Translate this page into:
Clinical Features and Psychiatric Comorbidity of Epicrania Fugax
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Epicrania fugax (EF) is a rare newly described primary headache characterized by paroxysms of unilateral pain radiating across one hemicranium.
Aim:
We aimed to describe 10 new cases of EF and assess the psychiatric comorbidity.
Materials and Methods:
Cases of EF were identified from patients attending the neurology outpatient department of a tertiary level referral and teaching hospital by the first author during a period extending from January 1, 2015 to April 31, 2017. Case ascertainment was done as per ICHD 3 beta criteria from among patients presenting with complaints of headache after detailed history and clinical examination. Clinical and demographic features were noted and patients were subjected to Mini Neuropsychiatric Interview to screen for psychiatric comorbidity followed by Becks Anxiety/Depression Inventory.
Results:
A total of 10 subjects were obtained during the study period, 4 males, and 6 females. Mean age of subjects was 45.3 years (standard deviation-10). Seventy percent had anteroposterior, and 30% had posteroanterior radiation of pain. The most common character of pain was stabbing (50%) followed by electrical (40%) and pressing (10%). None of the subjects had autonomic symptoms or focal symptoms in the scalp while 30% subjects had hyperesthesia in the affected area of the scalp. Six subjects (60%) patients had episodic course while 40% had chronic course. Sixty percent had comorbid anxiety while one (10%) had comorbid depression. A significant relation was obtained between duration of disease and occurrence of anxiety as well as Becks Anxiety Inventory scores while there was no correlation with attack duration. There was also a nonsignificant correlation between visual analog score and occurrence of anxiety symptoms.
Conclusions:
Our study conclusively proves the existence of EF as a rare, distinct primary headache syndrome in our study population. It has a significant psychiatric comorbidity consisting of 60% of generalized anxiety disorder, 10% of panic attacks, and 10% of depression.
Keywords
Clinical feature
epicrania fugax
headache
INTRODUCTION
Epicrania fugax (EF) is a rare newly described primary headache first by Pareja et al. in 2008.[1] In 2013, EF was included in the Appendix of the International Classification of Headache Disorders, 3rd edition, beta version (ICHD-3 beta).[2] It is characterized by very brief (<10 s) paroxysms of unilateral pain spreading in a linear or zigzag direction across one hemicranium through the territories of different nerves. Early case descriptions emphasized a posteroanterior radiation, that is, from the posterior scalp toward the ipsilateral eye or nose. However, various variants have been described subsequently including those in which the radiation of pain is in an opposite anteroposterior direction,[3] multidirectional EF and EF involving both hemicranias,[4] EF with sagittal radiation of pain,[5] EF radiating upward from the lower part of face[6] as well as cases of EF secondary to other causes such as intracranial lesions.[7] The pain of EF is usually severe and electric shock like.[8] As might be expected from its rarity, data regarding the epidemiologic and clinical features as well as its psychiatric comorbidity is limited. It has not been described to the best of our knowledge in an Indian cohort.
Aims
-
To describe the clinical and epidemiological features of EF in an Indian cohort
-
To assess the psychiatric comorbidity of EF.
MATERIALS AND METHODS
Cases of EF were identified from patients attending the neurology outpatient department of a tertiary level referral and teaching hospital by the first author during a period extending from January 1, 2015 to April 31, 2017. Patients diagnosed to have EF were identified as per the criteria laid down in the ICHD 3 beta version. A detailed history regarding all aspects of the headache was taken. They included the exact site of origin, radiation and termination of pain, trajectory (linear or zigzag), duration of attacks as well as total duration of disease, whether chronic or remitting-relapsing, frequency of attacks, character and severity of pain, presence of interictal headache and presence of triggers for development for pain. Subjects were asked to chart the exact radiation of pain on a line drawing of the head and face and the intensity of pain was noted on the visual analog scale (VAS). The presence of any other type of headaches was carefully noted, and subjects with secondary headaches were excluded from the study. The ICHD 3 beta criteria were applied in the case of the other coexisting primary headaches to identify them as migraine, tension headaches, or others as appropriate. In addition, a history of other neurological as well as significant systemic diseases was taken. A detailed examination of the scalp was done in all subjects specifically looking for any areas of tenderness, trigger points, color changes, and vasomotor or sudomotor changes and temporal artery pulsation. Mini neuropsychiatric interview was completed by all subjects to identify psychiatric comorbidity followed by Becks Anxiety/Depression Inventory for further detailed evaluation as appropriate. Neuroimaging studies (magnetic resonance imaging) were done in all patients. Complete blood counts, erythrocyte sedimentation rate, standard biochemical tests, and a baseline vasculitic workup consisting of rheumatoid factor, antinuclear antibody and C-reactive protein were done.
RESULTS
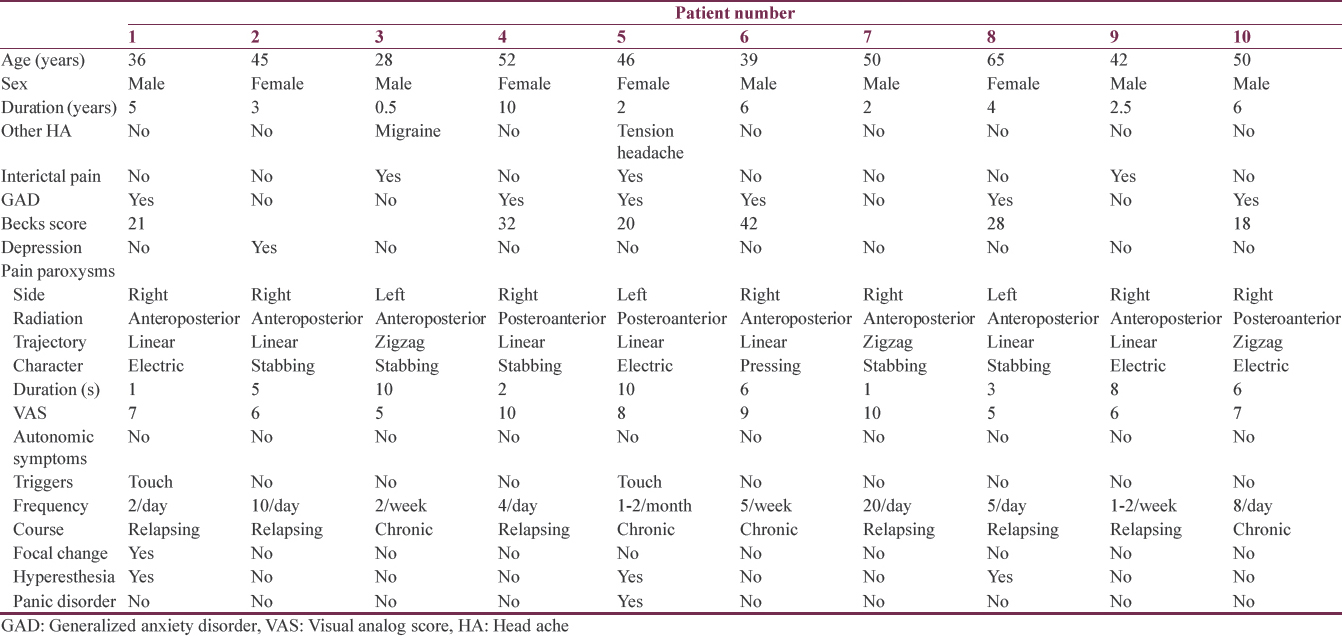
A total of ten subjects were obtained during the study period. Their clinical and demographic features are summarized in Table 1
Gender
The sample consisted of 4 male (40%) and 6 female (60%) subjects with no difference between gender and side of pain (χ2 = 0.2, P = 0.17). No Significant difference was noted between genders in regard to attack duration (χ2 = 0.14, P = 0.89). In the illness duration, there was also no significant difference between the sexes (χ2 = 0.53, P = 0.69). Male subjects had more left-sided pain whereas female had more incidence of right-sided pain which is having a significant difference (χ2 = 0.8, P = 0.04). Female subjects had more focal changes but not at a significant level (χ2 = 0.74, P = 0.3). Female subjects reported more hyperesthesia but again not significantly (χ2 = 1.27, P = 0.5). Males had more inter-ictal pain than females but no significant difference was noted (χ2 = 0.07, P = 1). Autonomic features did not occur in either sex. Male subjects had more chronic course than females (χ2 = 0.5, P = 0.4). In males, radiation of pain was more in the anteroposterior direction than posteroanterior while female subjects reported a similar frequency. Between the genders there was no difference in frequency of anxiety symptoms. In VAS pain scale, male subjects had higher pain scores than females but no there was no significant difference (t = 0.06, P = 0.9.)
Age
Mean (standard deviation [SD]) of the age of subjects at the time of presentation was 45.3.[9] The age of onset of disease in our cohort ranged from 27 to 61 years (mean 41.2; SD, SD = 9.04) Those subjects aged 50 years and above had more duration of illness than those < 50 years age; however, this was not statistically significant (χ2 = 0.09 P = 0.43). Those subjects < 50 years old had more attack duration than those above 50 years group (χ2 = 0.2, P = 0.03) On Beck's Anxiety Scale, those subjects aged more than 50 years have significantly higher occurrence of anxiety symptoms than those aged < 50 years group (t = 3 P = 0.01). Regarding VAS scores, there was no statistically significant difference between age and pain scores (t = 0.09, P = 0.9). Those aged < 50 years suffered more chronic type EF than relapsing-remitting EF whereas all subjects aged more than 50 years had a relapsing-remitting course. Those aged < 50 years had more right sided than left-sided EF while those more than 50 years had all left-sided EF. Focal changes in the scalp were very infrequent in the sample (only one subject). Similarly hyperesthesia was infrequent in the sample, occurring in 2 subjects aged below 50 years and one in a subject 65-year-old. There was no statistically significant difference in the occurrence of interictal pain or direction of radiation with age.
Duration of illness
Subjects with anxiety symptoms were found to have more duration of illness (P = 0.05). There was no significant correlation with between illness duration and attack duration. However, there was a significant positive correlation between duration of illness with Beck's anxiety scale scores, (Pearson coefficient = 0.72, P = 0.02). There was also a nonsignificant correlation between duration of illness and VAS scores (P = 0.15).
Attack duration
No difference in attack duration was noted between subjects with and without anxiety. A negative correlation between attack duration and occurrence of anxiety symptoms and VAS pain scores was obtained.
Anxiety score on BECK's scale (mean = 16.1, standard deviation = 15.44)
Presence of anxiety was positively correlated to higher VAS pain scores albeit not significantly (P = 0.5).
Direction of pain
No significant differences between the directions of radiation of pain with duration, attack durations, VAS, or Beck's anxiety score. Occurrence of anxiety was higher in those subjects with posteroanterior than anteroposterior radiation of pain (P = 0.37) whereas higher VAS pain scores occurred in subjects with posteroanterior radiation of pain (P = 0.13).
Frequency
Relapsing EF constituted 60% of cases whereas chronic cases were 40%. More attack duration was noted in chronic EF with significant difference as compared to relapsing EF (P = 0.02). Higher pain scores were noted in relapsing EF (P = 0.9) while more anxiety symptoms (P = 0.6) occurred in chronic EF subjects.
Side
Right-sided pain occurred in 70% cases whereas left-sided pain occurred in 30% cases. More anxiety symptoms (P = 0.6) and pain scores on VAS (P = 0.14) were noted in cases of the left-sided rather than right-sided pain; however, the difference was not significant.
DISCUSSION
The diagnostic criteria laid down for EF by The ICHD-3 beta, by the Headache Classification Committee of the International Headache Society[2] are as follows:
Description: Brief paroxysmal head pain, with stabbing quality, describing a linear or zigzag trajectory across the surface of one hemicranium.
Diagnostic criteria
-
Recurrent stabbing head pain attacks lasting 1–10 s, fulfilling criterion B
-
The pain is felt to move across the surface of one hemicranium in a linear or zigzag trajectory, commencing, and terminating in the territories of different nerves
-
Not better accounted for by another ICHD-3 diagnosis.
A total of 10 subjects were identified were identified during the study which constituted 0.96% of all primary headaches attending our neurology outpatient department during this period, thus making EF a truly rare primary headache syndrome in our study population. The possibility that many cases, especially the milder ones, do not show at a tertiary level center and are not picked up has to investigated in a population-based epidemiological study. Although epidemiological data are lacking EF made up 1.6% of the total number of patients attending a Spanish outpatient headache clinic during a 7 years period.[9] Cuadrado et al.[10] have summarized all the cases of EF (a total of 70) described in literature. In our study, males predominated over females in a ratio of 3:2 as opposed to the female preponderance of 1.7:1 reported by them. Similarly, the age of onset of our cohort ranged from 27 to 61 years (mean 41.2; SD, SD = 9.04) which is comparable the mean age of onset of 45.2 years (SD 17) reported by them. The majority of our subjects had no interictal pain, triggers for the pain paroxysms and did not exhibit focal changes or hyperesthesia over the scalp. None of the subjects had associated autonomic symptoms such as redness of eyes, tearing, or ptosis. The majority of subjects also had anteroposterior radiation of pain in a linear trajectory with a stabbing quality of pain and a relapsing-remitting rather than chronic course. Almost all patients had moderate-or-severe pain on VAS with duration of 1–10 s. The Mini International Neuropsychiatric Interview revealed six and one subjects to have generalized anxiety disorder (GAD) and depression, respectively. The mean score of the Becks Anxiety Inventory in the affected patients was 26.83 (SD: 9.13) while the Becks Depression Inventory score of the lone subject with depression was 19. One of the patients with GAD (patient no. 5) also had panic attacks. A few interesting facts emerge on analysis. Gender has no significant correlation with occurrence of anxiety. However, increased age of the patient (P = 0.01) as well as the duration of the illness (P = 0.05) had a positive correlation with the presence of anxiety. There was a nonsignificant correlation between the intensity of pain as shown on the VAS score and occurrence of GAD while no correlation between duration of individual headache attacks and anxiety could not be demonstrated. Similarly, the presence of anxiety was more in cases with posteroanterior radiation of pain (P = 0.37). Mean anxiety scores were more in subjects with a chronic course (P = 0.06) even though the mean VAS scores were more in the relapsing-remitting EF (P = 0.09). This raises the interesting question whether the high frequency of GAD in EF patients is secondary to the presence of a longstanding painful disorder or there is an inherent relation between EF and anxiety.
It is instructive to compare the prevalence of anxiety in other more common and better studied primary headaches like migraine. The prevalence of anxiety disorders in patients with migraine is 2–5 times higher than that compared to the general population.[9] Many population studies have demonstrated that various forms of anxiety disorders such as GAD, panic disorder, obsessive-compulsive disorder, and specific phobias are more common in migraineurs than the general population.[1112] One study has found that a patient with migraine has a 19% probability of comorbid anxiety, 7% of depression and 5% of both.[13] Other studies have found higher rates. For instance, Breslau et al.[14] found that in a random sample of young adults that those subjects with migraine were much more likely (50.7%–57.6%) to have anxiety disorders than those without migraine (27%). Regarding comorbid depression also, different studies have shown different rates from 8.6% to 47.9%.[15] The great importance of depression in migraine stems from its importance as a significant risk factor in the chronification of migraine, that is the conversion of episodic to chronic migraine.[16] Similarly, the other common type of primary headaches, tension type headaches, especially the chronic type of tension-type headaches have long been known to be associated with significant psychiatric comorbidity. Nearly half of these subjects have associated depression or anxiety disorder.[1718] Unfortunately, similar studies regarding psychiatric comorbidity in EF are lacking. However, in an interesting study, López-López et al.[19] attempted to analyze certain psychological features and their association with clinicodemographic characteristics in patients with EF by means of a case–control study and found that the case and control groups differed significantly from each other in denial, trait anxiety, and depression with EF patients scoring significantly from controls. No substantial differences were found in the stress, coping, and personality variables when a raw analysis of EF patients was done. However, in an in-depth analysis with control of paroxysm frequency, a very interesting and paradoxical finding emerged in that low-frequency EF patients scored significantly higher than controls in perceived stress, neuroticism, denial, self-blame, trait anxiety, and depression and higher than high-frequency EF in venting. The authors concluded that low-frequency EF patients seemed to have a distinctive psychological profile with poor coping strategies leading to stress and inadequate emotional adjustment and that were was a need to consider low-frequency EF patients as potential targets for psychological management in addition to medical management. This is comparable to the study conducted by Wacogne et al.,[20] who have found the intensity of stress and anxiety were higher in migraineurs as compared to a control group while depression scores remained low in both groups. Similar studies have found higher levels of stress in tension type headache.[21] The paradoxically higher frequency of perceived stress and poor coping skills in low-frequency EF as compared to higher frequency EF subjects favors the argument for an inherent relation between EF and anxiety.
The pathogenesis of EF is not definite, but it is probable that there is a peripheral generator of pain in the epicranium in view of the fixed, focal area of pain. After generation, pain irradiation may occur by peripheral (ephaptic transmission through different peripheral nerve fibres) or central (via the functional convergence of the trigeminal and cervical afferents in the central nervous system at the trigeminal nucleus caudalis) mechanisms.[102223] This raises the interesting possibility that anatomical and/or functional overlap between these neural pathways and those that mediate GAD, especially those in the brainstem could potentially explain the high correlation between EF and anxiety in our study. The most important impediment in the further study of the psychiatric comorbidity of EF is the paucity of patients. Studies with larger sample size of patients which are preferably population based as well as longitudinal studies which are necessary to enhance the statistical power and to accurately elucidate the influence of psychological factors on the course of EF. Regarding treatment, as no controlled trials are available no definite therapeutic recommendations are available. Due to possibility of spontaneous remission or low attack frequency in some patients preventive treatment is not required.[10] Medicines commonly found to be of use in several series of patients are antiepileptics such as gabapentin, lamotrigine, carbamazepine, pregabalin, and levetiracetam.[810] Amitriptyline, indomethacin, and greater occipital nerve blocks have been found to be useful in a few patients.[1810]
CONCLUSIONS
Our study has conclusively proved the existence of EF as a distinct rare primary headache syndrome in our population. It is a relatively homogenous entity, and the clinical profile of these patients conforms by and large to that described in international literature except for some aspects like a predominant anteroposterior rather than posteroanterior radiation of the pain. It has a high psychiatric comorbidity of 60% anxiety, 10% panic disorder, and 10% of depression. Only duration of disease was shown to have a statistically significant correlation with the occurrence of anxiety symptoms. Studies with larger number of patients, preferably population based and longitudinal are necessary to further define and elucidate the etiology and clinical correlations of psychiatric comorbidity of patients with EF.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Epicrania fugax: An ultrabrief paroxysmal epicranial pain. Cephalalgia. 2008;28:257-63.
- [Google Scholar]
- Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629-808.
- [Google Scholar]
- Epicrania fugax with backward radiation: Clinical characteristics of nine new cases. J Headache Pain. 2011;12:535-9.
- [Google Scholar]
- Facial pain radiating upwards: Could the pain of Epicrania fugax start in the lower face? Headache. 2015;55:690-5.
- [Google Scholar]
- Case report: Epicranial pain after radiotherapy for skull base meningioma – The first symptomatic Epicrania fugax? Cephalalgia. 2016;36:1389-91.
- [Google Scholar]
- Headache, depression and anxiety: Associations in the Eurolight project. J Headache Pain. 2016;17:59.
- [Google Scholar]
- Psychiatric comorbidities of episodic and chronic migraine. J Neurol. 2013;260:1960-9.
- [Google Scholar]
- Migraine, psychiatric disorders, and suicide attempts: An epidemiologic study of young adults. Psychiatry Res. 1991;37:11-23.
- [Google Scholar]
- Migraine and psychiatric comorbidity: A review of clinical findings. J Headache Pain. 2011;12:115-25.
- [Google Scholar]
- Psychosocial correlates and impact of chronic tension-type headaches. Headache. 2000;40:3-16.
- [Google Scholar]
- Depression and anxiety disorders associated with headache frequency. The nord-trøndelag health study. Eur J Neurol. 2003;10:147-52.
- [Google Scholar]
- Stress, coping, and personality in patients with Epicrania fugax, and their relation to the clinical characteristics of pain. Pain Med. 2017;18:152-60.
- [Google Scholar]
- Subjective stress and coping in recurrent tension-type headache. Headache. 1995;35:455-60.
- [Google Scholar]
- Structural relation of the trigeminal spinal tract to upper cervical roots and the solitary nucleus in the cat. Exp Neurol. 1961;4:134-48.
- [Google Scholar]
- Stimulation of the superior sagittal sinus increases metabolic activity and blood flow in certain regions of the brainstem and upper cervical spinal cord of the cat. Brain. 1991;114(Pt 2):1001-11.
- [Google Scholar]






