Translate this page into:
Cervical Intramedullary Cystic Teratoma with Dermal Sinus Tract: A Case Report and Review of Literature
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Intramedullary spinal teratomas are rare. We report a case in a 40-year-male who presented with progressive weakness over the right side of the body and gait imbalance. He had dermal sinus with hair patch over nape of the neck. Magnetic resonance imaging revealed cervical (C4–C7) intramedullary tumor with dermal sinus tract. C3–C7 laminectomy was performed and tumor excised along with the sinus tract. Histopathological examination revealed mature cystic teratoma. Gait ataxia was improved immediately while near complete recovery in motor power was achieved over a period of 2–3 weeks.
Keywords
Dermal sinus
spinal dysraphism
spine tumor
teratoma
INTRODUCTION
Teratomas are tumors of multipotent cells that recapitulate normal organogenesis, producing tissues that represent a mixture of two or more germinal layers of ectoderm, endoderm, and mesoderm. They account for approximately 0.1%–0.5% of spinal tumors[12] and are classified as mature, immature, or malignant based on the degree of differentiation. They are intradural lesions and commonly occur in the thoracic and lumbar regions and are solid in nature. Only seven cases of cervical intramedullary teratoma have been reported.[3456789] Cervical intramedullary mature cystic spinal teratoma with congenital dermal sinus has not been reported. We report clinical, radiological, operative, and histopathological findings and review literature on the subject.
CASE REPORT
A 40-year-old male presented with progressive distal weakness and sensory complaints over the right upper and lower limb for 3 years. He also developed gait imbalance since 1 year. On physical examination, there was a dermal sinus with a hair patch over C5 spinous process. Neurological examination showed spastic quadriparesis (right > left). Deep tendon reflexes were brisk, while superficial reflexes were absent. Hypoesthesia was noticed below C4 dermatomes bilaterally with reduced vibration and position sense. Magnetic resonance imaging (MRI) revealed 2.5 cm × 1.5 cm × 2 cm size contrast-enhancing intramedullary mass between fourth and seventh cervical levels. The lesion appeared hypointense on T1-weighted images and hyperintense on T2-weighted images. There was a dermal sinus tract extending from the surface down to the lesion at the level of C5 vertebral body [Figure 1a–d]. Patient underwent excision of intramedullary space-occupying lesion in prone position. Cervical spine explored through vertical midline incision from C2 to T1, surrounding the dermal sinus which was entering intraspinally through the bifid C5 spinous process and lamina. Furthermore, C4 as well as C3 spina bifida observed. C3–C7 laminectomy performed. Dura opened in the midline, around the sinus tract which was extending intradurally at the level of C5. Yellowish white avascular lesion was seen. Dermal sinus tract was almost going inside the lesion at C5 level. Lower part of the lesion appeared as extramedullary, but surprisingly there was no plane of cleavage between the lesion and the cord parenchyma. Cystic lesion was entered and yellowish white thick liquid fluid drained out from it. Cyst wall which was in continuity with dermal sinus was excised. Part of the cyst wall adherent to the cord parenchyma was left untouched. Cyst content, cyst wall as well as dermal sinus tract sent for histopathological examination. At the end, very thinned out, pulsatile cord parenchyma observed along with horizontally traversing cervical nerve roots very much close to the margin of the inner cyst wall. Histopathological examination of the cyst wall/sinus tract showed skin with adnexal structure, respiratory epithelium, cartilage muscle adipose tissue, cerebral tissues as well as psammoma bodies [Figure 2a–d]. As the tumor included elements of all the three germinal layers and did not show cytological evidence of malignancy, the final diagnosis of a benign mature cystic teratoma was made. Postoperatively, gait ataxia improved immediately while near complete recovery in motor power achieved over a period of 2–3 weeks.
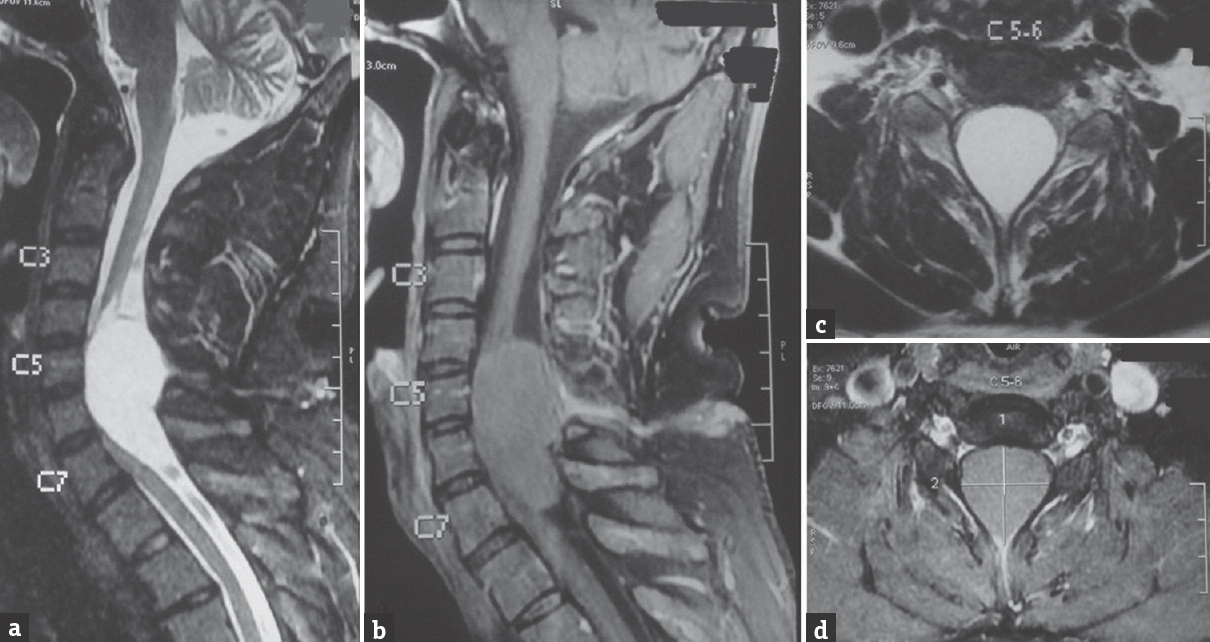
- (a) Magnetic resonance imaging of cervical spine T2-weighted sagittal view showing a 2.5 cm × 1.5 cm × 2 cm intramedullary mass lesion extending from C4 and C7 level and a dermal sinus tract extending from the skin surface to the lesion at the level of C5 vertebrae. (b) Magnetic resonance imaging of cervical spine T1-weighted sagittal view showing a contrast nonenhancing mass with a contrast-enhancing dermal sinus. (c) Magnetic resonance imaging of cervical spine T2 weighted axial view showing an intramedullary mass. (d) Magnetic resonance imaging of cervical spine post contrast axial view showing an intramedullary mass

- Hematoxylin-eosin-stained section showing typical histological appearances. (a) Cartilage (b) epidermis with eccrine glands (c) hair follicle with adipose tissue (d) sebaceous glands
DISCUSSION
Teratomas are uncommon spinal tumors.[2] The usual locations are extradural and intradural extramedullary. However, intramedullary spinal teratomas are rare in adults[6] The thoracolumbar region of the spinal cord is the most commonly affected site in adults.[5] Only eight cases of cervical intramedullary teratoma have been reported [Table 1], each with an absence of any congenital dermal sinus.[3456789] Amongst them, one was extensive, extending from the medulla to the L2 level. Ak et al. reported a lesion in the upper cervical cord at the C2–3 level,[6] and in the other two cases, the lesions were located in the lower cervical segments at the levels of C6–T1. In the available literature, we found a single case of cervical teratoma with congenital dermal sinus with an extramedullary location in which a complete excision of the lesion was possible.[10] Several hypotheses have been proposed for the origin of spinal cord teratomas. The most widely accepted theory is a misplacement of pluripotent embryonic cells into the dorsal midline during their normal migration from the primitive yolk sac to the gonadal ridges.[6]

The typical location of most central nervous system teratomas in midline structures supports the theory that they originate from pluripotent cell rests at the sites of early neural tube closure. In addition, there is a well-known association of spinal cord teratomas with dysraphic congenital spinal malformations such as spina bifida, dermal sinus, split cord, meningomyelocele, lipomeningomyelocele, syrinx, and thickened terminal filum.[11] This association suggests that a developmental fault arose during embryogenesis related to dysfunction of several factors that probably involve genetic and cellular inductive interaction.[7] There may be a cause-and-effect relationship between spinal cord malformation and the migration of pluripotent cells that get entrapped in an abnormal environment and lead to teratoma formation.
One of the associations, dermal sinus tracts, is an uncommon form of spinal dysraphism often presenting in childhood with skin findings, neurologic deficit, or infection and results from dysfunction during fetal development. Normally, between the 3rd to 8th week of gestation, the ectoderm that gives rise to the skin and dermal appendages separates from the neuroectoderm that gives rise to the spinal cord. This process, referred to as disjunction, allows for the insertion of mesoderm, which then forms the vertebral column and underlying musculature that separates the skin from the spinal cord. When a focal failure of disjunction occurs, a persistent connection, or tract, between the skin elements and the underlying neural structures is established. This tract is lined by stratified squamous epithelium encased in dermal tissue and terminates on or near neural structures.[8] The disjunction theory supports Mount's observation in 1949 that the dermatomal level of the defect often corresponds to the neural level of the central nervous system structures with which the tract communicates.[11]
There are no specific clinical or radiological features for the preoperative diagnosis of these lesions. However, several authors have reported clinical features including weakness of the leg, sensory changes, reflex abnormalities, and urinary incontinence which are related to the location of the tumors.[10] The operative findings revealed that the degree of spinal cord compression by the mass was severe. However, the patient's neurological symptoms were not severe presumably because of the slow-growing nature. The plain radiography would show bony erosion and widening of the interpedicular space with or without vertebral abnormalities at the level of the lesion. Vertebral abnormalities include spina bifida, vertebral body fusion, asymmetry of the vertebral bodies, and diastematomyelia.[12] Computed tomography scanning may show variable tumor density or calcification. MRI usually shows mixed high and low signal intensity corresponding to cystic and solid composition of the tumor.[12] Calcification within the tumor, although not detected on imaging studies, can be present at the microscopic level in the lesion.[2]
The distinction between enterogenous cysts and mature teratomas of the spinal cord is a histopathological and clinical dilemma, in the presence of a coexisting occult neural tube dysraphism. Enterogenous cysts are subdivided into three groups: Group I is characterized histologically by the presence of only endodermal derived tissues; Group II by endodermal- and mesodermal-derived tissues; and Group III by endo-, meso-, and ectodermal-derived tissue components.[1] In our patient, the presence of tridermal-derived tissues makes the lesion distinct from Groups I and II. In addition, the features favoring teratoma over Group III ECs were the dorsal location of the tumor and the absence of the ventrally located dysraphic features associated with EC (including cysts of the mediastinum, duplication of the gastrointestinal tract, malformations of the vertebral bodies, or a defect in the vertebral column that communicates with the abdomen or thorax). Furthermore, in our patient, the bone defect (spina bifida) was present at the level of the tumor. In contrast, in patients with enterogenous cysts, the associated bone defect is usually several segments caudal to the lesion, as embryological vertebral bodies move caudally relative to the spinal cord.
Total resection is the treatment of choice for mature teratomas, whenever there is a good plane of cleavage between the tumor tissue and the cord parenchyma. However, marked tumor adhesions to the adjacent neural tissues, as in our case, preclude attempt at complete resection due to neural tissue injury and surgery should be aimed at maximum safe possible removal of the lesion. Such a procedure would hopefully provide patients with many symptom-free years due to the generally extremely slow growth of the residual teratomatous tissue. Outcome in terms of the clinical recovery varies. The role of adjuvant therapy of spinal cord teratoma is not well characterized because of the rarity of these lesions and the limited collective experience in their management.
Early clinical detection of cutaneous markers as well as widespread availability of the neuroimaging of the asymptomatic patients would help in the diagnosis of these rare congenital lesions before the neurological deficit sets in.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cystic mature teratoma of the filum terminale in an adult. Case report and review of the literature. Neurocirugia (Astur). 2004;15:290-3.
- [Google Scholar]
- Intramedullary teratoma of the spine: Report of two adult cases. Spinal Cord. 2002;40:40-3.
- [Google Scholar]
- Medullary compression by congenital tumors or cysts. Acta Neurol Psychiatr Belg. 1954;54:874-89.
- [Google Scholar]
- Cervical spinal cord intramedullary teratoma. Clin Neurol Neurosurg. 2006;108:514-7.
- [Google Scholar]
- Adult intramedullary mature teratoma of the spinal cord: Review of the literature illustrated with an unusual example. Acta Neurochir (Wien). 2006;148:663-9.
- [Google Scholar]
- Intramedullary mature teratoma of the cervical spinal cord at C1-2 associated with occult spinal dysraphism in an adult. Case report and review of the literature. J Neurosurg Spine. 2007;6:579-84.
- [Google Scholar]
- Adult cervical intramedullary teratoma: First reported immature case. J Neurosurg Spine. 2010;13:283-7.
- [Google Scholar]
- Cervical spinal teratoma associated with dermal sinus tract: MRI and surgical findings. Turk Neurosurg. 1992;2:194-8.
- [Google Scholar]
- Split cord malformation and cystic teratoma masquerading as lipomeningomyelocele. Childs Nerv Syst. 2003;19:46-9.
- [Google Scholar]
- Diastometomyelia associated with teratomas. Report of two cases. J Neurosurg. 1980;53:720-5.
- [Google Scholar]






