Translate this page into:
Predicting Prognosis of Psychosis in Huntington's Disease: Case Report and Review of Literature
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Huntington's disease (HD) is rare variant of progressive neurodegenerative disorder which follows an autosomal dominant pattern. Psychiatric comorbidities are not uncommon with HD. Mood disorder, cognitive disturbances, anxiety disorders, and psychosis are the psychiatric comorbidities reported with HD. We report here a case of HD, where psychosis developed during illness. Prognosis of psychosis in HD is emphasized in this report with review of literature.
Keywords
Huntington's disease
prognosis
psychosis
INTRODUCTION
Huntington's disease (HD) is a rare autosomal dominant disorder results from progressive neurodegeneration at basal ganglia due to the formation of abundant abnormal protein “Huntingtin.”[1] Expansion of the trinucleotide “CAG” repeat sequence (>35 repeats) on the short arm of chromosome 4, gives rise to the formation of protein “Huntingtin.”[1] The onset of HD usually occurs in the fourth to fifth decade of life and choreiform movement is the prominent manifestation, however as the disease advances cognitive impairment and psychiatric manifestations become evident.[1] Nearly, one-third to three-fourth of patients with HD has psychiatric manifestations.[23] Mood disorders, aggression, anxiety are the most common psychiatric manifestations and psychosis being relatively rare.[34] Psychiatric disorders often occur before the onset of motor symptoms of HD.[5] Psychotic symptoms often appear in the course of HD, after the motor symptoms develop and hence, in the early days, it was thought to be the forerunner of the HD.[3] Schizophrenia-like psychotic symptoms were also known to precede the onset of abnormal body movements of HD.[267] Psychotic symptoms may mask the motor symptoms or may delay the diagnosis of HD.
CASE REPORT
A 50-year-old, nondiabetic and nonhypertensive male was hospitalized in our psychiatric unit for his aggressive behavior, refusal for food and disturbed sleep. He also had delusions of control (people are controlling him by putting a computer chip in his brain) and persecution (neighbors were plotting plans to kill him by poisoning his food). Due to this, he was not going out of his house, keeping himself locked inside. These symptoms had started since 5 years but worsened over past 1 year. In the past 5 years, once he had consulted a psychiatrist for illness and received treatment (risperidone 6 mg/day and lorazepam 2 mg/day) for 2 months with little improvement in symptoms. Nonadherence to treatment subsequently further worsened his symptoms. Family members of the patient reported about abnormal body movements involving his extremities, trunk, neck as well as his orofacial musculature since past 8 years (i.e., 3 years before the onset of psychiatric symptoms). These movements were involuntary, bizzare and were of facial grimacing, hand twisting, tongue darting, and pelvic thrusting type in nature which was causing significant impairment in talking, eating, drinking, holding objects in hand as well as walking. His history was insignificant. Family history of the patient revealed similar movement disorder in his elder brother in his fourth decade of life, who subsequently developed psychotic features and absconded from home and was missing till date. Patient's father had died early at the age of 35 years in an accident, and by that time he did not have any movement disorder or any psychiatric illness. There was no history of substance abuse. No cognitive decline was reported and observed on evaluation.
General physical examination was normal. Neurological examination revealed choreiform movements involving his extremities as well as trunk. Other systemic examinations were within normal limits. His hematological investigations were within normal limits. Neuroimaging of the brain (computed tomography scan and magnetic resonance imaging) revealed diffuse cortical atrophy [Figure 1]. Genetic evaluation revealed 43 repeats of CAG in one allele of Huntingtin gene and 17 CAG repeats in the other allele. He was diagnosed with HD with organic delusional (schizophrenia-like) disorder (F06.2 as per International Classification of Diseases-10 diagnostic criteria). He was prescribed olanzapine (up to 20 mg/day) for schizophrenia. After opinion of neurologist, sodium valproate (600 mg/day) was started for the management of abnormal movements. Over a period of 4 weeks, the severity of psychotic symptoms and abnormal movements were reduced.
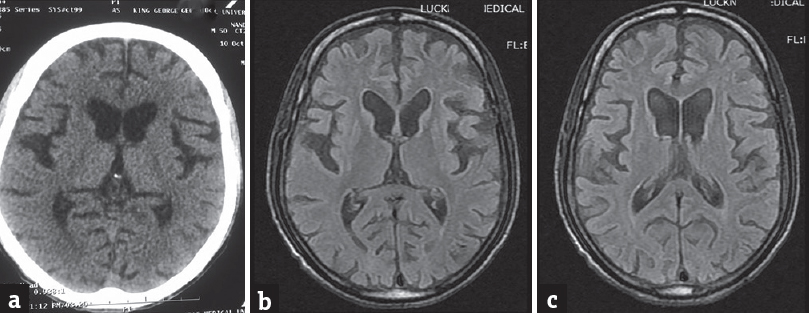
- (a) Computed tomography scan of brain showing cerebral atrophy and dilatation of the lateral ventricles; (b) magnetic resonance imaging of brain showing diffuse cerebral atrophy; (c) magnetic resonance imaging of brain showing dilatation of lateral ventricles resulting from cerebral atrophy. Atrophy of caudate nucleus is also evident (b and c)
DISCUSSION
Psychiatric manifestations are common in HD and can occur anytime in the course of illness (before as well as after the onset of motor symptoms).[3] The psychiatric symptoms evolve in the course of HD. Evidences suggest worsening of irritability, apathy, cognitive impairment as well as motor symptoms worsen with disease progression.[89]
Progressive neurodegeneration occurs in HD as well as in schizophrenia causing loss of brain volume. The presence of both the entities together is likely to hasten this process further. Hence, coexistence of both the entities may be considered as a poor prognostic factor for schizophrenia. In HD, there occurs loss of volume of gray matter, white matter, and expansion of the cerebrospinal fluid (CSF) spaces.[10] The presence of neurological signs and symptoms are also considered as poor prognostic indicator of schizophrenia.[11] Our patient had neurological signs and symptoms (movement disorder, ataxia, speech abnormality) along with radiological structural brain changes. The degree of mutation of CAG triplet has a correlation with the expansion of the CSF spaces,[10] hence can be considered as a prognostic indicator of schizophrenia also. However, another gene KCNN3 located in chromosome 1q21.3 also produces polymorphic CAG repeat sequences, is associated with better cognitive performance in schizophrenia.[12] Similarly, another earlier research concludes that degree of expansion of CAG repeats encoded by KCNN3 gene had a positive correlation with various symptoms of schizophrenia such as lack of energy, paranoia, and negative symptoms.[13]
Our patient had HD for past 8 years and psychosis for 5 years. Here, psychosis followed the motor symptoms of HD. The patient had significant cerebral atrophy, leading to dilatation of the ventricular system and cortical thinning [Figure 1]. In our patient, it can be a poor prognostic factor. CAG repeat sequence in one allele of Huntingtin gene was 43, which can be again a poor prognostic factor and have a positive correlation with the CSF space expansion (ventricular dilatation). The progressive neurodegeneration due to HD as well as schizophrenia can be double jeopardy in this case. Hence, the presence of HD may be considered as a poor prognostic indicator of psychosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Genetics and neuropathology of Huntington's disease. Int Rev Neurobiol. 2011;98:325-72.
- [Google Scholar]
- Psychosis, treatment emergent extrapyramidal events, and subsequent onset of Huntington's disease: A case report and review of the literature. Clin Psychopharmacol Neurosci. 2016;14:302-4.
- [Google Scholar]
- Psychopathology in verified Huntington's disease gene carriers. J Neuropsychiatry Clin Neurosci. 2007;19:441-8.
- [Google Scholar]
- Neuropsychiatric aspects of Huntington's disease. J Neurol Neurosurg Psychiatry. 2001;71:310-4.
- [Google Scholar]
- Cross-sectional study on prevalences of psychiatric disorders in mutation carriers of Huntington's disease compared with mutation-negative first-degree relatives. J Clin Psychiatry. 2008;69:1804-10.
- [Google Scholar]
- Schizophrenia-like psychotic symptoms in a patient with confirmed Huntington's disease: A case report. Psychiatr Pol. 2012;46:665-75.
- [Google Scholar]
- Huntington's disease in a patient with 15-year history of Capgras delusion misdiagnosed as paranoid schizophrenia. Gen Hosp Psychiatry. 2016;39:97-8.
- [Google Scholar]
- Longitudinal evaluation of neuropsychiatric symptoms in Huntington's disease. J Neuropsychiatry Clin Neurosci. 2012;24:53-60.
- [Google Scholar]
- How to target psychiatric symptoms of Huntington's disease: Clinical experience, limited evidence guide selection of symptom-focused treatments. Curr Psychiatry. 2012;11:34.
- [Google Scholar]
- Distinct brain volume changes correlating with clinical stage, disease progression rate, mutation size, and age at onset prediction as early biomarkers of brain atrophy in Huntington's disease. CNS Neurosci Ther. 2009;15:1-11.
- [Google Scholar]
- Kaplan and Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
- A CAG repeat polymorphism of KCNN3 predicts SK3 channel function and cognitive performance in schizophrenia. EMBO Mol Med. 2011;3:309-19.
- [Google Scholar]
- An association of CAG repeats at the KCNN3 locus with symptom dimensions of schizophrenia. Biol Psychiatry. 2002;51:788-94.
- [Google Scholar]






