Translate this page into:
Repeated Peritoneal Catheter Blockage Caused by Neurocysticercosis Following Ventriculoperitoneal Shunt Placement for Hydrocephalus
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cerebral cysticercosis is common, but the possibility for repeated occurrence of peritoneal catheter blockage caused by neurocysticercosis (NCC) after two revisions following ventriculoperitoneal shunt placement for hydrocephalus is unusual. Herein, we describe one rare case in which peritoneal catheter revision was performed two times unsuccessfully. Endoscopic cysternostomy rather than peritoneal catheter adjustment was performed successfully, and histopathological examination of excised cystic samples confirmed NCC in our hospital. The present case highlights the need for awareness of NCC as a possible etiology of hydrocephalus, especially in developing countries. Uncommon findings in both lateral ventricles following low-field magnetic resonance imaging scans as well as the rarity of this infection involved in unusual location play important roles in misdiagnosis and incorrect treatment for hydrocephalus; thus, endoscopic cysternostomy, rather than multiple shunt adjustment of the peritoneal end, is recommended in the selected patient. To the best of our knowledge, this is the first report describing the misdiagnosis and inappropriate treatment of hydrocephalus caused by cerebral cysticercosis in China.
Keywords
Blockage
diagnosis
neurocysticercosis
treatment
ventriculoperitoneal shunt
INTRODUCTION
Cysticercosis is a serious food-borne parasitic disease caused by the cysticercus larvae of Taenia solium. Humans acquire cysticercosis by eating food or drinking water contaminated with the eggs of this tapeworm.[1] Cysticercosis is distributed worldwide, but most cases occur in Latin America, West Africa, China, and Southeast Asia.[2] In China, cysticercosis is an important food-borne parasitic zoonosis and poses a serious threat to human health.[3] Cysticercosis in the central nervous system is common; in most cases, the cysticerci located in the parenchyma of the brain and cause seizures and headaches.[4] When neurocysticercosis (NCC) cysts are present within the ventricles of the brain, it can block the outflow of cerebrospinal fluid, lead to hydrocephalus, and cause the symptoms of increased intracranial pressure.[5]
Ventriculoperitoneal (VP) shunt is the common surgery to treat hydrocephalus, which is used to shunt cerebrospinal fluid from the lateral ventricles of the brain into the peritoneum.[6] However, the repeated occurrence of peritoneal catheter blockage after two revisions for the VP shunt placement is uncommon. Here, we report one rare case in which peritoneal catheter revision was performed twice in 2 years following the initial placement of a VP shunt. All operations for peritoneal catheter adjustment were unsuccessful. However, subsequent endoscopic ventriculocysternostomy, rather than peritoneal surgery, was performed successfully, and histopathological examination of the excised cystic samples confirmed NCC. To the best of our knowledge, this is the first report describing the misdiagnosis and inappropriate treatment of hydrocephalus caused by cerebral cysticercosis in China.
CASE REPORT
A 30-year-old female was admitted to our hospital with headache and abdominal distension as well as pain, which had been present for 4 months. She had a history of VP shunt placement 4 years ago and two subsequent peritoneal catheter revisions due to peritoneal shunt obstruction. One operation was conducted under traditional laparotomy, and another operation was performed under laparoscopy. At admission, the blood routine examination and chest radiography were normal; specific IgG antibodies against T. solium cysticercus in the serum and cerebrospinal fluid were also assayed by enzyme-linked immunosorbent assay or immunofluorescence test and were negative. Neurological examination indicated memory deterioration which mainly present with amnesia for 3 months, but she had no suffering from ataxia or aconuresis. In addition, she also presented symptoms of higher intracranial pressure, and magnetic resonance imaging (MRI) revealed gradual increase in ventricular size [Figure 1]. An abdominal ultrasound scan showed excessive encapsulated effusion and that the catheter was enwrapped by omentum [Figure 2a and b]. At admission, brain MRI (3.0 T) scans showed hyperintensity on T1-weighted and T2-weighted images as well as rim enhancement following gadolinium injection [Figure 1b-d]. The volume of the cystic lesion is 6.0 cm × 6.5 cm × 4.0 cm. The primary diagnosis was suspected to be an arachnoid cyst with acquired hydrocephalus in the bilateral ventricular region. The patient underwent endoscopic cysternostomy [Figure 2c], rather than peritoneal catheter adjustment, and experienced a good recovery. The ventriculostomy of the left middle frontal gyrus was adopted to resect the lesion, the cysts of lesion-containing cysticercosis scolex were removed completely, and there was no rupture of cysts or serious adhesion with surrounding structures during operation. Histopathological examination of the excised cystic samples confirmed intraventricular NCC [Figure 2d], showing dead scolex infiltrated with neutrophils, eosinophils, and tegumental cells, as well as degenerative changes in the inner layer of the cyst wall. The patient's symptoms improved after 2 months of follow-up after the operation.
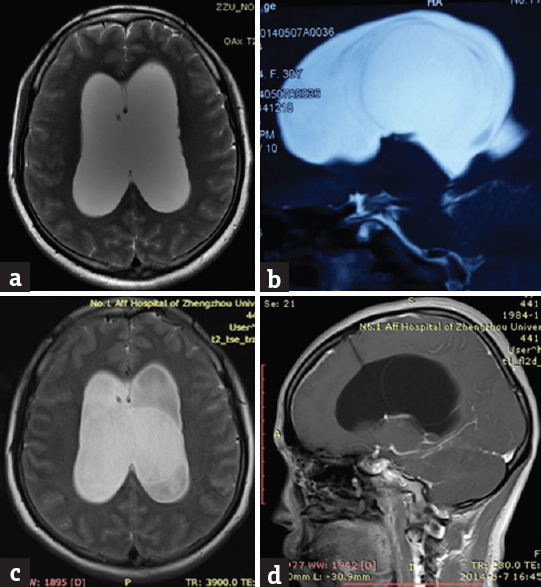
- Preoperative magnetic resonance imaging showed the cystic lesion in the ventricle. 0.5 T magnetic resonance imaging scans showed no lesion on T2 images (a); 3.0 T magnetic resonance imaging scans showed a cystic lesion on sagittal and axial T2 images (b and c); 3.0 T magnetic resonance imaging scans showed slight rim regular-enhancement after gadolinium injection on sagittal T1 images (d)

- Previous laparoscopy showed that the shunt was obstructed by inflammatory omentum, black dotted line showing peritoneal catheter, yellow arrow showing peritoneal catheter blockage by surrounding inflammatory omentum (a); abdominal ultrasound scans showed excessive encapsulated effusion (b); the cystic lesion was completely removed by endoscopic cysternostomy, no remnants of the cyst reach the parenchyma due to considerable slippery and gentle during operation. (c); Histopathology of excised cystic samples confirmed cysticercosis (H and E, ×40) (d)
DISCUSSION
VP shunt blockage is one of the most common complications of the shunt placement procedure and can include ventricular or peritoneal catheter obstruction. Previous studies reported that shunt blockage involving the ventricular end and requiring revision was observed in 26.4% of cases.[7] The rare cases of peritoneal catheter blockage after VP shunt placement have been not described in the literature, with only one report showing that spontaneous knot formation was responsible for peritoneal catheter blockage.[8] In contrast, the recurrent occurrence of peritoneal catheter blockage caused by NCC has not been reported in the literature.
There are several striking lessons that can be learned from the uncommon case presented in this report. First, early misdiagnosis occurred at the community hospital due to low-field MRI (0.5 T); these initial MRI results showed hydrocephalus in the bilateral ventricles but failed to detect the cystic lesion. Second, two revisions of the distal shunt due to peritoneal catheter blockage were performed unsuccessfully, and significant abdominal symptoms occurred after the operation, indicating the need to explore the possible causes for catheter revision failure on the peritoneal shunt. Third, a cystic lesion was highly suspected in the bilateral ventricles following 3.0 T MRI scans in our hospital; however, the primary diagnosis was still considered an arachnoid cyst, and cyst-peritoneal shunt adjustment was advocated by some members of the treatment team. Fortunately, endoscopic cysternostomy, rather than peritoneal catheter adjustment, was applied in this patient, and histopathological examination of excised cyst confirmed NCC. The repeated peritoneal shunt blockage was likely associated with an inflammatory reaction that generated abdominal encapsulated fluid.
The most common location of intraventricular NCC is the fourth ventricle.[9] However, the present case showed NCC located in both lateral ventricles, which was mistaken for an intraventricular arachnoid cyst. Therefore, arachnoid cysts should be differentiated from NCC. Neuroimaging with computed tomography (CT) or MRI is the most useful diagnostic method of NCC, but the cystercosis in the ventricles and subarachnoid space may not be visible on CT scan since the cyst fluid is isodense with the cerebrospinal fluid. MRI is more sensitive in the detection of intraventricular cysts, and enhanced MRI scans are helpful to evaluate the ventricular NCC; however, differentiation of NCC lesions from metastatic disease and pyogenic abscesses remains to be challenged; occasionally, the alternative examinations such as H nuclear MR spectroscopy, diffusion-weighted imaging, and MR perfusion imaging should be considered based on the previous literature.[10] In addition, the most serious complication caused by intraventricular cerebral cysticercosis is sudden death due to acute hydrocephalus.[11] Hence, based on our experience, the decision to operation should be made as soon as possible if the intraventricular cyst exhibits mass effect and cerebrospinal fluid obstruction.[12] The surgical management for ventricular NCC may be used by microsurgery or endoscopy. In the present patient, endoscopic cysternostomy represented an alternative effective treatment for the repeated shunt revisions for NCC with hydrocephalus; rare possible complication such as developing intraparenchymal calcifications and subsequent seizures due to remnants of cyst reached the parenchyma in the channel of the grasping forceps following endoscopic cysternostomy should be emphasized; consequently, regular neuroimaging should be performed to assess the surgical outcome in follow-up.
In summary, the present case highlights the need for increased awareness of NCC as a possible etiology of hydrocephalus, especially in developing countries. Uncommon findings in both lateral ventricles following low-field MRI scans as well as the rarity of this infection involved in unusual location play important roles in misdiagnosis and incorrect treatment for hydrocephalus; thus, endoscopic cysternostomy, rather than multiple shunt adjustment of the peritoneal end, is recommended in the selected patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Recent advances and perspectives in molecular epidemiology of Taenia solium cysticercosis. Infect Genet Evol. 2016;40:357-67.
- [Google Scholar]
- Major trends in human parasitic diseases in China. Trends Parasitol. 2010;26:264-70.
- [Google Scholar]
- Helminth infections of the central nervous system occurring in Southeast Asia and the Far East. Adv Parasitol. 2010;72:351-408.
- [Google Scholar]
- Clinical symptoms, diagnosis, and treatment of neurocysticercosis. Lancet Neurol. 2014;13:1202-15.
- [Google Scholar]
- Role of endoscopic third ventriculostomy and ventriculoperitoneal shunt in idiopathic normal pressure hydrocephalus: Preliminary results of a randomized clinical trial. Neurosurgery. 2013;72:845-53.
- [Google Scholar]
- Endoscopic observations of blocked ventriculoperitoneal (VP) shunt: A step toward better understanding of shunt obstruction and its removal. Br J Neurosurg. 2012;26:747-53.
- [Google Scholar]
- Ventriculoperitoneal shunt blockage due to spontaneous knot formation in the peritoneal catheter.Case report. J Neurosurg Pediatr. 2008;1:142-3.
- [Google Scholar]
- Imaging features and surgery-related outcomes in intraventricular neurocysticercosis. Neurosurg Focus. 2002;12:e6.
- [Google Scholar]
- Cysticercosis of the fourth ventricle causing sudden death: A case report and review of the literature. Pathol Oncol Res. 2009;15:143-6.
- [Google Scholar]
- A rare presentation of intracranial cysticercosis involving the cerebellopontine angle. J Clin Neurosci. 2013;20:892-4.
- [Google Scholar]






