Translate this page into:
Evaluation of Predictive Factors Influencing Community Reintegration in Adult Patients with Stroke
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
Patients with stroke are faced with gait, balance, and fall difficulties which could impact on their community reintegration. In Nigeria, community reintegration after stroke has been understudied. The objective of this study was to evaluate the predictors of community reintegration in adult patients with stroke.
Materials and Methods:
Participants were 91 adult patients with stroke. Gait variables, balance self-efficacy, community balance/mobility, and fall self-efficacy were assessed using Rivermead Mobility Index, Activities-specific Balance Confidence Scale, Community Balance and Mobility Scale, and Falls Efficacy Scale-International respectively. Reintegration to Normal Living Index was used to assess satisfaction with community reintegration. Pearson Product-Moment Correlation Coefficient was used to determine the relationship between community reintegration and gait spatiotemporal variables, balance performance, and risk of fall. Multiple regression analysis was used to determine predictors of community reintegration (P ≤ 0.05).
Results:
There was significant positive relationship between community reintegration and cadence (r = 0.250, P = 0.017), functional mobility (r = 0.503, P = 0.001), balance self-efficacy (r = 0.608, P = 0.001), community balance/mobility (r = 0.586, P = 0.001), and duration of stroke (r = 0.220, P = 0.036). Stride time (r = −0.282, P = 0.073) and fall self-efficacy (r = 0.566, P = 0.001) were negatively correlated with community reintegration. Duration of stroke, balance self-efficacy, community balance/mobility, and fall self-efficacy (52.7% of the variance) were the significant predictors of community reintegration.
Conclusion:
Community reintegration is influenced by cadence, functional mobility, balance self-efficacy, community balance/mobility, and duration of stroke. Hence, improving balance and mobility during rehabilitation is important in enhancing community reintegration in patients with stroke.
Keywords
Balance
community reintegration
gait
mobility
stroke
INTRODUCTION
Individuals with stroke are faced with gait and balance difficulties which could impact on their community reintegration. For many people, the reintegration into community life marks the end point of their rehabilitation.[1] As far as community ambulation is concerned, little is known about the dimensions of the task and the specific attributes required for its safe and independent execution.[2] Moreover, it is documented that individuals with chronic stroke often exhibit considerable gait impairments that significantly impact on their quality of life[3] and reintegration to living in the community.
Many studies have been carried out on factors associated with community reintegration to normal living after stroke.[4567891011] Findings by Murtezani et al. revealed that patients with stroke with stronger reintegration have a better outcome of daily activities and quality of life while those with severe gait disability present with poor activities of daily living (ADL) and subsequent poor community reintegration.[6] Ability to walk amidst stroke survivors is an extremely required goal[12] and a measure of recovery by both patients and their families.[1314] Thus, ability to reintegrate them back into the community is very important.
Individuals with stroke duration of >6 months have shown less satisfaction with community reintegration suggesting a possible deterioration of community reintegration over time.[15] Therefore, it is important to identify and explore the determinants and associated factors (physical and psychological) of satisfaction with community reintegration as well as the existing relationships between each of the factors and community reintegration. Hence, this study was designed to evaluate the predictors of community reintegration in adult patients with stroke.
MATERIALS AND METHODS
The participants for the study were drawn from a population of adult patients with stroke referred for outpatient rehabilitation in two public hospitals in Lagos, Nigeria. The inclusion criteria were stroke duration of 6 months or more, ability to walk 10 m unaided, ability to maintain balance for at least 30 s, and scoring ≥3 on Functional Ambulation Category/Classification scale. Participants with severe lower limb musculoskeletal problems and those with visual, verbal, and cognitive difficulties were excluded from the study. A total of 101 patients were recruited using purposive sampling technique. Three declined participation and seven did not meet inclusion criteria. A total of 91 participants completed the study. Ethical approval was obtained from Health Research and Ethics Committees of the two hospitals. Informed consent was obtained from the participants before they were enrolled in the study.
Gait variables, balance self-efficacy, community balance/mobility, and fall self-efficacy were assessed using Rivermead Mobility Index, Activities-specific Balance Confidence (ABC) Scale, Community Balance and Mobility (CB&M) Scale, and Falls Efficacy Scale-International (FES-I) respectively. The Reintegration to Normal Living Index (RNL-I) was used to assess satisfaction with community reintegration.
Outcome measures
The ABC Scale is a 16-item self-report measure in which patients rate their balance confidence for performing activities. It measures functional balance and perceived balance self-efficacy.[16] Confidence of the patients is evaluated using 16 functional activities, 9 of which are outside the home.[1] Items are rated based on an 11-point scale that ranges from 0 to 100. ABC has excellent test-retest reliability[17] and excellent internal consistency.[18]
CB&M Scale was used to evaluate balance and mobility. Participants were instructed to carry out 13 functional tasks and were scored on the first trial. A second trial was allowed only if the individual did not understand the task. The therapist judged the patient's performance in comparison to a young adult with normal neuromusculoskeletal system. There was a rest period between the tasks, and if in the therapist's clinical judgment the patient would be unsafe in performing part or all of a task, the participant was not allowed to attempt it. Scoring was done according to the part of the task attempted or “0” if it was not attempted.
FES-I was used to evaluate fall efficacy. FES-I is a short, easy-to-administer tool that measures the level of concern about falling during social and physical activities inside and outside the home whether or not the person actually does the activity. Participants were asked to rate their level of concern about falling while performing the tasks/activities. The level of concern was measured on a 4-point Likert scale (1 = not at all concerned to 4 = very concerned).[19]
The RNL-I was used to assess community reintegration. Participants were asked how much they agree with each item. The items include indoor, community, and distance mobility, self-care; daily activity, recreational and social activities; family role(s); personal relationships; presentation of self to others and general coping skills. Each of them was rated on a 4-point ordinal scale (1–4) with higher scores indicating a higher level of satisfaction. The scores for each item were summed and then normalized to 100, with a score of 100 indicating that the participants were fully satisfied; scores of 60–99 indicating mild-to-moderate restrictions in self-perceived community reintegration; and scores < 60 indicating severe restrictions in self-perceived community reintegration.[20]
Data analysis
Data were analyzed using Statistical Package for Social Sciences (SPSS) version 20.0 software (SPSS Inc., Chicago, Illinois, USA). Pearson Product-Moment Correlation Coefficient was used to evaluate the relationship between community reintegration and each of balance, mobility, and risk of fall. Multiple regression analysis was used to identify the predictors of community reintegration as well as determinants of satisfaction with community reintegration and the respective/collective contribution of such predictors.
RESULTS
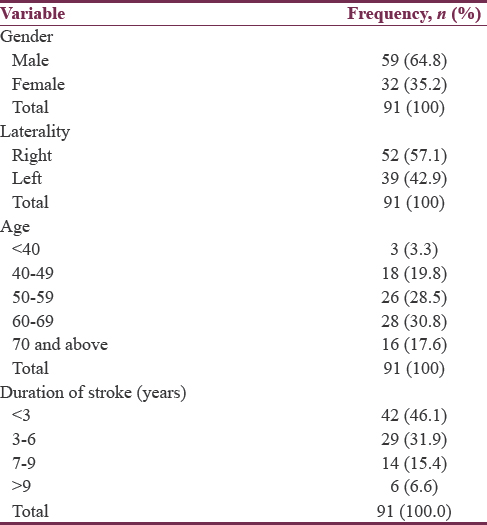
A total of 91 patients took part in the study. They comprised 59 males (64.8%) and 32 females (35.2%). Fifty-two (57.1%) participants had right hemiplegia while 39 (42.9%) participants had left hemiplegia. Twenty-eight (30.8%) participants were within the age range of 60–69 years while 3 (3.3%) were < 40 years of age. Duration of stroke was < 3 years in 42 (46.1%) participants while 6 (6.6%) have had stroke for >9 years [Table 1].
The relationships between community reintegration (RNL-I scores) and each of age, functional mobility, and duration of stroke are shown in Table 2. There was significant positive relationship between community reintegration and duration of stroke (r = 0.220, P = 0.036) as well as functional mobility (r = 0.503, P = 0.001). The relationships between community reintegration and each of gait spatiotemporal variables, balance performance, and risk of fall are shown in [Table 3]. There was significant positive relationship between community reintegration and cadence (r = 0.250, P = 0.017), balance self-efficacy (r = 0.608, P = 0.001), and community balance/mobility (r = 0.586, P = 0.001). Stride time (r = −0.282, P = 0.073) and fall self-efficacy (r = 0.566, P = 0.001) were negatively correlated with community reintegration.


The result of the multiple regression analysis used to evaluate the contributions of selected gait spatiotemporal variables, balance performance variables, fall self-efficacy, and duration of stroke to satisfaction with community reintegration is shown in [Table 4]. Duration of stroke (P = 0.01), balance self-efficacy (P = 0.02), community balance/mobility (P = 0.01), and fall self-efficacy (P = 0.03) were significant determinants/predictors of community reintegration. A total of 53% of the variance in the RNL-I scores was predicted/explained by the final regression model (F4(df = 86)= 23.99, P = 0.01). AmongAmong the predictors/independent variables, community balance/mobility (Standardized coefficient [β] = 0.34) had the strongest contribution and largest effect on community reintegration closely followed by balance self-efficacy (β = 0.26) and duration of stroke (β = 0.23) [Table 4].

DISCUSSION
The main aim of this study was to evaluate the predictors of community reintegration in adult patients with stroke. There was significant positive relationship between community reintegration and duration of stroke as well as functional mobility. Furthermore, there was significant positive relationship between community reintegration and cadence, balance self-efficacy, and community balance/mobility. Stride time and fall self-efficacy were negatively correlated with community reintegration. Duration of stroke, balance self-efficacy, community balance/mobility, and fall self-efficacy were significant determinants/predictors of community reintegration. About 53% of the variance in the community reintegration scores was explained by the final regression model. Among the predictors/independent variables, community balance/mobility had the strongest contribution and largest effect on community reintegration.
In Africa, the relationship between community reintegration and physical parameters (gait spatiotemporal variables, community balance/mobility, and functional mobility) and psychological parameters (balance self-efficacy and fall self-efficacy) in adult stroke survivors had not been fully explored in many studies. The results of the present study showed statistically significant moderate positive relationship between functional mobility and community reintegration. Thus, enhanced functional mobility ensures better reintegration into the community. Independent walking ability is a prerequisite to performing most daily tasks and activities;[2122] and accomplishing a task either physical or social task cannot be achieved without attaining certain level of functional mobility. The findings of this study also revealed a significant positive relationship between community reintegration and duration of stroke. This implies that the longer the poststroke duration, the better the reintegration into the community. As the participants got involved with gait retraining, balance performance, and related rehabilitation activities they tend to adapt more to environmental demands. This increases their level of community participation, reduces societal stigmatization/segregation and there is subsequent improvement in community reintegration. A similar finding of better community reintegration with longer poststroke duration was reported in an earlier study.[7]
Balance dysfunctions in stroke survivors appear to be common and have a significant impact on functional independence and overall recovery of the patient. According to the results of this study, there was significant positive relationship between community reintegration and cadence, balance self-efficacy and community balance/mobility. However, stride time and fall self-efficacy were negatively correlated with community reintegration. Balance problems have been implicated in poor recovery of ADL and mobility and an increased risk of falls.[23] This also explained why improved balance performance could likely minimize the risk of falling and ensure better societal participation. Impairment in balance regulation and the consequent increase fall risk result in high economic and social cost[24] and this could impact on community reintegration of stroke survivors. Balance forms the foundation for all voluntary motor skills; hence, recovery of balance impairment and disabilities serves as crucial part of stroke rehabilitation[25] and reintegration into the community. After a stroke, gait patterns are frequently slow and spatiotemporally asymmetric.[26] This is purported to lead to decreased balance, which is of particular concern, as impaired balance can subsequently lead to falls and injury.[27]
The result of this study showed that duration of stroke, balance self-efficacy, community balance/mobility, and fall self-efficacy were the significant predictors/determinants of community reintegration. The coefficient of determination (R2) of the final regression model showed that 53% of the variance in community reintegration is explained/accounted for by these factors. In previous studies,[59] the same factors explained smaller amount of variance in community reintegration. Among the predictor variables, community balance/mobility had the strongest contribution and largest effect on community reintegration, contributing about 27% to total coefficient of determination. This may be due to the fact that it entails activities that basically translate to most activities required in normal day-to-day human life. Balance self-efficacy also had significant contribution to community reintegration. This could be because balance self-efficacy is concerned with balance confidence, functional activity, and physical functioning of the participants. Duration of stroke also had fairly large contribution and effect on community reintegration implying that the more the poststroke duration, the better the community reintegration.
CONCLUSION
The factors that could influence community reintegration include cadence, functional mobility, balance self-efficacy, community balance/mobility, and duration of stroke. Furthermore, the less the stride time and fall self-efficacy, the better the community reintegration. Hence, improving balance and mobility during rehabilitation is important in enhancing community reintegration in patients with stroke.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Walking in the real world: Concepts related to functional gait. N Z J Physiother. 2007;35:126-30.
- [Google Scholar]
- Abnormal joint torque patterns exhibited by chronic stroke subjects while walking with a prescribed physiological gait pattern. J Neuroeng Rehabil. 2008;5:5-19.
- [Google Scholar]
- Measurement of community ambulation after stroke: Current status and future developments. Stroke. 2005;36:1457-61.
- [Google Scholar]
- Determinants of satisfaction with community reintegration in older adults with chronic stroke: Role of balance self-efficacy. Phys Ther. 2007;87:282-91.
- [Google Scholar]
- Factors associated with reintegration to normal living after stroke. Med Arch. 2009;63:216-9.
- [Google Scholar]
- Community reintegration in stroke survivors in Osun, Southwestern Nigeria. Afr J Neurol Sci. 2010;29:428-31.
- [Google Scholar]
- Participation in community walking following stroke: Subjective versus objective measures and the impact of personal factors. Phys Ther. 2011;91:1865-76.
- [Google Scholar]
- Community reintegration in stroke survivors: Relationship with motor function and depression. Hong Kong Physiother J. 2013;1:6-10.
- [Google Scholar]
- Functional ability, community reintegration and participation restriction among community-dwelling female stroke survivors in Ibadan. Ethiop J Health Sci. 2014;24:43-8.
- [Google Scholar]
- Arm and leg impairments and disabilities after stroke rehabilitation: Relation to handicap. Clin Rehabil. 2003;17:666-73.
- [Google Scholar]
- Exercise training improves walking function in an African group of stroke survivors: A randomized controlled trial. Clin Rehabil. 2011;25:442-50.
- [Google Scholar]
- Stroke rehabilitation: When should ambulation commence. J Niger Med Rehabil Ther. 2002;7:23-25.
- [Google Scholar]
- Effect of treadmill exercise training on spatial and temporal gait parameters in subjects with chronic stroke: A preliminary report. J Rehabil Res Dev. 2008;45:221-8.
- [Google Scholar]
- Changes in the quality of life of hemiplegic stroke patients with time: A preliminary report. Am J Phys Med Rehabil. 1999;78:19-23.
- [Google Scholar]
- The activities-specific balance confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28-34.
- [Google Scholar]
- Measurement properties of the activities-specific balance confidence scale among individuals with stroke. Disabil Rehabil. 2005;27:156-63.
- [Google Scholar]
- Psychometric evaluation of the original and Canadian French version of the activities-specific balance confidence scale among people with stroke. Arch Phys Med Rehabil. 2006;87:1597-604.
- [Google Scholar]
- Development and initial validation of the falls efficacy scale-international (FES-I) Age Ageing. 2005;34:614-9.
- [Google Scholar]
- Canadian Partnership for Stroke Recovery. Reintegration to Normal Living Index. 2017. Available from: http://www.strokengine.ca/assess/rnli/
- [Google Scholar]
- Gait training strategies to optimize walking ability in people with stroke: A synthesis of the evidence. Expert Rev Neurother. 2007;7:1417-36.
- [Google Scholar]
- Gait and balance performance of stroke survivors in South-Western Nigeria – A cross-sectional study. Pan Afr Med J. 2014;17(Suppl 1):6.
- [Google Scholar]
- Risk factors for falling in home-dwelling older women with stroke: The women's health and aging study. Stroke. 2003;34:494-501.
- [Google Scholar]
- Analysis and comparison of the psychometric properties of three balance measures for stroke patients. Stroke. 2002;33:1022-7.
- [Google Scholar]
- Clinical management of the patient with a postural control disorder. In: Shumway-Cook A, Woollacott MH, eds. Motor Control: Theory and Practical Applications (2nd ed). Baltimore: Lippincott Williams & Wilkins; 2001. p. :248-70.
- [Google Scholar]
- Changes in gait symmetry and velocity after stroke: A cross-sectional study from weeks to years after stroke. Neurorehabil Neural Repair. 2010;24:783-90.
- [Google Scholar]
- Balance score and a history of falls in hospital predict recurrent falls in the 6 months following stroke rehabilitation. Arch Phys Med Rehabil. 2006;87:1583-9.
- [Google Scholar]






