Translate this page into:
Emergent Neurosurgical Management of a Rapidly Deteriorating Patient with Acute Intracranial Hemorrhage and Alcohol-Related Thrombocytopenia
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Alcohol intoxication is a common risk factor of traumatic brain injury (TBI) and carries a significant health-care burden on underserved patients. Patients with chronic alcohol use may suffer a spectrum of bleeding diatheses from hepatic dysfunction not well studied in the context of TBI. A feared sequela of TBI is the development of coagulopathy resulting in worsened intracranial bleeding. We report the clinical course of an intoxicated patient found down with blunt head trauma and concurrent alcoholic cirrhosis who was awake and responsive in the field. Hospital course was characterized by a rapidly deteriorating neurological examination with progressive subdural and subarachnoid hemorrhage and precipitating neurosurgical decompression and critical care management. Our experience dictates the need for timely consideration of the possibility of rapid deterioration from coagulopathic intracranial bleeding in the initial assessment of intoxicated patients with head trauma of unknown severity, for which a high index of suspicion for extra-axial hemorrhage should be maintained, along with the immediate availability of operating room and the necessary medical personnel.
Keywords
Alcohol
coagulopathy
decompressive craniectomy
traumatic brain injury
underserved population
INTRODUCTION
Alcohol intoxication is reported in approximately one-half of all patients hospitalized for traumatic brain injury (TBI). Epidemiological evidence indicates that low socioeconomic status predisposes patients to alcohol dependence. The downstream effects of alcohol include platelet dysfunction, impaired clot formation, and thrombocytopenia. Several TBI studies report worse outcomes with acute intoxication,[12] while others propose a potential survival advantage due to the neuroprotective benefits.[3] However, in the clinical setting, these findings do not account for frequent association of acute intoxication with chronic use.
Starting in adolescence, alcohol use escalation is closely associated with environmental influences, such as the risk and protective factors that constitute the social environment. In the underserved population, such risk factors not only dispose individuals to head trauma but also become barriers to posttraumatic recovery and community reintegration. Patients with alcoholic cirrhosis may suffer altered hemostasis and/or experience a wide range of bleeding episodes as well as thrombotic events.[4] When patients present to the emergency department (ED) with head trauma and concurrent acute intoxication and liver cirrhosis, optimal management remains unclear.
Herein, we report the case of a 52-year-old man with a history of alcoholic liver disease (ALD) who was found awake and responsive after sustaining an unwitnessed fall. Numerous hematomas were present throughout the body suggestive of a chronic antihemostatic state. His initial ED Glasgow Coma Scale (GCS) score of 12 quickly declined to 4 due to space-occupying subdural and subarachnoid hemorrhages (SAHs).
CASE REPORT
The patient is a 52-year-old man found bleeding from a head laceration after an unwitnessed fall, who was alert and responsive. He reported drinking at the time of fall, and self-reported medical history was notable for liver cirrhosis. The initial assessment upon ED arrival was GCS 12 (eye = 3; verbal = 4; motor = 5). External injuries included a right periorbital contusion, 2-cm laceration on the right cheek, and bleeding from the scalp. Of note, numerous age-indeterminate superficial truncal and extremity hematomas approximately 1–2 cm in diameter were present, suggestive of a preexisting bleeding disorder/coagulopathy likely related to ALD. He remained responsive to commands. Complete blood count showed severe thrombocytopenia (platelets: 46,000/mL), coagulation studies were within normal limits, liver function tests showed aspartate aminotransferase 311 (laboratory reference range: 10–41 IU/L) and alanine aminotransferase 99 (laboratory reference range: 10–40 IU/L), and blood alcohol concentration was 0.4 g/dL (400 mg/dL).
Noncontrast head computed tomography (CT) demonstrated acute 1.2-cm left frontotemporal subdural hemorrhage along the falx cerebri and diffused SAH extending from the suprasellar cistern [Figure 1a and b]. The intracranial hemorrhage resulted in midline shift of approximately 5–7 mm. Re-examination showed a GCS of 4 (eye = 1; verbal = 1; motor = 2) with dilated and nonreactive pupils bilaterally, suggestive of progressive bleeding and bilateral herniation. Rapid sequence intubation was performed to maintain the airway, and emergent surgical decompression was pursued due to the concern of elevated intracranial pressure as evidenced by the rapid neurological decline.
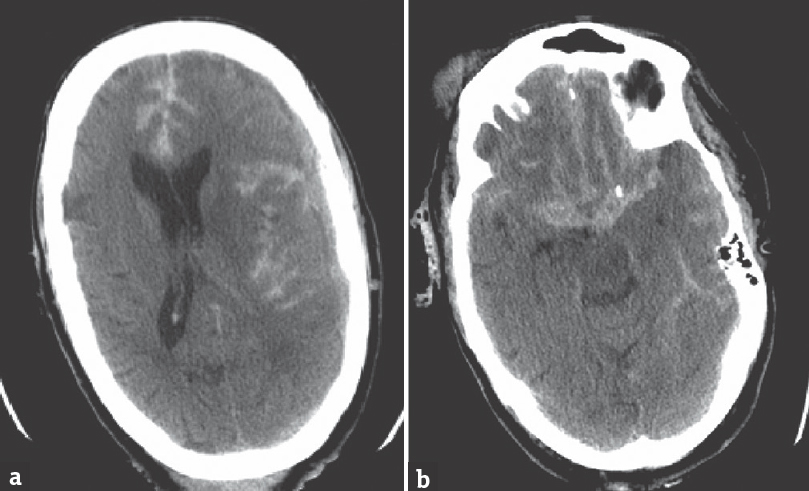
- Preoperative computed tomography scan demonstrates: (a) Frontotemporal subdural hemorrhage along the falx cerebri and midline shift compressing the left cerebral hemisphere; (b) diffuse subarachnoid hemorrhage extending from the suprasellar cistern
In the operating room, a left large frontoparietotemporal decompression was performed. Tamponade was partially successful due to difficulty attaining hemostasis, with an estimated blood loss of 1.5 L. The patient received 8 units of fresh frozen plasma, 2 units of cryoprecipitate, 2 packs of platelets, 5.5 L of crystalloids, and 4 units of packed red blood cells. At the end of the operation, the pupils remained 6 mm and unreactive bilaterally with GCS unchanged at 4. CT imaging demonstrated persistent cerebral edema and hemorrhage [Figure 2a and b]. Clinically significant neurological improvement was unable to be attained despite 4 days of intensive management per management guidelines for severe TBI, suggestive of diffuse inflammatory injury extending to the brain stem. The patient was compassionately extubated in accordance to the family wishes following discussion with the surrogate decision-maker.

- Postoperative computed tomography scan demonstrates: (a) Persistent intracranial hemorrhage with midline shift; (b) subarachnoid hemorrhage extending from the suprasellar cistern
DISCUSSION
Unwitnessed traumatic falls in the setting of acute intoxication and chronic alcoholism are common risk factors associated with TBI in the underserved population. While elevated blood alcohol level (BAL) is independently associated with decreased consciousness,[5] GCS in the intoxicated trauma patient should always be interpreted at face value during initial assessment as to judiciously intervene to minimize secondary injury following head trauma.[6] An estimated 10% of patients with SAH die before reaching the hospital, and this number may be greater for patients with limited access to neurosurgical services. The clinician should be critically mindful of the risk for rapid deterioration as intracranial bleeding quickly worsens due to hemostatic instability in cirrhotic patients. Urgent surgical management to reduce mortality and morbidity is recommended.[78] Undoubtedly, increased medical comorbidities that are present in the underserved population result in the urgent need for multidisciplinary medical management.
It is important to recognize that TBI patients frequently present with both elevated BAL and history of chronic alcoholism. Acute intoxication affects clot formation and fibrinolysis; therefore, screening methods using newer tests, for example, thromboelastography warrant further study as part of the diagnostic arsenal for patients at risk for coagulopathy. Liver dysfunction results in increased plasminogen activation and decreased plasmin inhibition,[9] which in our patient may have manifested as the numerous soft-tissue hematomas, and he presented with in addition to his worsening intracranial hemorrhage following head trauma.
Thrombocytopenia is a typical feature of chronic liver disease and may worsen intracranial bleeding. While early platelet transfusion should be considered, the threshold for platelet transfusion remains widely debated without an established body of evidence for feasible recommendations in the most recent TBI guidelines. A platelet threshold as low as 60 × 109/L in cirrhotic patients has been shown capable of preserving thrombin generation equivalent to that of healthy participants. Evidence for improved outcomes after coagulopathy reversal in patients with chronic hemostatic dysfunction, such as ALD, remains needed and awaits the well-designed multicenter clinical trial. Thrombocytopenia is an independent predictor of poor outcome in patients with preexisting low platelet count secondary to liver dysfunction.[10] While the benefits of early platelet transfusion should always be weighed against the risk of complications, judiciously considering transfusion should be a priority for patients presenting with TBI and alcohol abuse.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Alcohol abuse and traumatic brain injury: Quantitative magnetic resonance imaging and neuropsychological outcome. J Neurotrauma. 2004;21:137-47.
- [Google Scholar]
- The influence of ethanol intoxication on outcome of injured motorcyclists. J Trauma. 1984;24:695-700.
- [Google Scholar]
- Positive serum ethanol level and mortality in moderate to severe traumatic brain injury. Arch Surg. 2009;144:865-71.
- [Google Scholar]
- Hemostasis and thrombosis in patients with liver disease: The ups and downs. J Hepatol. 2010;53:362-71.
- [Google Scholar]
- Emergency department blood alcohol level associates with injury factors and six-month outcome after uncomplicated mild traumatic brain injury. J Clin Neurosci. 2017;45:293-8.
- [Google Scholar]
- Waiting for the patient to “sober up”: Effect of alcohol intoxication on Glasgow coma scale score of brain injured patients. J Trauma. 2006;61:1305-11.
- [Google Scholar]
- Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2016;1:25-36.
- [Google Scholar]
- The alpha2-plasmin inhibitor levels in liver diseases. Clin Chim Acta. 1978;84:99-105.
- [Google Scholar]
- Subsequent development of thrombocytopenia and coagulopathy in moderate and severe head injury: Support for serial laboratory examination. J Trauma. 2005;58:725-9.
- [Google Scholar]






