Translate this page into:
Bedside Ultrasonography as an Alternative to Computed Tomography Scan for the Measurement of Optic Nerve Sheath Diameter
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Optic nerve sheath diameter (ONSD) as measured by optic nerve sheath ultrasonography (ONSU) is used as a surrogate marker of intracranial pressure (ICP), especially in resource-limited settings. There is a growing interest in the use of ONSU in emergency and high-altitude setups. Notwithstanding multiple studies done on this subject, there is a paucity of data regarding standardization of techniques and comparison of ONSU with computed tomography (CT).
Materials and Methods:
Thirty-five patients with a diagnosis of high-altitude cerebral edema were enrolled in the study. ONSD was measured in all patients using ONSU, along visual and coronal axis, and CT scan. We repeated ONSU in these patients on days 3, 7, 10, and 15 (day of discharge). Correlation between visual and coronal axis as well as CT scan was analyzed.
Results:
The correlation of visual to coronal and coronal to visual was equally significant (both correlation coefficients being R2 = 0.983). Correlation of ONSD by visual axis to CT scan was better than coronal axis (correlation coefficient R2 = 0.986 vs. 0.96, respectively).
Conclusion:
In our study, we found a strong correlation between the visual and coronal axes. Thus, either of the two axes can be used for monitoring ICP. However, it has been found that measurements along the coronal axis are challenging, especially in the emergency setup. ONSD measured along visual axis correlated better with CT scan as compared to the coronal axis.
Keywords
Computed tomography scan
high altitude
intracranial pressure
optic nerve sheath diameter
INTRODUCTION
Various studies in the past have shown optic nerve sheath diameter (ONSD) as a surrogate marker of intracranial pressure (ICP).[123] Due to its ease of access, faster turnover time, and no radiation exposure (when compared to investigations like computed tomograph [CT] scan), ONSD, as determined by optic nerve sheath ultrasonography (ONSU), is being increasingly employed to monitor ICP, especially in emergency and critical care setups.[14] There is growing interest in the role of ONSD in high-altitude illnesses owing to the common pathogenesis of raised ICP in these disorders.[567]
We endeavored to compare the coronal and visual axes to see the difference in the measurements in the settings of high-altitude illnesses and compare these measures to CT scan measurements.
MATERIALS AND METHODS
The study aimed to identify the ideal axis of ONSD measurement. The objectives were to compare ONSD by coronal/visual axes and assess which correlates better to the ONSD by computed tomography (CT). Power calculation suggested that a minimum of 28 ultrasounds were required to measure a difference of 0.5 mm in the ONSD measured by the three methods (α =0.05 and β =0.8). A total of 35 patients of an ongoing study on the role of ONSD in high-altitude cerebral edema (HACE) were included in the study (n = 35). ONSD was measured in all the patients simultaneously by both the coronal and visual axes. In brief, the patient was placed in a supine position and asked to look upward to a point in the ceiling. He was asked to close his left eye, with his right eye focusing on the center point at the ceiling. 7.5 Hz probe of Fuji Sonosite M Turbo® was used and ONSU was done in B-scan mode. For coronal axis measurement, the probe was placed inferior to the globe over maxillary and zygomatic process and directed medially. The ultrasound beam was projected superiorly and posteriorly. For visual axis measurement, the probe was placed over the closed eye. The ultrasound beam was projected posteriorly. Ultrasound gel was put in a hand glove rather than directly over the eye to avoid contact irritation. The average time for each scan was 1 min. ONSD was measured post ultrasound using onscreen calipers at 3 mm behind the globe, as it reflects the best measure of ICP.[8] The primary author did all the ultrasounds, and the onscreen measurement of the ONSD was carried out by the third author who was blinded to patient details and diagnosis. All patients underwent CT scan on day 1 of admission as part of the treatment protocol of HACE to rule out other organic disorders which closely mimic HACE. CT scan measurement of ONSD was carried out by the second author who was blinded to the patient diagnosis and ONSD measurements from ONSU. Later, a separate analysis to see the correlation between the recordings of ONSD by either axis and with the CT scan was done. The management of HACE was independent of the ONSD measurements done by ONSU.
All these patients were subjected to ONSD on the following days at regular intervals as per the predefined protocol (i.e., on days 3, 7, 10, and 15) till their discharge from the hospital. Statistical analysis was done using SPSS 17.0. The above study was cleared by the ethical committee of the hospital. Informed consent was taken from the patients as per the revised ethical guidelines for human experimentation of Helsinki Declaration of 2000.[9]
RESULTS
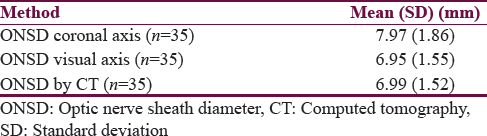
The study subjects were all male with an average age of 31.8 years. On the day of admission, the ONSD was measured in all 35 patients by all the three modalities (visual axis, coronal axis, and CT) [Table 1]. Moreover, 127 simultaneous recordings of ONSD were made on 35 patients during their hospital stay at regular intervals as per the defined study protocol [Table 1]. The correlation of visual to coronal and coronal to visual was equally significant (both correlation coefficients being R2 = 0.983) [Figure 1]. Correlation of ONSD by visual axis to CT scan was better than coronal axis (correlation coefficient R2 = 0.986 vs. 0.96, respectively) [Figure 2].

- Correlation of optic nerve sheath diameter measured by optic nerve sheath ultrasound along coronal and visual axes (n = 127). ONSD, Optic nerve sheath diameter; ONSU, Optic nerve sheath ultrasound

- Correlation between optic nerve sheath diameter along visual axis, coronal axis, and computed tomography scan (n = 35). ONSD, Optic nerve sheath diameter; ONSU, Optic nerve sheath ultrasound; CT scan, Computed tomography scan
DISCUSSION
Measurement of ONSD by ONSU is an easy modality to check for the changes in ICP.[11011] Since 2007, when Fagenholz et al. first described the role of ONSD in high-altitude illnesses,[7] there have been only six studies till date on the subject.[51213141516] The investigators in these studies have used various measurement techniques, with no consensus on the best method of measurement of ONSD.
In the study by Blehar et al., there was no correlation between both the axes (R = 0.51–0.69).[17] There were two major limitations in the above study as brought out by the authors, i.e., first, lack of a reference standard to show which of the two was more accurate, and second, ONSD measurements only in healthy individuals with no representation of diseased ONSD. We in our study addressed both these issues. First, we compared the ONSD in both the visual and coronal axes with CT scan, which is considered the gold standard for optic nerve sheath measurement. Second, to address the issue of representation of diseased ONSD, we measured ONSD in patient with HACE and followed them up till they recovered from the illness with regular ONSU as per the laid down study protocol. This helped us compare the ONSD between the visual and coronal axes for both diseased (raised ICP) and normal patients.
In our study, we found a strong correlation between the visual and coronal axes. Thus, either of the two axes can be used for monitoring ICP. However, from personal experiences, we have found that measurements along the coronal axis are challenging, especially in the emergency setup. Moreover, the corneal thickness changes in high altitude,[18] making the ONSD measurement less reliable along the coronal axis. In our study, the ONSD measured along visual axis correlated better with CT scan (R2 = 0.98) as compared to the coronal axis (R2 = 0.96). We further did Student's t-tests to compare the mean difference in ONSD as measured by CT scan and ONSU along coronal and visual axes. The mean difference in ONSD as measured by CT scan and coronal axis was 0.96 mm and statistically significant (P < 0.0001). The mean difference between CT scan and visual axis was 0.03 mm, and it was not statistically significant (P = 0.24). This suggests that the ONSD measured along the visual axis is in better agreement with CT scan as compared to coronal axis.
CONCLUSION
ONSD is a reliable index of ICP in critical care and resource-limited setup. In our study, we found that the ONSD measurements using bedside ONSU are comparable to CT scan.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Sonographic optic nerve sheath diameter as an estimate of intracranial pressure in adult trauma. J Surg Res. 2011;170:265-71.
- [Google Scholar]
- Use of the sonographic diameter of optic nerve sheath to estimate intracranial pressure. Am J Emerg Med. 2013;31:236-9.
- [Google Scholar]
- The incidence of increased ICP in ICU patients with non-traumatic coma as diagnosed by ONSD and CT: A prospective cohort study. BMC Anesthesiol. 2016;16:106.
- [Google Scholar]
- Ultrasonographic measured optic nerve sheath diameter as an accurate and quick monitor for changes in intracranial pressure. J Neurosurg. 2015;123:743-7.
- [Google Scholar]
- Optic nerve sheath diameter, intracranial pressure and acute mountain sickness on Mount Everest: A longitudinal cohort study. Br J Sports Med. 2008;42:183-8.
- [Google Scholar]
- Optic nerve sheath diameter correlates with the presence and severity of acute mountain sickness: Evidence for increased intracranial pressure. J Appl Physiol (1985). 2009;106:1207-11.
- [Google Scholar]
- Evidence for increased intracranial pressure in high altitude pulmonary edema. High Alt Med Biol. 2007;8:331-6.
- [Google Scholar]
- The subarachnoid space surrounding the optic nerves.An ultrasound study of the optic nerve sheath. Surg Radiol Anat. 1996;18:323-8.
- [Google Scholar]
- World Medical Association. World medical association declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79:373-4.
- [Google Scholar]
- Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med. 2007;33:1704-11.
- [Google Scholar]
- Sonographic assessment of the optic nerve sheath in idiopathic intracranial hypertension. J Neurol. 2011;258:2014-9.
- [Google Scholar]
- Optic nerve sheath diameter is not related to high altitude headache: A randomized controlled trial. High Alt Med Biol. 2012;13:193-9.
- [Google Scholar]
- Optic nerve sheath diameter and acute mountain sickness. Wilderness Environ Med. 2013;24:105-11.
- [Google Scholar]
- Ultrasonography of the optic nerve sheath diameter for diagnosis and monitoring of acute mountain sickness: A Systematic review. High Alt Med Biol. 2015;16:195-203.
- [Google Scholar]
- Oxidative stress response to acute hypobaric hypoxia and its association with indirect measurement of increased intracranial pressure: A field study. Sci Rep. 2016;6:32426.
- [Google Scholar]
- Multiparametric magnetic resonance investigation of brain adaptations to 6 days at 4350 m. Front Physiol. 2016;7:393.
- [Google Scholar]
- Correlation of visual axis and coronal axis measurements of the optic nerve sheath diameter. J Ultrasound Med. 2008;27:407-11.
- [Google Scholar]






