Translate this page into:
Real-World Effectiveness of Intravenous Stroke Thrombolysis is more than the Expectation of Practicing Neurologists
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The objective of the study was to compare the actual results of intravenous thrombolytic therapy (IVTT) in acute ischemic stroke with results anticipated by neurologists in practice.
Methods:
Neurologists practicing in Thrissur metropolitan region, covering a population of 1.8 million, were telephonically surveyed about the number of yearly IVTT and their expert opinion/comment about effects of thrombolysis. This was compared with the results of IVTT from a single institution in the same region from 2012 to 2016.
Results:
Eight neurologists in the region give approximately 140–150 IVTT per year. Nearly 20%–40% (median 32%) patients have good outcome, 5%–10% (median 9%) have intracerebral hematoma (ICH), and 25%–35% (median 30%) have death/bad outcome. Two neurologists from a tertiary care hospital in the region treated 122 cases of ischemic strokes with IVTT from 2012 to 2016. Age ranged from 8 to 88 years and 88 were males. Average delay in reaching hospital was 138.1 min and the door-to-needle time was 56.3 min. There were 26 cases of posterior-circulation strokes and 14 cases of cardioembolic strokes. At presentation, average National Institute of Health Stroke Scale (NIHSS) was 14.7; Modified Rankin Scale (mRS) 0.4; and CT Alberta Stroke Program Early Computerized Tomography Scores was 9.5. Good and sustained benefit (GSB) (>4 reduction in NIHSS at 24 h and 7 days) was there in 49% and no improvement (NI)/worsening in 36%. mRS 0–2 at discharge/30 days was documented in 57.3%. Symptomatic ICH was 10% (12/122) and mortality rate was 11.5% (14/122). GSB in posterior circulation strokes was 69.2% and NI/worsening in only 7.7%. mRS was 0–2 in 77% of posterior circulation strokes.
Conclusion:
Contrary to the popular belief of the practicing neurologists, IVTT has a high percentage of good outcome with a reasonable bleeding risk and low rates of absolute futility.
Keywords
Ischemic stroke
stroke outcome
stroke treatment survey
thrombolysis
INTRODUCTION
The global burden of acute ischemic stroke (AIS) is on a rise,[1] and the treatment with intravenous thrombolytic therapy (IVTT) using alteplase within the window period is the most effective and established immediate management strategy of this pandemic.[2] However, despite active efforts from many corners, the thrombolysis rates are still low, especially in the developing world.[23] Although the barriers for thrombolysis are many,[45] low acceptance among physicians may be an important factor.[6] Over-projected bleeding risk and subjective feel of futility[7] may be significant in this regard.[6] The clinical decision-making about IVTT varies among physicians.[78] The negative role of previous bad patient outcome in subsequent decision-making is well established.[9] In practice, most physicians remember a few patients who had no improvement (NI) or worsened following an IVTT. How far this subjective feeling of practicing physicians is substantial? We aimed to survey neurologists in Thrissur city routinely doing IVTT about their subjective feeling of effectiveness of IVTT and compare it with objective results of IVTT in a prospective hospital-based registry.
METHODS
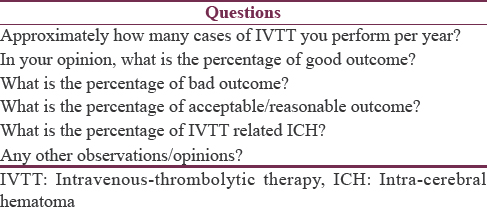
The study was done in Thrissur metropolitan region in the central part of Kerala, South India. The region caters to a population of 1.8 million.[10] Only neurologists in tertiary care hospitals practice IVTT in the region. There were two parts for the study. The first part was to survey the neurologists giving IVTT in the region about their personal opinion on the results of the intervention. The second part was to compare this with the actual clinical outcome of IVTT in a prospective thrombolysis registry maintained in a tertiary care hospital from the same region. Table 1 shows the questions asked in the telephonic survey. Neurologists from institutions with registry data were asked to give their expert opinion but not their data.
The second part of the study was done in a 350-bedded tertiary care hospital in Thrissur metropolitan region. A prospective stroke thrombolysis registry is maintained in the institution with all the clinical details of the cases undergoing IVTT. There are two neurologists in the hospital routinely doing thrombolytic therapy for ischemic stroke patients. Standard protocols are followed for the selection, drug administration, and post-thrombolysis care.[11]
Consecutive cases of ischemic stroke from April 2012 to March 2016 in the thrombolysis registry were selected for the analysis. The registry data were verified by reviewing the charts of all cases. Notice was made on demographic data, time delay in reaching the emergency room (ER), door-to-needle time, and the type of ischemic stroke. Risk factors, comorbidities, current drug usage, blood glucose, and blood pressure (BP) at presentation and complications during hospital stay were also noted. National Institute of Health Stroke Scale (NIHSS) scores[12] recorded at presentation to ER, at 24 h, at 7 days, and at 30 days or at the time of discharge were noted. Modified Rankin Scale (mRS) scores[13] before the stroke, at 24 h, at 7 days, and at 30 days or at the time of discharges were similarly noted. Furthermore, Alberta Stroke Program Early Computerized Tomography Scores (ASPECTS)[14] at presentation to ER and at 24 h were noted. The benefit of IVTT was categorized into four types [Table 2].

RESULTS
Questionnaire survey
Thrissur metropolitan region caters to a population of 1.8 million. Only neurologists in tertiary care hospitals do stroke thrombolysis in the region. There are three teaching and seven nonteaching tertiary care hospitals with at least one practicing neurologist in the region. Two teaching centers and one nonteaching center are not practicing stroke thrombolysis. The survey was conducted among neurologists of the hospitals except the one from which registry data were analyzed. Apart from this hospital, another tertiary care hospital also maintains a systematic thrombolysis registry. Neurologists from that center were asked to give their personal opinions and not to look into their registry data.
Total eight neurologists working in six hospitals were surveyed. They all put together give around 140–150 IVTT per year. Patient selection was strictly based on standard guidelines and none reported any protocol violation.[11] The feel about the outcome of IVTT was almost similar across all neurologists. The apparent percentage of IVTT-related intracerebral hematoma (ICH), the neurologists felt, ranged from 5% to 10% (median 9%). They thought that 20%–40% (median 32%) of IVTT patients have good outcome, whereas death/bad outcome occurs in 25%–35% (median 30%). They also felt that the rest of the patients has a slow recovery, which appears to be natural and not related to the IVTT.
Thrombolysis registry review
From April 2012 to March 2016, out of 3096 ischemic stroke admissions, 122 patients (3.9%) received IVTT with alteplase. Age of patients who received IVTT ranged from 8 to 88 years (median 62 years); 88 were males and 34 were females. Out of 122 patients, 66 were hypertensive, 60 were diabetic, 16 had dyslipidemia; coronary artery disease was there in 22, chronic kidney disease in 8, and chronic obstructive airway disease in 14. Prior ischemic stroke or transient ischemic attack was there in 16 patients, antiplatelet use in 30, and oral anticoagulant use in 6 patients. Average blood glucose at presentation was 166.5 mg%; BP ranged from 90/60 mmHg to 220/140 mmHg.
Average delay in reaching hospital was 138.1 min (range: 10–720, median: 120); there were three outliers with wake-up strokes. Average door-to-needle time was 56.3 min (range 10–135, median 52.5). Average delay of starting of IVTT from onset of stroke was 194.4 min (range 90–780 and median 180).
Fourteen patients had cardioembolic strokes (eight atrial fibrillation – four each valvular and nonvalvular, four severe left ventricular dysfunction, and two congenital heart disease). There were 38 cases of right anterior circulation strokes, 58 cases of left anterior circulation strokes, and 26 cases of posterior circulation strokes.
Average NIHSS score at presentation was 14.7 (range 4–40, median 11.5); mRS before stroke was 0.4 (range 0–3, median 0). Computerized tomography (CT) scan ASPECTS score was on an average 9.5 (range 7–10) at presentation; old infarcts or subcortical white matter changes were seen in 62 patients.
Two pediatric patients received alteplase 20 mg, whereas all the rest received alteplase 50 mg. Twenty-eight patients required BP reduction with labetalol before IVTT. During the hospital stay, 16 patients had seizures, 16 had pneumonia, 12 had urinary tract infection, 10 had new-onset renal dysfunction, 12 had hyponatremia, 8 had acute myocardial infarction (AMI), and 2 patients had upper gastrointestinal bleeding. There were 14 in hospital deaths, 10 due to symptomatic ICH, 2 due to worsening hepatic dysfunction, and another 2 due to AMI.
Average NIHSS at 24 h was 10.2 (range 0–40 and median 8). CT scan at 24 h showed symptomatic ICH in 12 patients and nonsymptomatic ICH in 6; ASPECTS score was on an average 7 (range 2–10, median 7.5). Average 7th day NIHSS was 8.5 (range 0–40, median 6); however, data were not available in eight patients (four died before 7th day, two shifted due to AMI for percutaneous coronary intervention, and two discharged before 7th day due to excellent outcome). Seventh day mRS was 2.8 (range 0–6, median 3). mRS at discharge was 2.7 (range 0–6, median 2) and at 30 days was 2.3 (range 0–6 and median 2; data were not available in 22). One-year mRS was 1.86 (range 0–6; data not available in 78).
Good and sustained benefit (GSB) was there in 60 (49%) patients and NI/Worsening in 44 (36%) patients. Sixteen (13%) had slow improvement, whereas two had good benefit followed by worsening. mRS 0–2 at discharge/30 days was documented in 70 (57.3%) patients. Symptomatic ICH was 10% (12/122) and mortality rate was 11.5% (14/122). Out of 26 patients with posterior circulation strokes, 18 (69.2%) showed GSB and 20 (77%) had an mRS of 0–2 at discharge/30 days. There were 14 cardioembolic strokes; eight (57%) had GSB, whereas 6 (42.8%) had mRS 0–2 at discharge/30 days.
DISCUSSION
Despite the striking benefit of IVTT in AIS, its use is limited to a minority of stroke patients in India and rest of the world, other than big academic stroke centers.[23] Although various reasons have been put forward for this discrepancy, authors have come across another curious reason during the discussions with fellow neurologists from institutions with less number of IVTT per year. Many subjectively felt that the benefit, if at all, with IVTT is modest and bleeding risk is high.[567] They do remember cases in which they landed in trouble. We thought that this feeling of the treating neurologists might be another reason for the low IVTT rates. How far this subjective feeling of futility about IVTT is substantial?
We wanted to compare the subjective feeling of benefit and complications of IVTT with objective measure of the same. For this comparison, we selected a group of practicing neurologists in a metropolitan region and assessed their subjective feeling about IVTT by a structured questionnaire. These data were compared with the objective results of the IVTT in a thrombolysis registry of a hospital from the same metropolitan region. We postulated that the subjective feeling of futility of IVTT might be a reason for lower thrombolysis rates.
Overall, the survey among practicing neurologists has shown that the bleeding risk of IVTT, which they think, is around 10%. They feel that roughly only a third really benefitted from IVTT, whereas another third have no benefit or worsening due to IVTT and the remaining third has a slow natural recovery not related to the drug effect. However, our results in the thrombolysis registry were not supporting this. Although the ICH rate was around 10%, GSB was seen in 49% at 7 days of IVTT and a good functional outcome (mRS 0–2) of 57.3% at the time of discharge from hospital or at 30 days of stroke. The rate of bad outcome (NI or worsening) of 36% was similar to what was anticipated by the neurologists in the survey. These higher than anticipated GSB at 7 days and functional outcome at the time of discharge/at 30days were present in posterior circulation and cardio-embolic strokes as well.
Another important observation is that the rates of slow “natural recovery,” which the practicing neurologists “predicted,” are not correct. Only 13% had this course, and in fact, even these people had significant recovery at 7 days. This is the reason why there is 57.3% good functional outcome at 30 days or at discharge. Hence, this group also has to be taken as those who are having good benefit to IVTT (and not as “unrelated natural recovery”).
Thus, the registry shows that around 60% of people receiving IVTT have a good outcome at the time of discharge or at 30 days. This is certainly in contrast to the one-third good outcome anticipated by practicing neurologists. The anticipated low outcome may be influencing the thrombolysis decisions and the rates of low thrombolysis.[78] Why does this discrepancy occur. We feel that it is related to the memory about really bad cases, which the physician had treated in the past. He may not be remembering the chunk of good cases he had treated. A similar scenario in aortic aneurysm surgery is detailed elsewhere.[9] Our study is really an eye-opener, which advises the physician that subjective feeling may not be correct and the actual data are more important. Analysis of our registry correlate well with large series.[15] Compared to the neurologists in the survey who used to stick to the time window, we even had gone out of the window period, treating wake-up strokes.[16] Still our patients had good outcome compared to what is anticipated by those in the survey, once again underscoring the benefit of IVTT.
The rate of ICH related to IVTT in our series is higher than the recent registries.[31517] The reason may be that we included at least a few cases outside the window period. However, in the survey also, neurologists felt roughly 10% ICH rates. Whether IVTT-related ICH rates are really high in our population? Although there is a suggestion in a recent study,[18] this requires further investigation.
CONCLUSION
The IVTT in AIS has a very good functional outcome, contrary to the belief of neurologists practicing the therapy. We believe that the therapeutic nihilism related to the apprehension of practicing neurologists about the benefit of IVTT is a strong reason for low thrombolysis rates, at least in our part of the world. Keeping registries in every institutions and periodically reviewing the data could mitigate this.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge the help of Dr. Abdul Majeed, Neurologist and Ms. Pearly chief staff nurse of Mother Hospital, Thrissur, for allowing us to use stroke thrombolysis registry.
REFERENCES
- Update on the global burden of ischemic and hemorrhagic stroke in 1990-2013: The GBD 2013 study. Neuroepidemiology. 2015;45:161-76.
- [Google Scholar]
- The Chinese stroke association scientific statement: Intravenous thrombolysis in acute ischaemic stroke. Stroke Vasc Neurol. 2017;2:147-59.
- [Google Scholar]
- A review of barriers to thrombolytic therapy: Implications for nursing care in the emergency department. J Neurosci Nurs. 2010;42:88-94.
- [Google Scholar]
- Why are eligible thrombolysis candidates left untreated? Am J Prev Med. 2006;31:S210-6.
- [Google Scholar]
- Medico-legal aspects of using tissue plasminogen activator in acute ischemic stroke. Curr Treat Options Cardiovasc Med. 2011;13:233-9.
- [Google Scholar]
- Survey of emergency physicians about recombinant tissue plasminogen activator for acute ischemic stroke. Ann Emerg Med. 2005;46:56-60.
- [Google Scholar]
- Factors that Influence Variation in Clinical Decision-Making about Thrombolysis in the Treatment of Acute Ischaemic Stroke: Results of a Discrete Choice Experiment. Southampton (UK): NIHR Journals Library; 2017.
- [Google Scholar]
- Risk as feelings in the effect of patient outcomes on physicians’ future treatment decisions: A randomized trial and manipulation validation. Soc Sci Med. 2012;75:367-76.
- [Google Scholar]
- Thrissur Urban Region. Available from: http://www.census2011.co.in/census/metropolitan/419-thrissur.html
- Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
- [Google Scholar]
- National Institute of Health, National Institute of Neurological Disorders and Stroke. Stroke Scale. Available from: http://www.ninds.nih.gov/doctors/NIH_Stroke_Scale.pdf
- [Google Scholar]
- Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J. 1957;2:200-15.
- [Google Scholar]
- Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS study group. Alberta stroke programme early CT score. Lancet. 2000;355:1670-4.
- [Google Scholar]
- Role of tissue plasminogen activator in acute ischemic stroke. Ann Pharmacother. 2011;45:364-71.
- [Google Scholar]
- Thrombolytic therapy in wake-up stroke patients. Clin Neuropharmacol. 2017;40:140-6.
- [Google Scholar]
- Risk of intracerebral haemorrhage with alteplase after acute ischaemic stroke: A secondary analysis of an individual patient data meta-analysis. Lancet Neurol. 2016;15:925-33.
- [Google Scholar]
- Race/Ethnic differences in the risk of hemorrhagic complications among patients with ischemic stroke receiving thrombolytic therapy. Stroke. 2014;45:2263-9.
- [Google Scholar]






