Translate this page into:
Depressive and Anxiety Symptoms in Relatives of Intensive Care Unit Patients and the Perceived Need for Support
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Admission of a patient in the Intensive Care Unit (ICU) and the recovery process may be stressful for family members.
Objectives:
This study aimed to explore the families’ psychological symptoms and their evolution over the 1st week of patients’ ICU stay. Additional objectives were the estimation of the families’ need for support and the estimation of satisfaction regarding the information provided by ICU physicians.
Methods:
A total of 108 individuals were participated in the study. Participants were interviewed with the Hamilton Anxiety Rating Scale and filled the Beck Depression Scale II on days 1 and 7 of patients’ ICU admission. They also filled a self-reported questionnaire which was created by the investigators, involving decision-making procedures; the satisfaction of the families of the patients’ care; and the support of the families by medical and nursing staff.
Results:
Anxiety levels were not significantly different among 2-time points, whereas rates of depressive symptoms raised significantly from 38% (day 1) to 58.3% (day 7). In cases of anxiety changes, age, education, closeness of relationship, and APACHE II score were the factors been associated. Changes in depressive symptoms were not associated with any of those factors. Over a week, there were significant differences in relatives’ views on participating in the decision-making procedure, and on expressing their opinion and concerns regarding the treatment process. Their attitudes about receiving support by the ICU personnel and even by mental health specialists, such as psychologists also changed.
Conclusions:
Over the 1st week of ICU admission, depressive symptoms in patients’ relatives were gradually evolving, while anxiety symptoms fluctuated and they were affected by the severity of the patients’ condition. Attitudes toward treatment procedures and the perceived need for support also changed. These findings should be taken into account by the ICU personnel.
Keywords
Anxiety
depression
Intensive Care Unit
relatives
support
INTRODUCTION
Admission of a patient in the Intensive Care Unit (ICU) and the recovery process may be stressful for family members. Patients’ relatives have to deal with the unfamiliarity of the ICU environment and the treatment procedures and with the uncertainty of the patients’ outcome. Thus, family's psychological stress is one of the most important issues concerning the ICU admission of a patient, due to lack of appreciation of their health condition, in terms of diagnosis, prognosis, and treatment.[1] Family members may experience high levels of fear, denial, anger, and guilt when facing the possibility of loss of their loved one in the ICU environment.[2] Several studies have addressed the short- and medium-term impact of ICU stay on the lives of the patients’ caregivers, and it has been consistently suggested that family members of ICU patients display depressive symptoms,[3] posttraumatic stress and anxiety,[4] fatigue and poor quality of sleep,[5] and that the symptoms tend to persist for several months after the patients’ hospitalization. A previous review reported that a high proportion of family members present with symptoms of anxiety and depression (70% and 35%, respectively).[6]
In Greece, there are only a few studies addressing the experiences of families of ICU patients. Paparrigopoulos et al.[7] found high levels of anxiety and depressive symptoms as well as posttraumatic stress (97% and 81%, respectively) in family members on the 1st week of admission. Those high rates of symptoms persisted 3 days before patients’ discharge to other wards (87% and 59%, respectively). More recently, a study on 223 Greek family members of ICU patients reported that a significant proportion of family members experienced high levels of cardiac anxiety on the 3rd day of admission.[8]
The aim of the present study is to explore the families’ psychological symptoms and their evolution over the 1st week of patients’ ICU stay. Additional study objectives are:
-
To explore the satisfaction of the ICU patients’ families during the 1st week of ICU stay
-
To explore the families’ need for support
-
To report on the level of satisfaction regarding the information provided by ICU physicians
-
To search for the impact of the participation to the decision-making process on the psychological condition of family members.
METHODS
Participants
This is a prospective study which was conducted over a 6-month period (from December 2014 to May 2015) in the ICU of the “G. Hatzikosta” General State Hospital of Ioannina, Northwest Greece. This is a six-bed ward which provides care for all critically ill patients. All family members of patients admitted to the ICU for at least 1 week were eligible for participation. Exclusion criteria were age <16 years, non-Greek speaking, and current mental health treatment. From a total of 132 participants who were initially approached for participation, 8 declined and 10 were excluded because they were illiterate or they received mental health treatment. Six more participants were excluded because although they were initially interviewed, the ICU stay of the patient was less than a week, due to patients’ death or transfer to another department. A total of 108 individuals participated in the study. Demographic information was obtained from participants and clinical information (APACHE score) was retrieved from patients’ charts.
The study's procedures were approved by the hospital's ethics committee. Written informed consent was obtained from all participants.
Research tools
The Hamilton Anxiety Rating Scale
For the estimation of the relatives’ anxiety symptoms, the Hamilton Anxiety Rating Scale (HAM-A) was used. This scale is largely used throughout the world as a valid and reliable tool for the estimation of anxiety. It has been translated and validated in Greek and has been used in research.[9] The interviews with the patients’ relatives were held on day 1 and day 7 of admission by the principal investigator (MB), after short-course training on the use of the scale.
The Beck Depression Scale II
The Beck Depression Scale II was used for the measurement of the depressive symptoms of the patients’ relatives. This is a self-reported questionnaire which includes 21 items measuring depressive symptomatology. This scale has been translated and validated in Greek and has shown good properties and interrater validity.[10]
Study participants were also given a self-reported questionnaire which was created by the investigators, involving decision-making procedures; the families satisfaction of the patient's care; the support of the families by medical and nursing staff; and the time schedule for the visits to the patient and the relatives’ waiting room. The five-grade Likert method was used for scoring to the items, with 0 meaning “totally disagree” and 4 corresponds to “totally agree.” Moreover, the participants were asked about their will to receive support from specialists (i.e., psychologists), during the patients’ ICU stay.
Statistical analysis
For the estimation of changes in the scores on Hamilton Anxiety Scale, the McNemar–Bowker test was used, whereas for the Beck's Depression Inventory, the McNemar test was used. For the inquiring of the factors related to score changes, we used the Pearson Chi-square test and also the multiple comparisons with the Bonferroni criterion. The level of significance was set at 0.05 for all comparisons. The SPSS v21.0 Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp) was used for all analyses.
RESULTS
Most participants were female (61.1%) and middle-aged, as 58.3% were in the range of 40–64 years. Two-thirds were living in urban areas. Most (71.3%) had no previous experience of a relative's ICU stay, whereas almost 20% had a history of mental disorder. Table 1 depicts the participants’ characteristics.
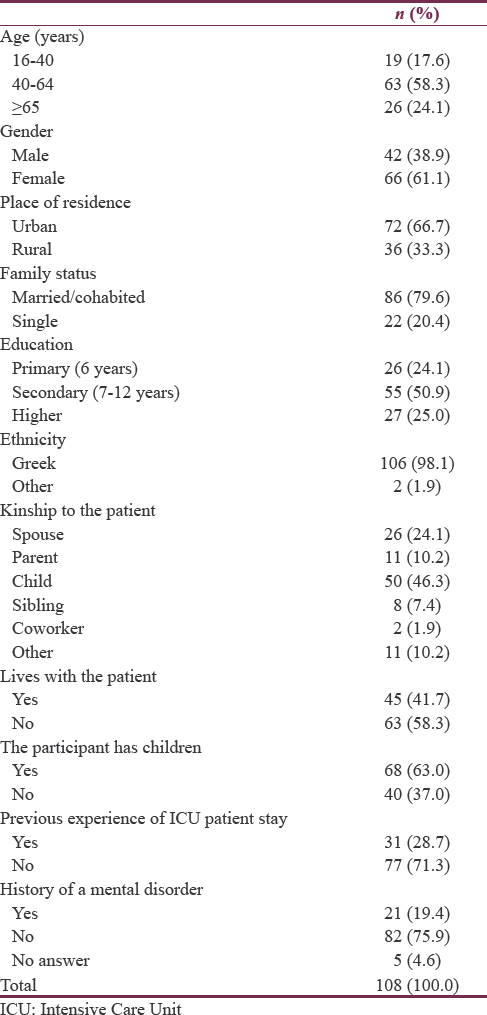
Table 2 shows the scores of the participants on the scales that measure the anxiety and depression levels (HAM-A and Beck II, respectively), at two different time points, that is, on patient's admission (day 1) and day 7 of ICU stay.

Table 3 shows the levels of anxiety as recorded with the HAM-A scale. Anxiety levels are not significantly different among 2-time points that are day 1 and day 7 of ICU admission.

On the other hand, the percentage of relatives who scored ≥17 on Beck-II raised from 38% (day 1) to 58.3% (day 7) [Table 4]. With the use of the McNemar test, it was found that changes of the scores on the Beck-II scale were statistically significant.

Regarding the factors that are associated with changes in the caregivers reported anxiety symptoms, we examined several demographic and clinical data (APACHE II score). Table 5 depicts all factors that have been correlated to changes in anxiety. Age, education, closeness of relationship, and APACHE II score were the statistical significant factors.

On the contrary, although changes in depressive symptoms between the 2-time points were statistically significant, there was no correlation of changes with the aforementioned factors (data not presented in a table).
Participants’ views on the patients’ ICU stay were also sought for. Those questions involved their perspective about treatment decision-making procedures, the perceived need for information and support, and the conditions of visiting the patient and the waiting room [Table 6].

DISCUSSION
The primary objective of the present study was to explore the development of acute psychological symptoms in family members of patients admitted to the ICU. Over a week period, total anxiety levels of family members were not significantly changed and a relatively small number of participants experienced severe anxiety at the 2-time points (13.9% and 12%, respectively). On the other hand, families’ depression levels were significantly higher at day 7 of evaluation, compared to day 1, and as high as 58.3% of them had scores ≥17 on the Beck-II sale, compared to 38% at the initial evaluation (P = 0.000).
Various studies worldwide have yielded different results regarding the psychological manifestations of ICU patients’ relatives. In a study in Brazil on 471 participants, the rates of anxiety and depression were 34% and 17%, respectively.[11] Even higher rates of anxiety (52%) were revealed in the study of Bandari et al.[12] on 720 relatives of ICU patients, whereas Choi et al.[13] reported a rate of depressive symptoms as high as 90%. Our results, especially the relatively low levels of anxiety that have been recorded, are somewhat different from those of previous research. This may be explained by differences at the time point of assessment, the sample, and the research tools. For instance in a comparative study in two tertiary hospitals in India and the USA Kulkarni et al.[14] reported on the differences of the levels of anxiety and depression among relatives of ICU patients in these countries. Interviews were held within 48–72 h of admission. It was found that relatives in India displayed higher levels of anxiety than their American counterparts, although posttraumatic stress was almost the same in the two groups. Comorbid depressive and anxiety symptoms were present in 30% and 5% in relatives in India and the USA, respectively. The differences were attributed to differences in education and socioeconomic factors within different health systems. It was also found that the severity of the patients’ condition and being a spouse were predictors of the development of depressive symptoms. The results of the present study are somewhat different, as depressive symptoms were gradually evolved over a week, independently of the aforementioned factors.
Regarding anxiety levels our study shows no statistical difference in overall scores between days 1 and 7 of admission. However, in cases that there were changes in anxiety levels, factors such as age, education, closeness of relationship, and APACHE II score were found to correlate. Improvement was recorded in ages 16–40 years and worsening in ages >65 years. Higher education was also associated with improvement in anxiety rates at day 7. More specifically, anxiety in lower education participants was rated as “moderate to severe” in 40%, comparing with 26.7% in the highly educated participants at day 1, whereas at day 7, those rates were 61.5% and 15.4%, respectively. With regard to the kinship to the patient, among the participants with anxiety, spouses had severe anxiety at a rate of 40% at day 1 which raised significantly (53.8%) at day 7, whereas the percentage of children with severe anxiety was 20% and 23.1%, respectively. McAdam et al.[4] studied a sample of 74 family members of ICU patients who had poor prognosis and high possibility of death at day 4 of admission. More than half family members displayed symptoms of posttraumatic stress, whereas 80% had marginal anxiety symptoms and 70% marginal depressive symptoms. Other symptoms, such as fear, sorrow, and fatigue were present in 80% of the relatives. Younger age and female gender were associated with symptoms’ development. The results of the present study, as well as those of another Greek study,[7] are in line with the notion that women are prone to develop anxiety symptoms during a relative's ICU stay.[15]
It is interesting to note that while anxiety symptoms are subjected to changes associated with several demographic and clinical factors, depressive symptoms in our sample increase steadily over a week and are not related to any of these factors. This means that during the 1st week of ICU admission, depressive symptoms are gradually evolving, while anxiety symptoms may fluctuate and they are affected by the severity of the patients’ condition, as measured with the APACHE II score.
With regard to the attitudes of family members toward the ICU stay of their relatives and the treatment procedure, the present study showed that families thought of having control over the care at a rate of 31.5%. A proportion of family members (30.5%) felt that they were members of the treatment decision-making process and even more (38.9%) preferred to be a part of this process. Importantly, 39.8% of family members felt that they had support from the ICU personnel and they had the time to express their concerns and to get answers to their queries regarding the treatment of their loved ones. Another study finding was that some family members (31.5%) wish to receive information about the ICU through brochure, as they thought it would be helpful and relieving to know about the ICU operation and about their rights and obligations. Even larger percentage of relatives (42.5%) opted for flexibility in the visiting hours and for the setup of a waiting room for them (48.2%). Much less relatives (almost 30%) had a positive attitude toward receiving support from associations and mental health specialists. It is interesting to note that during ICU stay of a patient the attitudes of their relatives gradually change. As Table 6 shows, there are significant differences in relatives’ views on participating in the decision-making procedure and on expressing their opinion and concerns regarding the treatment process. Importantly, over a week, they changed their attitudes about receiving support by the ICU personnel and even by mental health specialists, such as psychologists. This could be explained by the higher levels of depressive symptoms they developed which made them less reluctant to seeking help and support.
Several studies have addressed the issue of supporting families whose relative is admitted in the ICU. There is some evidence that several interventions, such as supportive groups[16] and the provision of material with information regarding the ICU treatment[17] may reduce relatives’ symptoms of depression and anxiety. In another study, the most effective way for relatives to deal with anxiety and depressive symptoms during the first days of ICU admission was acceptance and support seeking through counseling.[18] A previous Greek qualitative study highlighted the need of ICU patients’ families to receive information regarding the treatment process.[19] More recently, Chatzaki et al.[20] conducted a multicenter study on 230 patients’ relatives. They found that the provision of information and reassurance was most important for relatives. These results are in line with the findings of our study.
Regarding decision-making process, Heyland et al.[21] found that a quarter of relatives prefer treating physicians to make decisions and a further 15% did not wish to be part of this process. Almost 40% preferred share decision-making and 22% did so after physicians’ recommendations. The results of the present study are in line with previous research. It is worthy to note that according to Pochard et al.[22] more than two-thirds of relatives suffer anxiety or depressive symptoms, and this undermines their ability to act as the patient's surrogates. Conceivably, clinicians should bear in mind that relatives’ ability to participate in end-of-life decisions may be limited by their psychological manifestations.
Notably, it has been suggested that satisfaction of patients’ relatives regarding ICU stay is high.[21] Auerbach et al.[23] showed that the good interpersonal relationship with the medical and nursing staff may impact on the relatives’ satisfaction and their need for information. Thus, satisfaction with the ICU treatment may be mediated by good communication between the personnel and the relatives[24] and by support provision.
Strengths and limitations
This is a prospective study with a sufficient sample of participants addressing the issue of acute psychological symptoms displayed by the relatives of patients admitted to the ICU. In general, the results of this study are in line with the few previous national and international reports, yet some differences were yielded, which probably can be attributed to differences in methodology and study sample. However, the present study has some limitations. It involved a single ICU ward, and this limits the generalizability of findings. This is in accordance with the notion that there are some notable differences among the results of several studies worldwide. Other wards with critically ill patients, such as the coronary heart unit were not included in the study. The study design involved the short-term (over a week) assessment of relatives’ psychological symptoms, and there was no medium- or long-term follow-up. There is some evidence that symptoms of posttraumatic stress, anxiety, and depression may persist over a 3-month period and are associated with adverse outcome.[2526] Clearly, more research in different wards of several hospitals, with larger samples of relatives and longer-term follow-up, are needed to better understand the needs of ICU patients’ families and for the subsequent arrangement of appropriate short- and medium-term interventions to address these needs.
CONCLUSIONS
The findings of this study may be relevant for clinical practice. Given the high rates of depressive symptoms of patients’ relatives and their positive attitudes toward receiving support from specialists, efforts should be made to address these needs. For instance, ICU personnel should establish a close cooperation with the consultation-liaison psychiatric service of the hospital, so as to refer relatives promptly. Moreover, the ICU personnel should be trained to recognize as early as possible those relatives in need for support. For the relatives of patients whose clinical condition worsens during ICU stay, ICU personnel should be aware that they may be prone to develop anxiety symptoms and arrange appropriate consultation. Moreover, some training on basic supportive skills may be warranted for the ICU personnel. This could be relevant for relatives reluctant to receiving interventions from specialists, yet in need for psychological help.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Half the families of Intensive Care Unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28:3044-9.
- [Google Scholar]
- Perceived and unmet needs of critical care family members. Crit Care Nurs Q. 1998;21:58-67.
- [Google Scholar]
- Limited family members/staff communication in Intensive Care Units in the czech and slovak republics considerably increases anxiety in patients’ relatives – The DEPRESS study. BMC Psychiatry. 2014;14:21.
- [Google Scholar]
- Symptom experiences of family members of Intensive Care Unit patients at high risk for dying. Crit Care Med. 2010;38:1078-85.
- [Google Scholar]
- Sleep, anxiety and fatigue in family members of patients admitted to the Intensive Care Unit: A questionnaire study. Crit Care. 2013;17:R91.
- [Google Scholar]
- Having a loved one in the ICU: The forgotten family. Curr Opin Crit Care. 2012;18:540-7.
- [Google Scholar]
- Short-term psychological impact on family members of Intensive Care Unit patients. J Psychosom Res. 2006;61:719-22.
- [Google Scholar]
- Symptoms of cardiac anxiety in family members of Intensive Care Unit patients. Am J Crit Care. 2016;25:448-56.
- [Google Scholar]
- Assessment of anxiety symptoms among intensive care nursing personnel in Greece. Nursing. 2009;48:447-57.
- [Google Scholar]
- Adaptation of Beck-II depression scale in Greek residents. Hell J Psychol. 2013;10:120-46.
- [Google Scholar]
- Anxiety, depression, and satisfaction in close relatives of patients in an open visiting policy Intensive Care Unit in Brazil. J Crit Care. 2015;30:440.e1-6.
- [Google Scholar]
- Psychometric properties of the Persian version of the critical care family needs inventory. J Nurs Res. 2014;22:259-67.
- [Google Scholar]
- Health risk behaviors in family caregivers during patients’ stay in Intensive Care Units: A pilot analysis. Am J Crit Care. 2013;22:41-5.
- [Google Scholar]
- Comparison of anxiety, depression, and posttraumatic stress symptoms in elatives of ICU patients in an American and Indian public hospital. Indian J Crit Care Med. 2011;15:147-56.
- [Google Scholar]
- Stress and coping of Hong Kong Chinese family members during a critical illness. J Clin Nurs. 2007;16:372-81.
- [Google Scholar]
- Effects of support groups on anxiety of family members during critical illness. Heart Lung. 1990;19:62-71.
- [Google Scholar]
- Improving cognitive development of low-birth-weight premature infants with the COPE program: A pilot study of the benefit of early NICU intervention with mothers. Res Nurs Health. 2001;24:373-89.
- [Google Scholar]
- The acute psychobiological impact of the intensive care experience on relatives. Psychol Health Med. 2016;21:20-6.
- [Google Scholar]
- The experiences of families of critically ill patients in Greece: A social constructionist grounded theory study. Intensive Crit Care Nurs. 2009;25:10-20.
- [Google Scholar]
- Defining the needs of ICU patient families in a suburban/rural Greek population: A prospective cohort study. J Clin Nurs. 2012;21:1831-9.
- [Google Scholar]
- Measuring family satisfaction with care in the Intensive Care Unit: The development of a questionnaire and preliminary results. J Crit Care. 2001;16:142-9.
- [Google Scholar]
- Symptoms of anxiety and depression in family members of Intensive Care Unit patients: Ethical hypothesis regarding decision-making capacity. Crit Care Med. 2001;29:1893-7.
- [Google Scholar]
- Optimism, satisfaction with needs met, interpersonal perceptions of the healthcare team, and emotional distress in patients’ family members during critical care hospitalization. Am J Crit Care. 2005;14:202-10.
- [Google Scholar]
- How to improve communication quality with patients and relatives in the ICU. Minerva Anestesiol. 2016;82:797-803.
- [Google Scholar]
- Posttraumatic stress and complicated grief in family members of patients in the Intensive Care Unit. J Gen Intern Med. 2008;23:1871-6.
- [Google Scholar]
- Psychological symptoms of family members of high-risk Intensive Care Unit patients. Am J Crit Care. 2012;21:386-93.
- [Google Scholar]






