Translate this page into:
The Evolving Pattern and Outcome of Stroke at Moderate Altitude
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The people residing in hills of this Sub-Himalayan region traditionally have a distinct lifestyle involving high level of physical activity. However, increased urbanization in the last two decades has led to changes in lifestyle of people. The present study was an endeavor to document changes in the pattern of stroke in people residing at moderate altitude.
Aim:
This study was aimed to study the evolving trends in clinical profile, risk factors, and outcome at 3 months in hospitalized patients of stroke in a Tertiary Care Hospital situated at moderate altitude.
Setting and Design:
This prospective, observational study was carried out in a Tertiary Care Hospital, situated at 2000 m mean sea level, from July 2014 to June 2015 in Sub-Himalayan region of India.
Methods:
The clinical features and risk factors profile of 235 patients of stroke consecutively admitted in hospital were analyzed, and findings were expressed in percentage. The profile was compared with a study conducted at this institute 15 years back. The outcome of patients at 3 months in terms of modified Rankin Scale >3 (mRS) and Barthel Index <60 (BI) was also studied.
Results:
The occurrence of stroke as a cause of hospitalization was decreasing. Ischemic stroke was noted in 74%, and 26% had hemorrhagic stroke (HS). There was male predominance (58%), but affliction of females with stroke increased from 34% to 42%. The altered sensorium (P = 0.00) and neurological weakness (P = 0.024) were significantly associated with poor outcome in stroke. The occurrence of hypertension, diabetes mellitus, and coronary artery disease increased but smoking decreased among indoor patients of stroke in the last 15 years. Poor outcome of 203 patients at 3 months follow-up in terms of mRS >3 was 79 (IS-47, HS-32) but in term of BI, 63 (IS-32, HS-31) had poor outcome. Overall HS had poorer outcome. Age >70 years, female sex, altered sensorium, hypertension, and diabetes mellitus, were observed as poor prognostic factors, but the association was significant with advanced age, headache, and altered sensorium.
Conclusion:
The occurrence of stroke decreased among hospitalized patients. Hypertension, diabetes mellitus, and coronary artery disease increased but smoking decreased among patients of stroke.
Keywords
Moderate altitude
outcome
stroke
INTRODUCTION
Stroke is the second most common cause of death and fourth leading cause of disability worldwide.[1] In India, the overall age-adjusted prevalence rate for stroke is estimated between 84 and 262/100,000 in rural and between 334 and 424/100,000 in urban areas, and the adjusted annual incidence (per 100,000 persons) of stroke is 124 in rural area and 145 in urban area.[1] The World Health Organization defines stroke as “rapidly developing clinical signs of focal or global disturbance of cerebral function with symptoms lasting >24 h or leading to death with no apparent cause other than a vascular origin”. This definition includes subarachnoid hemorrhage but excludes transient ischemic attack (TIA), subdural hematoma, and hemorrhage or infarction caused by infection or tumor.[2] Patients with highest risk, benefit more from effective risk reduction. Early recognition of poor prognostic factors may help in the identification of those patients who are at greatest risk of early death or recurrence, and for whom early intervention may be considered, and thus, poor long-term outcome can be prevented.[3] History of diabetes mellitus, a severe neurological deficit at presentation, and total anterior circulation stroke was found to be predictors of an unfavorable outcome.[4]
Among 30-day survivors of the first-ever stroke, about half survive 5 years; of survivors, one-third remain disabled, and 1 in 7 remain in permanent institutional care.[5]
We analyzed clinical profile of patients of stroke at our institute situated at moderate altitude (2000 m mean sea level [MSL]) in the year 1999–2000 which was published in 2004.[6] Our institute is situated in a state in North-West part of India and is mainly a hill state with inhabited areas ranging from 600 to 4000 m MSL. It is one of the least urbanized States in India, and about 90% of its population resides in rural areas. The people residing in hills of this region traditionally have a distinct lifestyle consisting of high level of physical activity in the form of walking long distance, working manually, and consuming less processed high-fiber diet. However, in the last two decades, deeper and higher penetration of road network has made transportation easy with easy availability of highly processed packed food in remotest parts of the area. The present study was an endeavor to document changes in pattern of stroke in people residing at moderate altitude.
METHODS
This prospective, observational study was carried out in a Tertiary Care Hospital, situated at 2000 m MSL, from July 2014 to June 2015 in the Sub-Himalayan region of India. The clinical profile and outcome at 3 months of all patients admitted consecutively with stroke in medical wards were studied after obtaining informed consent from patient/attendant. Lipid Profile, ECG noncontrast computerized tomography head and echocardiography (when indicated) were relevant investigations done. The findings of the present study were compared with the study conducted 15 years back at our institute and changes in clinical profile were analyzed. The patients were contacted telephonically at 3 months for assessment of outcome.
Poor outcome was defined as modified Rankin Scale >3 (mRS) and Barthel Index <60 (BI) or death. The study was approved by the Hospital Ethics Committee.
mRS defines 6 different grades of disability, from 0 for “no symptoms at all” to 5 for “severe disability or bedridden, incontinent, and requiring constant nursing care and attention,” and Grade 6 for death. It has proved to be valid and reliable for defining outcome in stroke patients. Although the mRS was designed as a handicap scale, is now considered a disability scale as well.[7]
BI contains 10 items with varying weights that score the activities of daily living. The items bathing and grooming are scored 0 or 5; the items feeding, dressing, controlling bladder, controlling bowel, getting onto and off the toilet, and ascending and descending stairs are scored 0, 5, or 10. Items regarding moving from wheelchair to bed and walking on level surface are scored 0, 5, 10, or 15. The total BI is a cumulative score of the 10 items, with a maximum score of 100 corresponding with complete independence, and a minimum score of 0 corresponding with total dependence. It has also shown to be valid and reliable for assessing disability in stroke patients.[7]
RESULTS
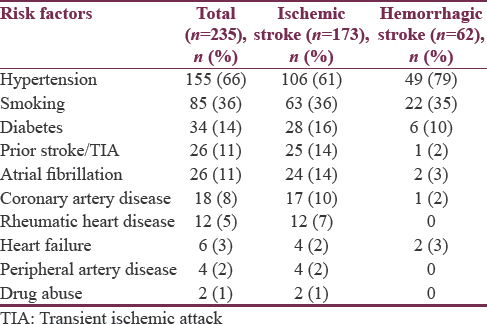
During the study, a total of 235 patients of stroke were admitted to medicine wards. Of these, 173 (74%) patients had ischemic stroke (IS), and 62 (26%) had hemorrhagic stroke (HS). Age group 61–70 years had highest (28%) number of patients. The various risk factors noted in patients are presented in Table 1. The details of clinical features are given in Table 2. The details of outcome of patients of stroke at 3 months are given in Table 3. During hospital stay, six patients (IS-4, HS-2) developed pneumonia and had poor outcome.


Stroke formed 0.7% of total admissions to hospital and 2.9% of total admissions to medicine wards during the study which was 0.9% and 3.3%, respectively, in the study conducted 15 years back. The types of stroke were similar in both studies (IS-74%, HS-26%). Male formed 58%, and 42% were female in the current study; however, it was 66% and 34%, respectively, in the previous study. Male-to- female ratio became 1.35:1 from 1.95:1 since the last study. The average age of patients was 62 years (M-60.3 years, F-64.7 years) as compared to 57.88 years (M-55.65 years, F-52.29 years) during the previous study. Stroke in elderly (>60 years) increased to 55% from 50% but stroke in young (<40 years) decreased to 8% from 12% since the last study.
Among risk factors, hypertension was present in 66% (IS-61%, HS-79%) patients than in 62% (IS-55%, HS-81%) in the previous study. The prevalence of smoking in patients of stroke decreased from 60% (IS-63%, HS-53%) to 36% (IS-36%, HS-35%). Diabetes Mellitus (14% vs. 8%), atrial fibrillation (11% vs. 6%), and Coronary artery disease (8% vs. 3%) increased since previous study. Past stroke/TIA (11% vs. 10%), rheumatic heart disease (5% vs. 6%), and peripheral arterial disease (2%) were comparable in both studies. In addition, heart failure and drug abuse were noted in the present study.
Poor outcome was determined at 3 months in terms of mRS >3 and BI <60. Out of total 235 patients, 203 could be contacted telephonically for the assessment of outcome. The details of factors associated with poor outcome in stroke are given in Table 4. Of total 62 patients of HS, 11 (18%) patients died during hospital stay, and mortality increased to 27 (55%) of total 49 patients available for follow-up at 3 months. Overall HS patients had poorer outcome at 3 months.

Of total 173 patients in IS group, 12 (7%) patients died during hospital stay; mortality rose to 36 (23%) out of 154 patients available for follow-up at 3 months. As the age advanced, outcome at 3 months worsened in both types of stroke by mRS and BI. In IS group, poor outcome was mRS-14%, BI-09% in 41–50 years age group, and it was mRS-75%, BI-69% in 81–90 years age group. Similarly, in HS, poor outcome was noted mRS-25%, BI-25% in 41–50 years age group and in 81–90 years group, it was mRS-100%, BI-100%.
Only 37 patients of IS presented <4.5 h of onset of symptom and 19 (51%) could be thrombolysed. Eighteen patients could be contacted, 6 patients had poor outcome, and 5 of them died. Four patients died in hospital and 1died during follow-up.
In our study, 23 (10%) patients of stroke died during hospital stay. In IS group, 12 patients died during hospital stay and total 36 (23%) died at 3 months follow-up. In HS 11 patients died in hospital and total 27 (55%) died at 3 months follow-up.
DISCUSSION
Of total 235 patients, 173 (74%) had IS and 62 (26%) had HS which is in unison with other studies.[89] Majority of the patients were males (57%), maximum (28%) patients were in 61–70 years age group. In a study by Siddique et al., stroke was found most commonly in 51–60 age groups and had male-to-female ratio 3:1 in HS and 1.35:1 in IS.[10]
Hypertension was the most common risk factor observed in our study in 66% of all patients of stroke and in 79% of patients of HS. This study correlated well with a study by Mahajan et al. in which hypertension was most common and most significant risk factor.[6] However, smoking, as a risk factor of stroke had decreased from 60% to 36% in our study. The consistent efforts of various agencies in our country for raising awareness regarding risks of smoking must have contributed to this. On comparing data of risk factors of our two studies, Diabetes mellitus and Coronary artery disease has increased which can be contributed to rising trends of both diseases in community. A multicentric, hospital-based case–control study revealed that diabetes mellitus, hypertension, tobacco use, and low hemoglobin, were the most important risk factors of IS.[11] In this study, 11% patients had past history of stroke/TIA. Hankey et al. reported the recurrent of stroke in 15% of patients of first-ever stroke over the next 5 years. The predictors of first recurrent stroke in their study were advanced age, hemorrhagic index stroke, and diabetes mellitus.[12] Of all 18 patients of stroke with CAD, 17 (94%) had IS and 6 (3%) patients of stroke had preexisting heart failure. Gilum observed in his study that the presence of prior heart disease as an established risk factor for stroke.[13]
In our study, in term of mRS, 79 patients had poor outcome and 32 (65%) of them were in HS group. In term of BI, 63 patients had poor outcome and 31 (63%) of them had HS. In this study, more patients with HS (55%) died than IS (23%) after 3 months follow-up. According to Hatano more patients with intracerebral hemorrhage had a fatal outcome and more than one-third of patients died on the day of the attack, irrespective of age, and 70%–80% died within a year. Cerebral ischemic necrosis showed the low fatality rate, beginning with only 4% and 5% on the 1st day, and reaching 20% and 45% at one year, in young and old patients, respectively.[2]
Patients with age >70 years had poor outcome in 62% (IS-55%, HS-91%) of patients with stroke. Michael and Shaughnessy reported age to be an independent predictor of outcome after IS. Older patients, especially those older than 80 years, are more likely to die in the hospital after stroke and less likely to make a favorable long-term recovery.[14] In IS group, poor outcome was noticed in 26 female patients (38%), whereas in HS group, both male and female patients, equally (65%) had poor outcome. In a study by Das et al., the rates of incidence and case fatality were especially higher among women perhaps because women outlive men (Census India, 2001) and exhibit higher prevalence of uncontrolled hypertension than men.[11] The altered sensorium (P = 0.00) and neurological weakness (P = 0.024) were significantly associated with poor outcome. The study by Mathews et al. is in agreement with the current study in which reduction of the level of consciousness to any degree and paralysis of conjugate gaze were adverse factors for outcome.[15] Jongbloed et al. have also reported less favorable functional outcome with more severe hemiparesis on admission.[16]
Association of hypertension, smoking, diabetes mellitus, coronary artery disease, and other risk factors with poor outcome by either mRS or BI as highlighted in Table 3. Willmont et al. concluded in a systematic review of 32 studies involving 10 892 patients that high blood pressure in acute IS or primary intracerebral hemorrhage was associated with subsequent death, death or dependency, and death or deterioration.[17] Michael and Shaughnessyconducted a study among patients who survived to 3 months poststroke. Older age, not being partnered, smoker, diabetics, history of a prior stroke, worse prestroke and poststroke functional status, greater stroke severity, and not being treated with thrombolytic were the predictors of worse functional status.[14]
CONCLUSION
There occurrence of stroke has decreased among hospitalized patients at moderate altitude. Hypertension, diabetes mellitus, and coronary artery disease increased but smoking decreased among patients of stroke. In current study, there was higher occurrence of IS but overall, HS had poor outcome. Age >70 years, female sex, altered sensorium, hypertension, diabetes mellitus, prior stroke, and smoking were observed as poor prognostic factors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We acknowledge the contribution of our teacher Prof. BS Prashar for his encouragement and guidance.
REFERENCES
- Stroke in India factsheet: Asia Network for Chronic Disease. Hyderabad: Public Health Foundation of India; 2012.
- Experience from a multicentre stroke register: A preliminary report. Bull World Health Organ. 1976;54:541-53.
- [Google Scholar]
- Early prognostic factors in ischemic stroke. The role of protein C and protein S. Stroke. 1993;24:1496-500.
- [Google Scholar]
- Ischaemic stroke in young adults: Predictors of outcome and recurrence. J Neurol Neurosurg Psychiatry. 2005;76:191-5.
- [Google Scholar]
- Long-term disability after first-ever stroke and related prognostic factors in the Perth community stroke study, 1989-1990. Stroke. 2002;33:1034-40.
- [Google Scholar]
- Optimizing cutoff scores for the Barthel index and the modified Rankin scale for defining outcome in acute stroke trials. Stroke. 2005;36:1984-7.
- [Google Scholar]
- The causes of stroke. In: Donaghy M, ed. Brains Diseases of Nervous System (10th ed). Oxford University Press Oxford; 1993. p. :216-29.
- [Google Scholar]
- Long-term risk of first recurrent stroke in the Perth community stroke study. Stroke. 1998;29:2491-500.
- [Google Scholar]
- Risk factors of stroke in blacks: A critical review. Am J Epidemiol. 1990;150:1266-74.
- [Google Scholar]
- Stroke prevention and management in older adults. J Cardiovasc Nurs. 2006;21:S21-6.
- [Google Scholar]
- High blood pressure in acute stroke and subsequent outcome: A systematic review. Hypertension. 2004;43:18-24.
- [Google Scholar]






