Translate this page into:
Clinico-radiologic Profile of Pediatric Traumatic Brain Injury in Western Rajasthan
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The aim of this study was to evaluate clinico-radiological profile and outcome of pediatric traumatic brain injury (TBI).
Design:
Prospective observational study
Setting:
Intensive Care Unit, ward and OPD of Pediatrics, Dr. S. N. Medical College, Jodhpur (tertiary care hospital).
Participants:
A total of 188 children (1 month–18 years) were enrolled and 108 admitted.
Intervention:
TBI classified as mild, moderate, or severe TBI. Neuroimaging was done and managed as per protocol. Demographic profile, mode of transport, and injury were recorded.
Outcome:
Measured as hospital stay duration, focal deficits, mortality, and effect of early physiotherapy.
Results:
Males slightly outnumbered females mean age was 5.41 ± 4.20 years. Fall from height was the main cause of TBI (61.11%) followed by road traffic accident (RTA) (27.78%). Majority (56.56%) reached hospital within 6 h of injury, out of which 27% of patients were unconscious. Mild, moderate, and severe grade of TBI was seen in 50%, 27.78%, and 22.22% of cases, respectively. About 12.96% of cases required ventilator support. The average duration of hospital stay was 11.81 ± 12.9 days and was lesser when physiotherapy and rehabilitation were started early. In all children with temporal bone fracture, magnetic resonance imaging (MRI) brain revealed a temporal lobe hematoma and contusion in spite of initial computed tomography (CT) head normal. Children who have cerebrospinal fluid (CSF) rhinorrhea/otorrhea had a high chance of fracture of base of skull and contusion of the basal part of the brain.
Conclusion:
In India, fall from height is common setting for pediatric TBI besides RTA. Early initiation of physiotherapy results in good outcome. MRI detects basal brain contusions in children presenting with CSF rhinorrhea/otorrhea even if initial CT brain is normal.
Keywords
Accidents
brain contusions
neuroimaging
traffic
INTRODUCTION
Traumatic brain injury (TBI) is a leading cause of death and disability following injury in children, adolescents, and young adults worldwide (WHO, 2009).[1] Nonetheless, most of our understanding, including clinical management of pediatric TBI is extrapolated from adults. Children are not just “little adults,” and there are many important distinctions between the developing and mature brain, particularly with regard to normal function, pathophysiological response to injury, recovery, and plasticity.[2] Many studies have reported the clinico-radiologic profile of TBI in the Western (Developed) world and appropriate management guidelines are in place.[3]
In India, apart from road traffic accidents (RTA), children are very vulnerable to accidents at home, farms, playground, school, etc. due to the lack of safety measures and effective legal regulations at all these places. There is, in general, nonavailability of on the spot resuscitation facility, poorly organized, equipped transport of patient and emergency services; lack of team approach the developing world like India.[4]
It is very obvious that the clinical and radiologic picture reported by the western literature does not provide appropriate and adequate information regarding TBI due to these accident/trauma situations, and hence very exclusive to India and other developing countries.[56] The current study was therefore conducted to find out the clinico-radiologic profile and outcome of Pediatric TBI in children presenting to the emergency room (ER)/trauma center attached to a tertiary Pediatric Hospital.
MATERIALS AND METHODS
The current study was conducted in the pediatric ER, Pediatric Intensive Care Unit (PICU), Pediatric Neurology clinic and ward of Department of Pediatrics, Dr. S. N. Medical College and attached Hospitals, Jodhpur during 2 years of study from November 2014 to October 2016. This study included all the children from 1 month to 18 years of age of trauma with clinical or radiological evidence of head injury with or without other injuries admitted in the Department of Pediatrics.
A data capture form was filled for each of the patient, which included all the details about the case such as patient profile, prehospital care, type and mode of injury, time to reach emergency department, general physical and neurological examination, radiological findings, management details, including physiotherapy and outcome. TBI severity was scored according to Glasgow Coma Score (GCS). Computed tomography (CT) or magnetic resonance imaging (MRI) scan of the brain in all patients and spine in some cases as indicated was done as early as possible. All patients were managed as per laid down standard[7] and departmental protocols. Based on the GCS patients were grouped as minor head injury (GCS 13–15), moderate head injury (GCS 9–12), and severe head injury (GCS 8 or less). Postresuscitation GCS was considered as baseline and discharge GCS was done to assess outcome. The progress, follow-up, and their final outcome were recorded by neurologic examination.
The data were analyzed using Microsoft Excel 2010. Continuous data of sample were summarized as a mean ± standard deviation, and categorical data of the sample were presented as proportion or percentage.
RESULTS
A total of 21,918 patients (all age groups) presented in the accident and trauma ER of our hospital. Out of these, a total of 1090 (4.97%) patients were diagnosed to have trauma to head region (with/without associated polytrauma) and out of the 1090 patients who had trauma to head region, 188 (17.25%) were between 1 month and 18 years of age. 80 (42.55%) children out of the 188 were asymptomatic and had a normal neurologic examination and normal CT brain (done in 48 children) and were discharged from the ER itself. These children were followed up after 7 days and were not found to be symptomatic or having any focal deficit.
Out of 188 children, 57.45% (mean age 5.41 ± 4.20 years, n = 108) required admission out of which 22% (n = 24) were admitted in PICU because of severe TBI and all of them required advanced airway management, including ventilation. Age and sex distribution of children admitted with TBI are shown in Table 1. Mean age of males was 6.08 ± 4.77 years and mean age of females was 4.53 ± 3.66 years. Overall two peaks were seen in children admitted with TBI, first in the age group of 1–3 years (38/108, 35%) and second between 6 and 14 years (36/108, 33%).
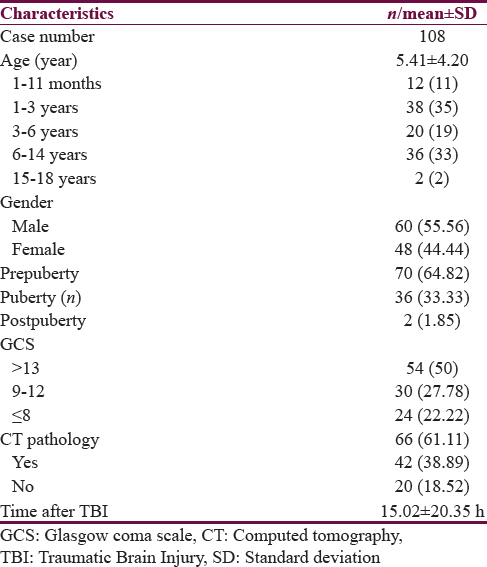
Mode of injury and time of presentation of admitted TBI patients are shown in Table 1. Fifty percent children arrived within 6 h of trauma, 35.11% of children arrived between 6 and 24 h of trauma, and 14.89% arrived between 24 and 72 h. In fact, 83% of children who arrived after 6 h had already sought consultation in another ER or hospital and were referred to our trauma center. Grading of TBI is shown in Figure 1.

- Severity of traumatic brain injury
Deficit at presentation and imaging findings of admitted TBI patients are shown in Table 2. Nearly 16.67% of patients presented with bleeding from ear immediately or within few hours of trauma and 11.11% had associated vomiting and 3.7% also had focal seizures. Nearly 77.78% of these children had a fracture base of the skull or temporal bone (22.2% had middle cranial fossa fracture, 44.4% had temporal bone fracture, and 11.11% had a frontoparietal bone fracture). In all eight patients who had a temporal bone fracture, the CT brain did not reveal any abnormality, but MRI brain revealed a temporal lobe hematoma and contusion in all these patients. Of all, 2.7% of children had cerebrospinal fluid (CSF) rhinorrhea, and all of them had a fracture of the cribriform plate of the ethmoid bone with contusion of the ipsilateral basifrontal region. Of these, 66.7% developed recurrent meningitis despite a good initial recovery in the first 6 months post-TBI and they required endoscopic repair of the fracture of cribriform plate. In this study, it is amply clear that a MRI brain should be conducted in all children with TBI because in approximately 31.5% (34/108) of children with a normal CT head had an abnormal MRI brain performed within 72 h of CT head [Table 3].


Hospital stay of these children varied from <24 h to 60 days with an average 11.81 ± 12.9 days. In all the admitted children formal physiotherapy and rehabilitation was started immediately or as early as possible as per protocol except for children who had multiple fractures due to polytrauma or who had cardiopulmonary instability. Early physiotherapy and its effect on outcome in terms of hospital stay and deficit at discharge and 6 months is shown in Table 4. The mean hospital stay was lesser in children having moderate (10.23 ± 3.33 days vs. 12.2 ± 0.99 days) and severe TBI (13 ± 2.82 days vs. 18.56 days) in whom physiotherapy and rehabilitation were early as compared to children in whom it was started late.

Thirty (27.78%) children had features of raised intracranial tension (ICT), and all of them were treated with the recommended protocol for TBI, including maintenance of fluid and electrolyte balance, antibiotics only if indicated due to infected wounds, anticonvulsants, decongestants, oxygenation, and ventilation as indicated. Orthopedic management was required in 6 (5.56%) children who had fractures and included plastering with immobilization. None of the children required nailing or operative intervention. Phenytoin was used initially in 15 children with severe TBI and was replaced by levetiracetam in 10 children because of excessive sedation interfering with assessment of sensorium.
DISCUSSION
TBI is the leading cause of mortality, morbidity, and socioeconomic losses in India. TBI accounts for 24% of all injuries due to road traffic injuries (RTI) among hospital-based victims. As per NCRB 2005, the prevalence of RTA deaths is 90 per million in India and 111 per million in Rajasthan. Most of the data are on adults, and it has been reported that RTI a is leading cause of TBI in India accounting for 45%–60% of TBI, and falls account for 20%–30% of TBI, paralleling the findings from global disease study.[8] We are lacking data in children, especially in India and Rajasthan. According to NCRB, children under the age of 15 years account for only 6.4%/deaths due to RTI. In adults, RTA constitutes the most important cause of TBI.
In Yemen, home-based causes were the dominant cause, and RTI was the second leading cause of TBI.[9] Males account for more than two-third of patients as found in studies conducted in Pakistan, Singapore, and China.[101112] Yet all these studies were adult based. Over 8.75 lakh children die every year as a result of injuries. In India, children between 1 and 15 years constitute about 35% of the total population. In India, Gururaj reported the incidence, mortality and case fatality rates due to TBI were 150/1 lakh, 20/1 lakh, and 10%, respectively.[8] In Taiwan male:female ration was 1.6:1 with RTI accounting for 47% and falls for 40% of the cases.[13] In the current study also 55.56% of children were male.[11] However, males, as usual, are slightly predominating in numbers because for trivial injury, females may not be brought for medical consultation as is especially true for rural India. In another study reported from Kashmir the males predominated at all ages.[14] Chiaretti et al. hypothesized that the higher incidence of TBI in boys might be due to larger head circumference, more muscular and physical activities in comparison to girls.[15] In our study, boys outnumber girls in the incidence. We do believe the hypothetical factors, described by Chiaretti et al., might contribute to the higher incidence of TBI in boys in our study.
We observed two peaks in children admitted with TBI, first in the age group of 1–3 years and between 6 and 14 years. This was interesting to note because the younger age group (1–3 years) mostly had TBI because of a fall either from their home terrace, balcony or a construction site. This raises a very critical point related to child (especially toddlers) safety in this country and reflects the poor safety measures at both home and unfortunately construction sites. Infants and Toddlers in developing world are taken to the construction sites by parents because there is no one left at home to look after them in a typical lower socioeconomic urban family where only one generation migrated to the city. Studies specifically looking into the health issues of children at construction sites are required to further elaborate on many of these issues. In a study by Sharma M, Lahoti BK performed in a single tertiary center of India, 13% of children admitted in pediatric facilities were admitted because of trauma and the mean age of presentation was 6.3 years.
In this study, fall from height (64%) was the most common mode of injury followed by RTA (27.5%). This is very unlike the western data where home accidents are rare and most of the TBI in this age group is because of car accidents or child abuse. This observation is highly disturbing as home seems to be the more dangerous place for children than roads contrary to the belief. This is because most of the homes in the urban area are just makeshift houses with the incomplete construction where stairs and terraces do not have a safety rail or barricading. The data from the current study, therefore, makes a persuasive case for improvement in safety standards and criteria while constructing houses in the future. Children of laborers at a construction site and at farms are also very vulnerable to injury due to falls and inflicted by animals and therefore separate designated and cordoned off areas for infants, toddlers and small children should be made available by the construction contractors and other responsible people. Mahapatra and Kumar[16] and Bhargava et al.[17] concluded in their study that fall from a height as the most common mode of injury in TBI followed by RTA in children.
Only 50% of children arrived within 6 h of trauma. In fact, 83% of children who arrived after 6 h had already sought consultation in another ER or hospital and were referred to our trauma center. Time of arrival was similar to other studies looking into this aspect in an Indian scenario.[181920] However, these observations necessitate the development of a very efficient transport system to manage these children on the site of accident and immediately transport them to the nearest well-equipped facility to improve their outcome. In the current study, it is extremely unfortunate that only 12.5% of children were transported to the hospital by an ambulance equipped with oxygen and emergency medical personnel (driver cum nursing personnel). In the developed world the transport of sick/injured patients is highly organized and has reduced morbidity and mortality significantly.[21] Despite an exponential increase in the number of hospitals catering to critically ill children and adults, there has been no serious attempt to improve cost-effective and appropriate transportation of trauma victims/critically ill patients in this country. A highly organized free/subsidized emergency transport system is the need of the hour. Among children who required admission, most cases were of mild TBI followed by moderate and severe TBI. Satapathy et al.[6] found the similar incidence of mild (56.47%), moderate (29.25%) and severe TBI (14.28%) in the pediatric population as our study.
In this study, it is evident that almost 77.8% of children who have bleeding from ear or nose will have an associated fracture skull. This is not a new observation but is often overlooked in a very busy ER, and by this study, it is restressed that history of bleeding from ear or nose should always be asked emphatically. It was also noted in the current study that children who had fracture in the middle cranial fossa or temporal bone also had an underlying contusion and or hematoma of the ipsilateral temporal lobe which was missed in the screening CT head region and is only picked up on an MRI brain. Two patients who had middle cranial fossa fracture with right parietal region hypodensity on CT brain were subsequently found to have acute right MCA territory infarct on MRI brain. Therefore, the results of this study clearly emphasize that in a child having pediatric trauma to head region and having a history of ear bleeding, an MRI should be performed even if CT brain is normal which helps in planning appropriate management and reduce morbidity in these children. Various studies in India on children found similar finding on neuroimaging as our study.[61718]
Levetiracetam instead of phenytoin can be recommended to be an initial medication even in trauma settings. In the current study, continuous 3% saline infusion was used to treat raised ICT along with other standard measures.[7] It was not associated with any significant side effects including hypernatremia. More studies are required to compare continuous 3% NS infusion with other decongestant agents, including mannitol to review its recommendations in pediatric TBI.
TBI is one of the most common forms of acute brain injury globally and is associated with a high morbidity and mortality. It is also associated with a very high chance of long-term neurodevelopmental sequele leading to a serious financial, social, and medical burden over the community. Six months neurologic outcome of children in whom physiotherapy and neurorehabilitation were started early. Overall only 13% of children continued to have severe deficits at the end of 6 months. Although not exactly a good outcome when compared to the other studies this is a much better outcome.[22]
In the current study, one of the objectives was to find out the relationship of the mode of injury or fall with the exact anatomic location and extent of brain injury. In this regard, even an extensive history from all available attendants and eyewitnesses could not give us an exact detail of the injury/fall/mode with the spatial details of the child during the accident. Therefore, we could not elucidate this relationship despite being one of the objectives.
In the current study, predictors of the presence of a radiological contusion in the brain/or any other finding related to TBI (including hemorrhage, midline shift, skull, or skull base fractures) included severe TBI (GCS < 8), hemorrhagic or clear fluid (CSF) discharge from ear or nose, seizures within first 24 h of trauma, altered sensorium persisting >34 ± 2.3 h and clinical features of raised ICT. In these children, MRI brain is recommended to evaluate the extent of radiologic brain injury, even if initial screening CT scan is normal.
Limitations
Although the current study was performed in the biggest tertiary referral center of Western Rajasthan, a few patients may have not been referred to this center and therefore missed in the data presented here. Besides those with very severe injuries who died en route to the hospital were also not included and therefore exact factors and causes of mortality due to severe TBI in these children could not be included. Furthermore, children with mild injuries may not have sought clinical care and therefore bias the observations. This study also missed analysis of children with TBI who were never admitted to pediatric wards (e.g., admitted and discharged from trauma ICU or neurosurgery).
CONCLUSION
Early intervention for raised ICT and physiotherapy significantly improves long term neurological outcome. MRI should be the investigation of choice in children of TBI with ear nose bleed/discharge and basi-cerebral contusions should always be suspected and ruled out in these children even if initial CT is normal. Guidelines for safety of children at construction sites, playground and even at home (related to its child friendly construction) should be developed jointly by pediatricians, trauma experts, child support groups, and architects. Knowledge about the causes, pattern, and distributions about TBI in pediatric age group from this study will be extremely helpful in policymaking, research, health management, and rehabilitation at the national level in our country and other developing nations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Neuroprotective measures in children with traumatic brain injury. World J Crit Care Med. 2016;5:36-46.
- [Google Scholar]
- Lasting effects of pediatric traumatic brain injury. Indian J Neurotrauma. 2006;31:19-26.
- [Google Scholar]
- Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents – Second edition. Pediatr Crit Care Med. 2012;13(Suppl 1):S1-82.
- [Google Scholar]
- Clinical practice experiences in diagnosis and treatment of traumatic brain injury in children: A Survey among clinicians at 9 large hospitals in China. PLoS One. 2015;10:e0142983.
- [Google Scholar]
- The prevalence of traumatic head injury seen in a tertiary health facility in North-central Nigeria. Int J Public Health Res. 2015;3:127-9.
- [Google Scholar]
- Spectrum and outcome of traumatic brain injury in children <15 years: A tertiary level experience in India. Int J Crit Illn Inj Sci. 2016;6:16-20.
- [Google Scholar]
- Neurologic emergencies and stabilization. In: Kliegman RK, ed. Nelson Textbook of Pediatrics (20th ed). Philadelphia: Elsevier; 2016. p. :508-12.
- [Google Scholar]
- Epidemiology of traumatic brain injuries: Indian scenario. Neurol Res. 2002;24:24-8.
- [Google Scholar]
- The epidemiology of brain injury and the organization of health care to victims in Aden (Yemen) Zh Vopr Neirokhir Im N N Burdenko. ;2:40-2.
- [Google Scholar]
- The burden of road traffic injuries in developing countries: The 1st national injury survey of Pakistan. Public Health. 2004;118:211-7.
- [Google Scholar]
- Investigating gender differences in outcome following severe traumatic brain injury in a predominantly Asian population. Br J Neurosurg. 2006;20:73-8.
- [Google Scholar]
- Pediatric traumatic brain injuries in Taiwan: An 8-year study. J Clin Neurosci. 2004;11:126-9.
- [Google Scholar]
- The incidence and severity of injury in children hospitalised for traumatic brain injury in Kashmir. Injury. 2006;37:410-5.
- [Google Scholar]
- The impact of initial management on the outcome of children with severe head injury. Childs Nerv Syst. 2002;18:54-60.
- [Google Scholar]
- Pediatric head injury. In: Mahapatra AK, Kumar R, Kamal R, eds. Textbook of Head Injury. Delhi: Jaypee Publ; 2012. p. :180-90.
- [Google Scholar]
- Epidemiology and clinical characteristics of traumatic brain injuries in a rural setting in Maharashtra, India 2007-2009. Int J Crit Illn Inj Sci. 2012;2:167-71.
- [Google Scholar]
- Demographic profile, clinical presentation, management options in cranio-cerebral trauma: An experience of a rural hospital in Central India. Pak J Med Sci. 2007;23:724-7.
- [Google Scholar]
- Brain injury and prehospital care: Reachable goals in India. Indian J Neurotrauma. 2009;6:5-10.
- [Google Scholar]
- Benchmarking prehospital and emergency department care for argentine children with traumatic brain injury: For the South American Guideline Adherence Group. PLoS One. 2016;11:e0166478.
- [Google Scholar]
- Advanced neuromonitoring and imaging in pediatric traumatic brain injury. Crit Care Res Pract 2012 2012 361310
- [Google Scholar]






