Translate this page into:
Impact on Cognitive Improvement Following Burr Hole Evacuation of Chronic Subdural Hematoma: A Prospective Observational Study
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
Patients of Chronic subdural haematoma can present with only subtle cognitive impairment without any motor deficit. It is hence imperative for the treating clinician to be aware of this entity. The aim of the study was to identify any statistically significant improvement of cognitive functions following burr hole evacuation of Chronic SDH especially in the elderly patients.
Methods and Material:
A Prospective observational study of 30 patients of CSDH, from Jan 2015 to Dec 2016 was done at a tertiary level Armed Forces Hospital. The study had 23 male, 07 female, with age ranging from 7-85 years. The cognitive function of each patient was assessed at admission and 24 hours after surgery by MMSE. Radiological confirmation was done by CT head. Standard two burr holes were made and hematoma evacuated. The clinical, cognitive assessment and radiological data were collected and analysed.
Results:
There was no statistical significance preoperatively between age and pre operative cognitive impairment, headache, hemiparesis, dysarthria (P>0.05). We however found a statistically significant improvement postoperatively in cognitive impairment, headache (P= 0.00), motor deficit (P=0.01) and dysarthria (P=0.046).
Conclusion:
The clinical features of dementia and other neurodegenerative disorders simulate CSDH in the geriatric population. These patients should have early neuroimaging and prompt surgical intervention to alleviate cognitive deficits.
Keywords
Chronic subdural hematoma
cognitive impairment
dementia
INTRODUCTION
Chronic subdural hematoma (CSDH) is an old liquefied clot of blood underneath the dura and arachnoid membrane. CSDH mostly occurs in patients aged above 60 years having brain atrophy.[1] Other predisposing factors include cerebral degeneration, trauma, coagulopathy, and intracranial hypotension.[2] Clinically, patients may present with features of that of stroke or those of raised intracranial pressure. In the elderly age group, patients of CSDH have impaired cognitive functions in the form of transient memory loss or language impairment.[3] These subtle symptoms can be confused with early dementia and other neurodegenerative diseases.[4] The aim of this observational study was to identify any statistically significant improvement of cognitive functions following burr hole evacuation of CSDH.
MATERIALS AND METHODS
A prospective observational study of 30 patients of CSDH was carried out from January 2015 to December 2016 at a tertiary-level Armed Forces Hospital. The study had 23 male and seven female patients, with age ranging from 7 to 85 years. The cognitive function of each patient was assessed at admission and 24 h after surgery using Mini-Mental State Examination (MMSE) scale. The clinical, cognitive assessment and radiological data were collected and analyzed. The lesions were diagnosed by computed tomography (CT) head. Two standard burr holes on the frontal and parietal regions were made along with evacuation of CSDH till the returning fluid was clear. As a protocol, noncontrast CT (NCCT) head was done within 24 h of surgery. The data were analyzed for age and sex; thickness and side of CSDH; and pre- and postoperative clinical improvement and improvement in cognitive deficit. We measured the cognitive status using MMSE on admission and at 24 h after surgical evacuation of CSDH. Cognitive impairment was confirmed when the recorded MMSE score was <23 out of 30. MMSE score of 23 or less is generally accepted as indicating cognitive impairment.[5]
Inclusion criteria
All cases of CSDH irrespective of age and sex were included in the study.
Exclusion criteria
All cases of:
-
Acute and subacute subdural hemorrhage
-
Cases of CSDH who were managed conservatively
-
Known cases of dementia.
Statistical analysis
Data of all the patients were collected and analyzed using paired t-test and Wilcoxon signed-rank test. In all circumstances, a P < 0.05 was considered statistically significant.
RESULTS
There were 23 men (76.6%) and seven women (23.3%), with age ranging from 7 to 85 years. Fourteen patients had left-sided CSDH, 13 had right-sided CSDH, and the remaining three patients had bilateral CSDH as shown in Table 1. Mean size of hematoma was 17.9 mm.

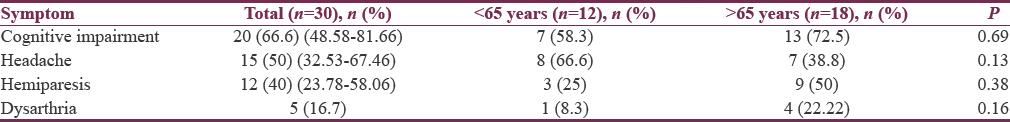
The preoperative mean MMSE was 22.97, whereas the postoperative mean MMSE was 26.60. The chief clinical symptom of cognitive impairment was present in 20 patients (66.6%). There were headache in 15 patients (50%), motor deficits (monoparesis or hemiparesis) in 12 patients (40%), and dysarthria in five patients (16.7%) [Table 2]. The incidence of preoperative cognitive impairment was 58.3% (7 out of 12) in patients <65 years of age, whereas it was 72.5% in (13 out of 18) in patients >65 years of age. There was no statistical significance between the clinical symptoms in relation with age (P > 0.05) [Table 2]. However, in our study, we found a statistically significant improvement postoperatively in cognitive impairment, headache (P = 0.00), motor deficit (P = 0.01), and dysarthria (P = 0.046) [Table 3].

DISCUSSION
The overall incidence of CSDH is high between the fifth and sixth decades as per the available literature.[123] The symptoms and signs of CSDH vary from subtle cognitive deficits to frank hemiplegia. The symptoms include change in the level of consciousness, dysarthria, psychomotor deterioration, headache, and vomiting, resulting from an increased intracranial pressure.[67]
The symptoms of increased intracranial pressure are common among young patients, but focal neurologic deficit and cognitive impairment are common among elderly.[3] The study conducted by Ye et al.showed that headache was common in patients below 65 years of age, while cognitive impairment was a predominant symptom in patients above 65 years of age. Our study has also revealed similar outcome parameters [Table 2].
CSDH can have a bizarre clinical presentation. It can vary from incidental fever and urinary incontinence to the central nervous system (CNS) manifestations such as headache, altered consciousness, aphasia, motor weakness, seizure, and vomiting.[8] A detailed history along with high index of clinical suspicion is required in elderly patients who present with subtle cognitive impairment. Such patients should be assessed by MMSE and NCCT head along with neurosurgical consultation. However, 40% of patients with CSDH have a clinical presentation akin to other neurodegenerative diseases such as stroke, dementia, and tumors.[6] Although literature suggests that neuropsychiatric symptoms are common in elderly patients with CSDH, the number of objective studies to prove that are limited.[37]
Dementia is a progressive, irreversible syndromic disorder which has multifactorial etiology. It has ill effects on health and has a high economic burden on society and nation as a whole.[79] Various studies have, however, enumerated multiple causes of reversible impairment of neurocognitive functions and dementia.[91011]
Dementia which is reversible is usually associated with cognitive or behavioral symptoms which can be resolved once the primary etiology is treated.[12]
The literature review has shown that frequency of reversible dementia is up to 23%.[1314] Some of the most common causes of reversible dementia are alcohol, iatrogenic dementia, depression, leading to cognitive impairment, neurosurgical causes, such as normal pressure hydrocephalus, CSDH, and tumors. Metabolic disorders such as hypothyroidism, hypoparathyroidism, Vitamin B12 deficiency, and CNS infections such as neurosyphilis and HIV have also been implicated as possible causes of reversible dementia.[41315]
It is, hence, imperative to identify early and treat these reversible causes of dementia. The cognitive impairment associated with CSDH is mostly reversible by surgical intervention.
A study conducted by Ye et al.[3] documented that there was a statistical significance between age and preoperative cognitive impairment and headache (P < 0.05). In our study, we however did not find any significant correlation between age and preoperative cognitive impairment and headache [Table 2].
In our study, 17 (85%) of the 20 patients with initial MMSE <23 showed cognitive improvement (postoperative MMSE >23). These results are quite comparable to the study by Ye et al. in 2008,[3] where approximately 50% of patients with CSDH were suspected of having dementia on admission and the surgery showed improved cognitive outcome in 70% of these patients. In our study, the postoperative improvement in cognitive impairment was statistically significant with P = 0.00. We also found a statistically significant improvement in motor deficit, P = 0.00 and dysarthria, P = 0.046 [Table 3].
Hence, CSDH should be an important differential diagnosis of reversible dementia. Early evacuation though primarily is done to reduce headache, improve motor function, and stabilize, the patient has also shown improved cognitive outcome.
CONCLUSION
Dementia and various other neurodegenerative diseases mimic CSDH in its clinical manifestations. A high degree of clinical suspicion for CSDH should be kept against the background of cognitive impairment. Such patients should have early imaging and prompt surgical intervention to alleviate cognitive impairment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We sincerely thank Dr. Seema Patrikar for assisting in the statistical analysis.
REFERENCES
- Histopathological study of the outer membrane of the dura mater in chronic sub dural hematoma: Its clinical and radiological correlation. Asian J Neurosurg. 2016;11:34-8.
- [Google Scholar]
- Cognitive impairment in the elderly with chronic subdural hematoma. J Korean Neurotraumatol Soc. 2008;4:66-9.
- [Google Scholar]
- Reversible dementia in patients with chronic subdural hematomas. J Neurosurg. 2002;96:680-3.
- [Google Scholar]
- The minimental state examination – An up-to-date review. Harefuah. 2006;145:687-90. 701
- [Google Scholar]
- Chronic subdural hematoma in adult and elderly patients. Neurosurg Clin N Am. 2000;11:447-54.
- [Google Scholar]
- The US economic and social costs of Alzheimer's disease revisited. Am J Public Health. 1994;84:1261-4.
- [Google Scholar]
- Chronic subdural hematoma: Epidemiological and prognostic analysis of 176 cases. Rev Col Bras Cir. 2015;42:283-7.
- [Google Scholar]
- Reversible dementia in elderly: Really uncommon? J Geriartric Ment Health. 2015;2:30-7.
- [Google Scholar]
- Prevalence of potentially reversible conditions in dementia and mild cognitive impairment in a geriatric clinic. Geriatr Gerontol Int. 2012;12:59-64.
- [Google Scholar]
- Prevalence of potentially reversible cognitive function disorders in patients of a memory dysfunction clinic. Psychiatr Pol. 2006;40:845-54.
- [Google Scholar]
- The decreasing prevalence of reversible dementias: An updated meta-analysis. Arch Intern Med. 2003;163:2219-29.
- [Google Scholar]
- The relationship of preoperative magnetic resonance imaging findings and closed system drainage in the recurrence of chronic subdural hematoma. J Neurosurg. 1997;87:870-5.
- [Google Scholar]






