (95.7%) were male while only 17,834 (4.3%) were female.[1] In the study, the most common reason for tele-consultation was worsening/recurrence/relapse of symptoms only to be seconded by routine follow-up. Schizophrenia, mood disorders, SUD (alcohol and cannabis), anxiety disorders, and seizure disorder were the common diagnoses made. Interestingly, 81.1% were advised pharmacotherapy, and only 18.9% were advised for further evaluation of illness and inpatient care at a higher center. Our findings are in line with the literature review on the prevalence of psychiatric illness across prisons from Indian central jails[359] and worldwide.[1213]
Our center used the Specialist–Doctor–Patient model. This model has been more feasible in delivering tele-psychiatry, neurology, and neurorehabilitation consultations in our center. A similar model has been reported to be successful in another center in India.[14] The prison Medical officers found this tele-collaborative Specialist–Doctor–Patient model as a useful prototype of care. The collaborative tele-psychiatry and neurology service have been unevenly distributed throughout different districts of Karnataka. This is a reflection of the poor utilization of tele-medicine services in our country.[15]
Our study strengthens the international literature for feasibility and acceptability of tele-psychiatry service for prison and correctional centers. A review from Deslich et al. highlighted increasing the access to mental healthcare for the underserved group through tele-psychiatry, which would improve living conditions and safety inside correctional facilities, in turn, have health economic benefits.[1617] Another review by Young and Badowski in 2018 concluded that the use of telemedicine technologies could remove barriers and help in increasing access to high-quality multidisciplinary care.[18]
As per ICPR Institute for Criminal Policy Research and NCRB 2015, 360 prison inmates escaped in one-year period; among these 272 were outside the prison set up during run off under police custody.[1] This emphasizes the need for high-level security and vigilance by escorts during the patient assisted travel/transport of these inmates to the medical care facility or tertiary care centers. These problems can be addressed by creating hospital-based service inside the central prison and hosting weekly consultations from each specialty based on the needs of the prison patients. Alongside, advanced technology-like telemedicine can further provide these underprivileged with optimum and fundamental healthcare. Literature proposes the following as barriers to health for prisoners: (a) tendency to escape during travel by prison inmates, (b) the cost of security (escorts for patient assisted travel), (c) need for vigilance, etc., These can be overcome or minimized using tele-medicine thus lessening the police workforce requirement during transport and saving the travel expense while bettering the ease of specialist accessibility and reducing the waiting time for consultation.[1819] These barriers were identified and agreed on by medical officers of central prison of Karnataka and acknowledge overcoming this by collaborative tele-neuropsychiatry services.
A review by Deslich et al. on Telemedicine services remarked that the prison system is an ideal setting for offering telepsychiatry facility. The study concludes that it is more economical as a model with an added advantage of reducing the risk of absconding in prison and correctional settings in following states such as Arizona, California, Georgia, Kansas, Ohio, Texas, West Virginia, and Texas.[1617] A recent retrospective study from India also found that telepsychiatry is an economically better model than regular outpatient model providing services to unreached special populations.[20]
Despite the promising advantages, still, some drawbacks curb the widespread use of telemedicine model in prison which includes (a) lack of acceptance to this model, both by patients and healthcare professionals, at spoke side as a replacement for an in-person consultation, (b) conflicting view on virtuality versus reality interphase-based consultation, (c) technical difficulties faced in connecting hub with spoke center, (d) inadequate training and lack of availability of skilled workforce, (e) disputed primary legal responsibility in cases of medico-legal issues, (f) uncertain policy on confidentiality of patient information during web consultation and (g) storage of relevant audiovisual telemedicine data.[21]
Future direction
This novel model can be used by other prison and correctional institute in both developing and developed countries. There is a need for TeleMedicine Act regarding rules and regulations for tele-consultations, patient's selection criteria, ethical and legal obligations, confidentiality, and international teleconsultations.
CONCLUSION
The collaborative care was successful in delivering psychiatry, neurology, and neurosurgery consultation with a Specialist–Doctor-Patient model to prison inmates.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Prison Statistics India – 2015, National Crime Records Bureau. Ministry of Home Affairs. Available from: http://www.ncrb.gov.in/StatPublications/PSI/Prison2015/Full/PSI-2015-%2018-11-2016.pdf
- Health status of the prisoners in a central jail of South India. Indian J Psychol Med. 2013;35:373-7.
- [Google Scholar]
- Mental health of prisoners: Prevalence, adverse outcomes, and interventions. Lancet Psychiatry. 2016;3:871-81.
- [Google Scholar]
- Minds Imprisoned: Mental Health Care in Prisons. Bangalore: National Institute of Mental Health & Neuro Sciences Publication Supported by Karnataka State Legal Service Authority; 2011. p. :3-50.
- Mental health and substance use problems in prisons. The Bangalore Prison Mental Health Study: Local Lessons for National Action. Bangalore: Nimhans Publication Supported by Karnataka State Legal Service Authority. 2011:84-104.
- [Google Scholar]
- 2005. World Health Organization Information Sheet: Mental Health and Prisons Substance. 39:1-7. Available from: http://www.who.int/mental_health/policy/mh_in_prison.pdf
- The treatment of persons with mental illness in Prisons and Jails: A State Survey. United State of America - 2012: Treatment Advocacy Center. 2014. :1-116. Available at https://www.ncjrs.gov/App/Publications/abstract.aspx?ID=268468
- [Google Scholar]
- Feasibility and utility of tele neuro rehabilitation service in India – Experience from a quaternary center. J Neurosci Rural Pract. 2018;9:541-4.
- [Google Scholar]
- Prevalence of mental illnesses in US state prisons: A systematic review. Psychiatr Serv. 2014;65:862-72.
- [Google Scholar]
- Telepsychiatry in Chennai, India: The SCARF experience. Behav Sci Law. 2008;26:315-22.
- [Google Scholar]
- Karnataka state telemedicine project: Utilization pattern, current, and future challenges. Indian J Psychol Med. 2013;35:278-83.
- [Google Scholar]
- telepsychiatry in the 21st century: Transforming healthcare with technology. Perm J. 2013;17:80-6.
- [Google Scholar]
- Telepsychiatry in correctional facilities: Using technology to improve access and decrease costs of mental health care in underserved populations. Perm J. 2013;17:80-6.
- [Google Scholar]
- Telehealth: Increasing access to high quality care by expanding the role of technology in correctional medicine. J Clin Med. 2017;6:pii: E20.
- [Google Scholar]
- Telepsychiatry as an economically better model for reaching the unreached: A Retrospective report from south india. Indian J Psychol Med. 2017;39:271-5.
- [Google Scholar]
- Tele-psychiatry: After mars, can we reach the unreached? Indian J Psychol Med. 2015;37:120-1.
- [Google Scholar]






