Translate this page into:
Profile of Patients from a Neurology Registry in Resource-Poor Rural Northwest India
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The neurology register is based in a tertiary care center in a rural north-west India. The center caters to a predominantly rural population. The present study is based on the data retrieved from this registry over a period of 1 year.
Materials and Methods:
Details of the patients reporting to the Department of Neurology are entered in a registry. For the purpose of this study, 1-year data (from August 1, 2013, to July 31, 2014) of patients (with complete information and final diagnosis) were analyzed.
Results:
Out of a total of 2431 patients, 1296 (53.3%) were males and 1135 (46.7%) were females. The six major neurological disorders identified were epilepsy and seizures, headache, spondolysis with neurological manifestations, cerebrovascular disease, Parkinsonism, and neuropathies.
Conclusion:
Six neurological disorders account for more than two-thirds of the patients with neurological disorders, whereas epilepsy, seizures, and headache together constituted more than one-third.
Keywords
Neurology
profile
registry
resource-poor
INTRODUCTION
Neurology as a branch of science and medicine, in particular, has reached an exciting period in its growth curve. Newer initiatives such as the Human Brain Project and US Brain Research through Advancing Innovative Neurotechnologies across the world will catapult neurology as the most happening branch of medicine.[1] However, the benefits of these initiatives may not be felt across geographies and populations as most of the neurology services worldwide have a definite urban bias. With a large concentration of neurologists based in the bigger cities, the rural areas tend to suffer. This urban-rural divide in neurological health services is felt more in developing countries like India where 97% of neurologists practice in cities and less than 3% neurologists are available to treat the population in the rural area, where majority of the Indians live.[2]
MATERIALS AND METHODS
The neurology clinic in our center was established in August 2012 and runs outpatient department (OPD) on 3 weekdays. A hospital-based register was established to maintain a record of patients presenting to the neurology OPD which is directly manned by the neurologists. Patients of all age groups presenting to the Department of Neurology are included in the register. Variables such as age, sex, occupation, residence, and income relating to the patient are entered in the register after eliciting information on the same from the patient in a structured format. In case of disoriented and minor patients, history on the variables is collected from guardian/parent of the patient through an in-person interview at the time of registration. Each interview lasts about 15–20 min. A detailed survey is conducted on each patient to establish the diagnosis. A provisional diagnosis is made based on the history and examination after which a unique number is allotted to each patient and his/her further recordings are made on the same number. The same number is used for the conduct of investigations and follow-up after which a final diagnosis is made. The final diagnosis is also entered in the register.
Methods
The study was approved by the institutional ethics committee. For the purpose of this study, data for 1 year from August 1, 2013, to July 31, 2014, were screened. However, only patient data with complete information were included for analysis. Therefore, of a total of 3067 patients entered in the registry, 2431 (79.2%) patients with complete data were included. In the patients having two or more diagnoses, the predominant diagnosis was taken and the patient was only entered once.
The data were entered in the Excel spreadsheet based on the diagnosis. In certain disorders, subdiagnosis was also made and data were entered accordingly [Tables 1 and 2]. The data were analyzed using the Excel software of Windows 8 Professional version.

RESULTS
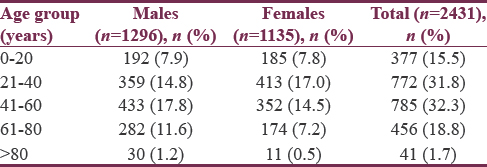
A total of 2431 patients were analyzed, of which 1296 (53.3%) were males and 1135 (46.7%) were females. Maximum number of males (17.8%) were in the age group of 41–60 years, whereas females were maximum in the age group of 21–40 years (17%) [Table 1]. The mean age of all patients in years was 42.61 (standard deviation [SD] 19.83), with mean age of males as 44.51 (SD 20.59) and females as 40.45 (SD 18.3).
Epilepsy and seizures (E&S) was the most common diagnosis in males (22.1% of males), whereas headache was the most common diagnosis in females (23% of females). Together, these two disorders accounted for 37.4% of the total patient load. These were followed by spondylosis with neurological manifestations (8.2%), cerebrovascular diseases (7.9%), Parkinson's disease (4.5%), and neuropathies (4.4%). The age-wise distribution of these six diagnoses is shown in Figure 1.

- Age-wise distribution of six common diagnoses
In the subgroup analysis of 541 patients of E&S, 34% had generalized-onset epilepsy whereas 49% had focal E&S. Seventeen percent were either with dissociative reaction or their epilepsy types could not be differentiated. On further analysis, it was found that 4.4% of total epilepsy patients or 13% of generalized-onset epilepsy patients were juvenile myoclonic epilepsy (JME). Active neurocysticercosis (NCC) was the most common cause of focal seizures (18.7%) and constituted 9.2% of total E&S [Tables 2–4].


Headache was the second most common diagnosis with 368 (15.1%) of patients suffering from this disorder, of which 106 (4.4%) were males and 262 (10.8%) were females. In this group, migraine was the most common diagnosis with 61% of total headaches. It was found that 15.9% of all females had this type of headache whereas only 3.4% of males presented with migraine. Tension-type headache was the next most common headache which was 16.5% of the total headaches, with males constituting 6.5% and females 10% [Tables 2–4].
Spondylosis with neurological manifestations was the third most common group with 8.2% of patients falling in this group. Eleven percent of total males and 5% of total females were suffering from this problem. Single prolapsed inter vertebral disc (PIVD) causing a single radiculopathy whether it was cervical or lumbosacral was the most common diagnosis which was 48.2% of total patients in this group. Of total males, 4.62%, and of total females, 3.2% had this diagnosis. Cervical radiculomyelopathy was the next most common entity with 3.1% of total patients, and 37% of patients in this group had this disease. Lumbar canal stenosis was seen in 14.5% in this group, which was 1.2% of total patients [Tables 2–4].
Cerebrovascular diseases were the fourth most common group of disorders, with 7.9% of patients – 5.3% males and 2.6% females. Of the total males and females, 10% and 5.6%, respectively, had this disorder. Infarction was the most common entity in this group comprising 75% of all cerebrovascular disorders, in which 51% were males and 24% were females. Intraparenchymal bleed was present in 19.8% constituting 13.5% males and 6.3% females. Cerebral venous thrombosis was seen as 4.7% of total cerebrovascular disease [Tables 2–4].
Parkinsonism and Parkinson's disease was the fifth most common entity with 5.5% of patients falling in this group. Of these, 2.9% were males and 4.1% were females. 78% of this group had idiopathic Parkinson's disease – 35% males and 43% females. In this group, 22% had Parkinson's plus syndromes. Dyskinesias were segregated separately, and they constituted 1.2% of total patients. If we club movement disorders together, then they constituted 6.7% of total patients [Tables 2–4].
Peripheral neuropathies as a group were the sixth most common entity with 5.4% of patients. Distal symmetrical neuropathy was the most common subgroup with around 40% of patients (28.5% males, 11.5% females) followed by mononeuropathy in 37% of patients
DISCUSSION
As a group, E&S was the most common diagnosis with nearly one-fifth of the patients. As the center mainly deals with referrals from secondary care centers, this group of patients ranged from newly diagnosed to difficult-to-treat patients. In the so-called refractory/difficult to treat epilepsy category, JME stands out as it is frequently misdiagnosed and labeled as either partial seizure, complex partial seizure, or even dissociative reactions.[345] NCC was the most common entity in focal group. A study from the National Institute of Mental Health and Neuro Sciences,[6] Bangalore, reported a diagnosis of NCC in 2% of all epilepsy patients whereas, in another study from Delhi, NCC was the cause in 2.5% of all intracranial space-occupying lesions.[7] A study from South India reported NCC as the cause in one-third of all cases of active epilepsy.[8]
As per the GBD 2015, Neurological Disorders Collaborator Group – “migraine was the cause of around 13.1% of disability-adjusted life years (DALYs) lost to the world population.”[9] In our analysis, migraine was the most common headache with female-to-male ratio of nearly 5:1. It was the most common disease in females with around 15% of total females suffering from a migraine. As per the clinical course of the disease, it was most prevalent in the age group of 20–40 years, which comprised 44% of all our patients with migraine. This subset of female patients was the reason why females were maximum in the age group of 20–40 years. Most of the patients were already diagnosed as migraine but were on either inadequate treatment or at times the prophylaxis was not emphasized upon. The nonpharmacologic aspects of disease management were also not given adequate attention. The findings from our study were similar to other studies in this regard.[91011] Surprisingly, tension-type headache was also more common in females and was found to be nearly as twice more than reported in previous data.[91213]
Spondylosis with neurological manifestations as a group was specifically taken together as a subset of patients with vertebral column diseases secondary to degeneration, disc disease, without any trauma or infection, but with definite neurological manifestations. In a study by Singhal et al., it was found that 3.8% of new indoor patients were due to this group of disorder.[14]
Cerebrovascular diseases are the leading cause of mortality and morbidity in the spectrum of neurological disease.[15] In our study, it was the fourth most common disease entity as against the most common entity in one similar study from Ghana, Africa.[16] Around 8% of the patients presented with this disorder, of which three-fourths were arterial infarction, one-fifth hemorrhages, and rest were venous thrombosis and infarcts. As is the global trend, half of our patients with infarcts were in the age range of 61–80 years and around 37% were in the age range of 41–60 years. Most of the patients managed by us during the study period were followed up patients, and none of the arterial infarcts were thrombolysed. Thrombolysis as an intervention was later taken up as part of our Telestroke project.[17]
Parkinsonism was not clubbed with other dyskinesias as they may not be having a pure degenerative etiology. GBD 2015, Neurological Disorders Collaborator Group found that Parkinson caused 0.8% loss of DALYs and 1.2% of deaths.[8] 1.2% of patients were reported as cases of dementia and included Alzheimer's disease and frontotemporal and vascular dementia. The findings correlated with the prevalence estimates for dementia from an earlier field-based study from our area.[18]
Distal symmetrical neuropathy secondary to diabetes mellitus was the most common entity strengthening the fact that diabetes and its complications have really spread itself in rural India.[1920] Mononeuropathy secondary to trauma, iatrogenic, or otherwise was next common entity. People in the rural areas have a preference for intramuscular injections, and sural/common peroneal nerve injury secondary to this is a very commonly encountered.[21]
Cranial neuropathies were clubbed in different diagnostic groups – cranial neuropathies and trigeminal neuralgias, in which cranial neuropathies constituted 2.9% of total patients (males 1.4% and females 1.5%). This was done due to difference in the etiologies and management of cranial neuropathies. If these are added to the neuropathies, then this would have been group of 8.3% patients and it would be the third largest group of neurological disorders preceded only by headache and E&S.
CONCLUSION
The spectrum of neurological disorders in rural India does not differ markedly from urban India and the western world. The big three – headache, E&S, and Cerebrovascular accidents (CVA) – still constitute to the main bulk of patients. Spondylosis with neurological manifestations is another major problem, and as a neurologist we must be aware of the finer nuances of this disorder.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Distribution of neurologists and neurosurgeons in India and its relevance to the adoption of telemedicine. Neurol India. 2015;63:142-54.
- [Google Scholar]
- The relationship between neurocysticercosis and epilepsy: An endless debate. Arq Neuropsiquiatr. 2014;72:383-90.
- [Google Scholar]
- Incidence of solitary cysticercus granulomas. In: Rajshekhar V, Chandy MJ, eds. Solitary Cysticercus Granuloma: The Disappearing Lesion. Chennai: Orient Longman; 2000. p. :12-28.
- [Google Scholar]
- Focal epilepsy in India with special reference to lesions showing ring or disc-like enhancement on contrast computed tomography. J Neurol Neurosurg Psychiatry. 1987;50:1298-301.
- [Google Scholar]
- Active epilepsy as an index of burden of neurocysticercosis in Vellore district, India. Neurology. 2006;67:2135-9.
- [Google Scholar]
- Global, regional, and national burden of neurological disorders during 1990-2015: A systematic analysis for the global burden of disease study 2015. Lancet Neurol. 2017;16:877-97.
- [Google Scholar]
- Underdiagnosis and undertreatment of migraine in Italy: A survey of patients attending for the first time 10 headache centres. Cephalalgia. 2009;29:1285-93.
- [Google Scholar]
- Barriers to headache care in India and efforts to improve the situation. Lancet Neurol. 2004;3:564-7.
- [Google Scholar]
- Overview, diagnosis, and classification of headache. In: Silberstein SD, Lipton RB, Dalessio DJ, eds. Wolff's Headache and Other Head Pain (7th ed). New York: Oxford University Press; 2001. p. :6-26.
- [Google Scholar]
- Surgery versus conservative management of sciatica due to a lumbar herniated disc: A systematic review. Eur Spine J. 2011;20:513-22.
- [Google Scholar]
- Profile of neurological disorders in an adult neurology clinic in Kumasi, Ghana. eNeurologicalSci. 2016;3:69-74.
- [Google Scholar]
- Telestroke in resource-poor developing country model. Neurol India. 2016;64:934-40.
- [Google Scholar]
- Is dementia differentially distributed. A study on the prevalence of dementia in migrant, urban, rural, and tribal elderly population of Himalayan region in Northern India? N Am J Med Sci. 2014;6:172-7.
- [Google Scholar]
- High prevalence of diabetes in an urban population in South India. BMJ. 1988;297:587-90.
- [Google Scholar]
- The need for obtaining accurate nationwide estimates of diabetes prevalence in India – Rationale for a national study on diabetes. Indian J Med Res. 2011;133:369-80.
- [Google Scholar]
- Neurological Practice – An Indian Perspective (1st ed). New Delhi: Elsevier India; 2005. p. :606.






