Translate this page into:
Perception and Attitude toward Mental Illness in Antenatal Mothers in Rural Population of Southern India: A Cross-Sectional Study
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Mental health disorders globally are on a rise due to various reasons. Gender differences have been one of the reasons. Pregnancy is a stressful event in mothers and it can either exacerbate preexisting mental illness or can give rise to other mental health disorders. Studies have shown that women residing in rural areas are at higher risk of developing mental health problems. Mental health problems have detrimental effects in post-partum period. Most of the complications can be prevented if psychiatric symptoms are detected in early part of pregnancy and if women are aware of these symptoms.
Aim:
To find the awareness, attitude and perception towards mental illness in antenatal mothers residing in rural area of India.
Setting and Design:
It's a descriptive cross sectional study conducted at primary health care centers.
Methods and Materials:
Total of 300 antenatal mothers attending primary health care centers were recruited into the study after a written informed consent was obtained.
Statistical Analysis:
Basic socio demographic data were collected and a semi structured questionnaire was designed. The participants were interviewed according to the questionnaire. Data collected was analyzed using SPSS software.
Results and Conclusion:
The mean age of the study participants was 24+5. Of the 300 study participants more than 90% were unaware that mental illness can occur during pregnancy and only around 07% could agree say that it can occur in pregnancy. There is poor awareness of mental health problems amongst pregnant women residing in rural part of southern India. The reasons for the same are lack of awareness, low levels of education, lower socio economic status, cultural beliefs and practices, lack of mental health services and stigma associated with mental illness. There is no routine screening for mental health problems during antenatal visits. If done otherwise could bring down adverse maternal outcome.
Keywords
Antenatal mothers
attitude and perception
mental illness
INTRODUCTION
Mental health disorders are on a rise globally. It is estimated that the mental health disorders contribute to 14% of global burden of the disease,[1] and according to recent update of World Health Organization (WHO) world mental health survey, the prevalence of mental health disorders ranges from 18.1% to 36.1%.[2] In India, the prevalence of mental disorders is 10.6%.[3] At least 20% of population has one or the other mental health problems.[4] It is also observed that mental health problems have a gender bias slightly occurring more common in females than males.[5] There have been observations that mental health problems occur more in rural areas than urban areas. An Indian epidemiological study reports prevalence rates of mental and behavioral problems up to 37.1%.[6] In another study done in rural south India, the prevalence rate of mental disorders was found to be 24.4%.[7] People who come from poor socioeconomic strata with lower education with poor awareness and stigma related to mental illness are at higher risk of suffering from mental illness.[8] Women especially in their reproductive age are more prone to develop mental illness and stressful events such as pregnancy being one of the reasons.[910] With declining maternal mortality, more emphasis is put on maternal morbidity. Psychological disturbances occurring during pregnancy are linked with inadequate antenatal care, low-birth weight, and preterm delivery, while in the postpartum, it has been associated with poor emotional involvement, neglect, and hostility toward the newborn. Much of the data in this area are from the developed world, particularly, the United States, Canada, Europe, and Australia, the last decade has seen some interesting publications from developing countries as well where gender disadvantage, poverty, and limited access to resources further complicate the issue. Mental illness occurring in pregnancy affects maternal outcome and overall quality of life.[11]
During antenatal period, more emphasis is given to physical problems of the mothers than the psychological and emotional well-being of the mothers. Physical problems such as pregnancy-induced hypertension and others are treated as high-risk pregnancy, whereas mental illness is not addressed adequately unless it is severe. One of the studies done in Southern India showed that knowledge about mental illness overall in general public was poor and associated with negative attitude.[12] This could be because the mothers during their antenatal period are unaware about common mental illness that can occur during antenatal period and fail to recognize it in early stages leading to poor maternal outcome. Hence, this study aims to find out the awareness and perception of mental health problems in pregnant women residing in rural areas of India.
METHODOLOGY
The present study is a descriptive, cross-sectional in nature. A total of 300 participants were recruited by convenient sampling method. The structured questionnaire was prepared by community medicine and psychiatry experts. The questionnaire contained information on various study variables, items on knowledge, attitude, and practice toward common mental illnesses prevailing in that area. The questionnaire included “Yes” or “No” type and multiple options type. This study was carried out in a community health center and primary health center in all antenatal mothers attending these centers. Knowledge and attitude about mental illness were assessed using the questionnaire by semi-structured interview. Initial pilot study was conducted to ascertain if the questionnaire was easily understood and was indeed appropriate. Based on the finding from this pilot study, the questionnaire was adapted and no major changes were required. Data collection took place from April 2017 to August 2017. Participant's verbal and written informed consent was obtained before their participation in the study. No incentives were offered to the study participants. All the participants received an explanation that the study results would be of benefit to the general practice of mental health, especially in pregnant women. Confidentiality of results was assured. Data entry and statistical analysis was performed using the Epi - Info 7 WHO software.[13]
RESULTS
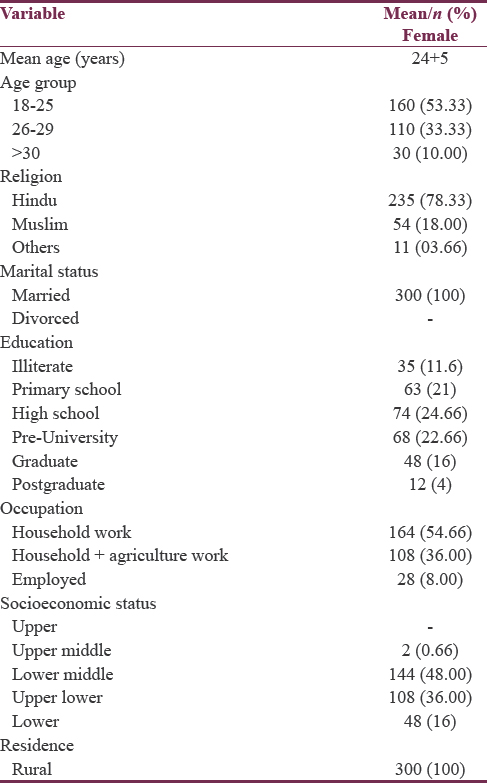
Of the 300 pregnant women who took part in the study, 53.33% were between 18 and 25 age group, 33.33.% were between 26 and 30 age group, and 10% were above 30 years. The mean age of the study participants was 24 + 5. Nearly 78.33% of the study participants belonged to Hindu religion followed by 18% belonged to Muslim religion and rest 3.66% were from other religion. According to Modified BG Prasad's classification,[14] 48% belonged to lower middle class followed by upper lower accounting to 36% and 16% by lower socioeconomic status. By status of education, majority (24.66%) had studied up to high school. Almost 22.66% went to preuniversity. Nearly 21% accounted for primary school, 16% were graduates, and 4% were postgraduates. About 54.66% were homemakers by their occupation, 36% were involved in both agricultural and household work, and 28% were employed in either public or private sectors. The sociodemographic details have been depicted in Tables 1 and 2.

Of the 300 study participants, >90% were unaware that mental illness can occur during pregnancy and only around 7% could agree say that it can occur in pregnancy. 90% of the study participants(antenatal mothers) felt that mental illness in pregnancy means - being possessed by god, or goddess or some devil l. Very few were aware about common mental illness such as depression and anxiety disorders. Almost 44.66% came to know about their mental illness from their relatives and friends, 14.6% knew from mass media, and 12.66% knew from newspaper ads. About 5.3% reported awareness because they had a history of being suffering from mental illness in the past. Only 3.6% reported to have come to know from their treating physician. Nearly 97.33% reported that their treating physician do not ask for symptoms of mental illness during their antenatal visits. Only 2.66% reported that their treating physician asks about mental illness symptoms. More than 50% believed that they would seek treatment if they develop mental illness in pregnancy, whereas 46.3% refuse to seek treatment. If detected 46% felt that they would consult their treating physician, 42% felt they would visit faith healers, and 12.66% felt they would seek a consultation with mental health professionals. Almost 91% reported that they do have mental health services available at their place and 9% reported that they had mental health services available either in full time or part time.
DISCUSSION
Pregnancy is one of the happy moments for most women yet it is a stressful life event. Pregnancy is associated with various psychological, social, emotional, and physical changes. Of late, there has been increase in reporting of mental health problems from both developing and underdeveloped countries.[15] There have been studies which have shown that mental health problems in pregnancy are associated with various complications such as preterm, low birth weight babies, increased risk of developing postpartum depression, poor mother–child bonding, and overall poor maternal outcome leading to increased maternal morbidity.[1617] Studies on antenatal psychological well-being are on a rise in recent years.[11] It has been observed that prevalence of psychological problems in pregnancy are occurring more commonly in developing countries than developed countries.[18] Since our study is done in rural area of southern India, our findings are in concurrence with the findings of previous studies. This could be because of lack of awareness (85.6%) about mental health problems in pregnancy, lack of mental health services (91%), and various beliefs and cultural practices in that area. Almost 42% reported that they would visit a faith healer for their problems; 88.66% did not believe in receiving medications if mental illness occurred in pregnancy. Nearly 96% reported stigma-related problems. In another study done in rural part of southern India by Chandran et al. reported high incidence and prevalence of depression and other psychological problems during antenatal period, even though these pregnant women suffered these illness, they never sought for any treatment, who eventually had poor outcome during postpartum period. The reasons why they never sought help were beliefs by mothers’ family members and even the health workers that the existing symptoms during antenatal period were part of normal pregnancy.[19] Our study also found that majority of mothers believed that these symptoms either do not occur in pregnancy and if occurred these symptoms were due to acts of witchcraft and did not need any professional intervention. Additional finding which needs a special mention is >90% of treating physicians do not ask about mental illness symptoms routinely. A high-risk pregnancy traditionally was defined as one complicated by a serious medical condition that may jeopardize its outcome.[20] Hence, we suggest that common mental health problems occurring during antenatal period warrant routine screening and to be treated as high-risk pregnancy and one should not focus only on medical problems as high risk. A study by Rahman et al. reported that psychological problems were associated with poor nutritional outcomes in the infants and this study argued for promotion of maternal mental health to be included in maternal and child health programs.[21] Our study shows that 85% of mothers were unaware and 97.3% of the times the treating physician do not ask about mental health symptoms. This could be because current maternal and child health program emphasize more on medical problems and neglects maternal mental health and another reason could be a busy outpatient department and lack of time or even work overload. Hence, we suggest that, by screening for common mental health problems during antenatal visits, one can detect psychological problems early and can be referred to mental health specialist in the early stage and hence prevent adverse maternal outcome. By referring to mental health specialist, level of awareness can be improved and one can take away the wrong beliefs which people harbor.
CONCLUSIONS
There is poor awareness of mental health problems among pregnant women residing in rural part of southern India. The reasons for the same are lack of awareness, low levels of education, lower socioeconomic status, cultural beliefs and practices, lack of mental health services, and stigma associated with mental illness. There is no routine screening for mental health problems during antenatal visits and are not treated as high-risk pregnancy. If done otherwise could bring down adverse maternal outcome and maternal morbidity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- World Health Organization. Mental Health. World Health Organization. Available from: http://www.who.int/mental_health/en
- The global burden of mental disorders: An update from the WHO world mental health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18:23-33.
- [Google Scholar]
- National mental health survey of India 2015-2016. Indian J Psychiatry. 2017;59:21-6.
- [Google Scholar]
- Indian psychiatric epidemiological studies: Learning from the past. Indian J Psychiatry. 2010;52:S95-103.
- [Google Scholar]
- Women and mental health in India: An overview. Indian J Psychiatry. 2015;57:S205-11.
- [Google Scholar]
- Prevalence of mental and behavioural disorders in India: A meta-analysis. Indian J Psychiatry. 1998;40:149-57.
- [Google Scholar]
- Suttur study: An epidemiological study of psychiatric disorders in South Indian rural population. Indian J Psychiatry. 2014;56:238-45.
- [Google Scholar]
- National Rural Health Policy Brief. Rural Women Health; January; 2013.
- Epidemiological study of prevalence of mental disorders in India. Indian J Community Med. 2001;26:102.
- [Google Scholar]
- Suicide prevention is possible: A perception after suicide attempt. Indian J Psychiatry. 2012;54:172-6.
- [Google Scholar]
- Maternal mental health in pregnancy and child behavior. Indian J Psychiatry. 2011;53:351-61.
- [Google Scholar]
- Mental health issues and challenges in India: A review. Int J Sci Res Publ. 2013;3:1-2.
- [Google Scholar]
- Epi Ino. WHO Software. Available from: https://www.cdc.gov/epiinfo/index.html
- Antenatal depression in Anuradhapura, Sri Lanka and the factor structure of the Sinhalese version of Edinburgh post partum depression scale among pregnant women. PLoS One. 2013;8:e69708.
- [Google Scholar]
- Depression during pregnancy: Prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind Psychiatry J. 2013;22:37-40.
- [Google Scholar]
- Mental health aspects of pregnancy, childbirth and the postpartum period. In: Chandra PS, Herman H, Fisher J, Kastrup M, Niaz U, Rondon MB, eds. Contemporary Topics in Womens Mental Health-Global Perspectives. United Kingdom: John Wiley and Sons Ltd; 2009. p. :197-226.
- [Google Scholar]
- Gender, poverty, and postnatal depression: A study of mothers in Goa, India. Am J Psychiatry. 2002;159:43-7.
- [Google Scholar]
- Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. Incidence and risk factors. Br J Psychiatry. 2002;181:499-504.
- [Google Scholar]
- Psychological aspects of high risk pregnancy. Glob Lib Womens Med 2009:1756-2228. Doi: 10.3843/glowm.10155
- [Google Scholar]
- The neglected ‘m’ in MCH programmes – Why mental health of mothers is important for child nutrition. Trop Med Int Health. 2008;13:579-83.
- [Google Scholar]






