Translate this page into:
Mood Disorder as an Early Presentation of Epidermoid of Quadrigeminal Cistern
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Intracranial epidermoids are space-occupying lesions of rare variant. Although cerebropontine angle and parasellar region are common sites of occurrence, it has been reported in various other parts of the intracranial cavity. Headache and features of increased intracranial tension are the common clinical manifestation. Report of psychiatric symptoms as the initial presentation of epidermoid is not known in literature except a single case report, which describes mutism to be the manifestation of intracranial epidermoid. We present here the case of a young male, who presented with long depressive episode persisting for 3 years with subsequent switch to mania, which persisted for more than 3 years. An episode of unconsciousness warranted neuroimaging, which revealed a large epidermoid of the quadrigeminal cistern. Surgical resection of the epidermoid was done. Persisting mood symptoms had responded to mood stabilizer and antipsychotic treatment.
Keywords
Epidermoid
mood disorder
quadrigeminal cistern
INTRODUCTION
Epidermoids are relatively rare variant of slow-growing, intracranial space-occupying lesions.[1] They constitute <2% of all brain tumors.[23] Commonly, these tumors are located at the parasellar or cerebellopontine angle region.[2]
They may arise from various sites in the cranial cavity, such as posterior fossa,[4] quadrigeminal cistern,[4567] brain stem,[238] temporal lobe,[910] and supratentorial dorsal cistern.[11] Patients with epidermoid cyst may present with features such as seizure, headache, nausea, and rarely with features of raised intracranial tension.[711] The clinical manifestation in intracranial epidermoid depends on the size as well as site of epidermoid. Epidermoids located at the cerebellopontine angle commonly manifest in the form of impairment of hearing and vertigo, whereas fourth ventricular involvement manifest with cerebellar signs and disturbance of gait.[12] Removal of the epidermoid is the treatment of choice. Complete surgical removal helps in maintaining the integrity of cerebrospinal fluid pathways.[7]
CASE REPORT
A 32-year-old gentleman was referred from the neurosurgery unit of a tertiary care hospital for psychiatric evaluation. The patient was apparently asymptomatic 6 years back. He had a history of gradual onset withdrawn behavior which was associated with low mood, decreased interest in work, and other pleasurable activities. He would lie down most of the time at home and would not go for work. He would report about lack of energy in the body leading to easy fatigability. He was shown to general physicians on multiple occasions, who prescribed him multivitamins and antioxidants. However, these symptoms persisted for 3 years with fluctuating severity. For the past 3 years, it was reported by the family members that he was talking more than usual. He would identify himself as the King of Ayodhya (an erstwhile kingdom in India). He would roam around here and there most of the times. There was increased cheerfulness and episodic anger outbursts. Increased sociability was also reported. His sleep was reduced to 2–4 h in a day. For the last 2 years, he had started consuming cannabis products daily in smoke form. Family members reported about sudden episode of unconsciousness 6 months back for which eventually led to his referral to us. There was no history of seizure or substance intoxication, immediately before the episode of unconsciousness. Before undergoing surgery, he was abstinent to cannabis; however, his mood symptoms persisted as before.
Investigation findings
Neuroimaging revealed an irregular large epidermoid occupying the quadrigeminal cistern with compression of the posterior 3rd ventricle and adjoining bilateral lateral ventricles [Figure 1]. The patient was operated through occipital transtentorial approach and near-total removal of the tumor was achieved. Histopathological examination of the excised specimen confirmed our preoperative diagnosis of epidermoid.
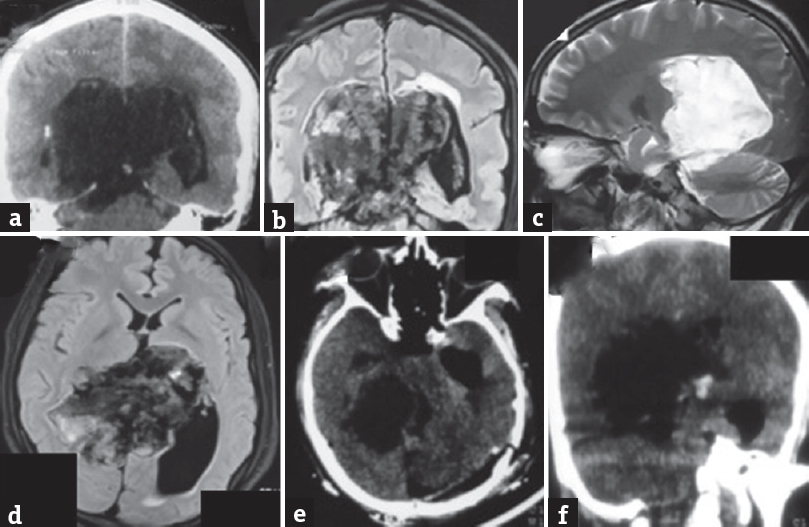
- Coronal reconstruction of cranial computed tomogram shows a hypodense large mass mainly located supratentorially with minimal infratentorial extension (a). The mass is compressing the posterior part of 3rd ventricle and bilateral lateral ventricles. The mass is heterogenous as seen on T2 flair image (b). The mass appears as predominant hyperintensity on T2 sagittal image (c). The mass was heterogenous with irregular borders on T2 flair (d) obliterating the body and atrium of the lateral ventricle on the right side with dilatation of the left occipital horn. Postoperative computed tomogram of the head showed a left occipital craniotomy defect with patent surgical cavity (e and f) and air inside the left temporal horn (e)
Postoperative period
His postoperative period was uneventful; however, there was persistence of psychiatric symptoms (irritability, grandiose talks, increased physical activity) despite near-total tumor excision; hence, he was referred to us for consultation (which was after 2 weeks following surgery). He was receiving prednisolone 10 mg/day, phenytoin 300 mg/day, and pantoprazole 40 mg/day.
Psychiatric evaluation and follow up management
On mental status examination, the patient had elated mood, delusion of grandiosity, increased flow of speech, and increased psychomotor activity. The patient had no insight for his behavioral changes. The psychiatric diagnosis of organic bipolar disorder was made. He was prescribed sodium valproate 1000 mg/day as mood stabilizer and olanzapine 10 mg/day. The dose of phenytoin was tapered and stopped over 2 weeks period. The patient was not receiving any psychotropic medication before surgery. The patient had shown improvement in his mood symptoms (baseline score of 34/60 on Young's Mania Rating Scale to 12/60 at the end of 8 weeks follow-up) with these treatments.
DISCUSSION
Our patient had presented with depressive features for 3 consecutive years followed by manic symptoms for 3 consecutive years without any interepisodic period of remission. His mood symptoms were persistent and pervasive. He had never received any psychiatric consultation till being referred from the neurosurgeon. Sudden unconsciousness warranted consultation from a tertiary care setup. Epidermoid of the quadrigeminal cistern was accidentally discovered during neuroimaging evaluation.
Mood (emotion) is regulated by various cortical as well as subcortical structures (frontal cortex, temporal cortex, amygdala, thalamus, hypothalamus, striatum, limbic system, and brain regions functionally connected to these important areas and cerebellum).[1314] The mood episodes in this patient were unique in their characteristics. They are persistent, pervasive, and prolonged (depressive symptoms for 3 years and manic symptoms for 3 years) without any interepisodic remission. In the natural course, depressive episodes are mostly short-lasting (mean duration of episode being 3 months) and more than 60% cases, the episodes last <6 months.[15] Similarly, in half of the cases with bipolar affective disorder, mood episodes last between 2 and 7 months.[16]
The neurobiology of switch of mood state in bipolar disorder is complex. Spontaneous switching may occur from the state of depression to mania in the presence of stress, sleep deprivation, substance use, and drugs or treatment modalities that alter mood state (electroconvulsive therapy, antidepressants, steroids, and stimulants).[17] In our patient, the switch of the mood state from depression to mania was not associated with any of the above factors. However, the slowly growing epidermoid might have a pivotal role in altering brain function to cause a switch in mood state.
Epidermoid, being a slow-growing tumor, did not result in any sudden neurological decompensation in this case. Epidermoid tumors, in general, have a tendency to creep into cisternal spaces without actually compressing the neural structures. It was evident in our patient that there was no gross alteration of the cortical architecture and neurological deficits for years despite the extensive size of the tumor as revealed on imaging.
In routine clinical practices, antiepileptic drug is prescribed following neurosurgical interventions for a variable period. In this regard, sodium valproate may be a good choice in patients who have prominent mood symptoms (manic type) due to its additional mood stabilizing property.
Clinical manifestations in intracranial epidermoid may be explained in two ways
-
Local effect (irritation of local structures, rarely local pressure effect)
-
Generalized effect (mainly due to chemical meningitis).
In our patient, the brain areas compressed due to mass effect were upper brainstem and limbic structures; however, hydrocephalic changes resulted in diffuse cortical thinning, which might have resulted in neuropsychiatric manifestations. Alterations in structural as well as functional integrity of the brain due to the tumor mass could not be restored back to normalcy in the postoperative period. It might be responsible for persistence of patient's symptoms warranting psychiatric intervention. This did not nullify the effect of the surgery and the clinical improvement during the follow-up period could be the cumulative effect of surgery and psychiatric intervention. There was a significant improvement in patients’ manic symptoms in 2 months follow-up.
Neuropsychiatric manifestations discussed in the context of epidermoid are cognitive impairment (dementia)[9] and mutism.[5] We did not find any description of mood disorder as the presentation or in association with epidermoids in literature. This is probably the first case report, where mood disorder (bipolar affective disorder) was possibly an early manifestation of epidermoid. However, a coincidental association of epidermoid with mood disorder could not be ruled out.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Intracranial midline dermoid and epidermoid cysts in children. Journal of Neurosurgery: Pediatrics. 2004;100:473-80.
- [Google Scholar]
- Intramedullary epidermoid cyst in the brain stem: Case report. Surg Neurol. 1996;45:537-40.
- [Google Scholar]
- Association of craniovertebral and upper cervical anomalies with dermoid and epidermoid cysts: Report of four cases. Neurosurgery. 2005;56:E1155.
- [Google Scholar]
- Epidermoid cyst in quadrigeminal cistern presenting with mutism. J Pediatr Neurosci. 2010;5:160-3.
- [Google Scholar]
- Epidermoid of the quadrigeminal cistern – Case report. Neurol Med Chir (Tokyo). 1990;30:59-62.
- [Google Scholar]
- Large epidermoids of the quadrigeminal cistern: An experience of 15 consecutive cases and review of literature. Acta Neurochir (Wien). 2012;154:1391-8.
- [Google Scholar]
- Intrinsic brainstem epidermoid cyst. Case report and review of the literature. J Neurosurg. 2006;104(4 Suppl):285-9.
- [Google Scholar]
- A case report of giant epidermoid in the temporal lobe: Considerations of the occurrence of intramedullary epidermoids. No Shinkei Geka. 1994;22:769-73.
- [Google Scholar]
- Intracerebral epidermoid tumor: A case report and review of the literature. Surg Neurol. 2001;55:218-22.
- [Google Scholar]
- Supratentorial dorsal cistern epidermoid cyst in childhood. Pediatr Neurosurg. 1998;29:203-7.
- [Google Scholar]
- Functional neuroanatomy of bipolar disorder: Structure, function, and connectivity in an amygdala-anterior paralimbic neural system. Bipolar Disord. 2012;14:340-55.
- [Google Scholar]
- Common and distinct neural correlates of emotional processing in Bipolar disorder and major depressive disorder: A voxel-based meta-analysis of functional magnetic resonance imaging studies. Eur Neuropsychopharmacol. 2012;22:100-13.
- [Google Scholar]
- Duration of major depressive episodes in the general population: Results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Br J Psychiatry. 2002;181:208-13.
- [Google Scholar]
- Is traumatic brain injury associated with reduced inter-hemispheric functional connectivity? A study of large-scale resting state networks following traumatic brain injury. J Neurotrauma. 2016;33:977-89.
- [Google Scholar]
- The neurobiology of the switch process in bipolar disorder: A review. J Clin Psychiatry. 2010;71:1488-501.
- [Google Scholar]






