Translate this page into:
Pulmonary Involvement in Patients with Guillain–Barré Syndrome in Subacute Phase
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
To evaluate the pulmonary function in Guillain–Barre syndrome (GBS) patients in subacute phase and find clinical correlates of pulmonary dysfunction.
Methods:
This was a single-center, prospective, cross-sectional, hospital-based study in GBS patients performed in Department of Neurological Rehabilitation at a tertiary care institute. Clinical examination for pulmonary function was done by measuring chest expansion. The pulmonary function tests were carried out by Spirometry kit Microquark Cosmed, Italy. Fatigue was assessed by Fatigue Severity Scale, disability status by Hughes Disability Scale (HDS), and muscle weakness by Medical Research Council sum scores.
Statistical Analysis:
Statistical analysis was performed by Stata 11. The significance of P value was adjudged against an alpha of 0.05.
Results:
Twenty-eight patients were included with 17 (61%) men and mean age of 31 years. Median duration of symptoms was 16.5 days. There were 10 (36%) demyelinating and 18 (64%) axonal variants. Twenty-six (93%) patients scored more than 2 on HDS. All study participants reported fatigue. Twenty-two (78.6%) patients had chest expansion of <2.5 cm. Spirometry showed restrictive pulmonary dysfunction in 23 (79%) patients. Significant correlation was found between abnormal pulmonary function test and chest expansion (P = 0.003).
Conclusion:
Pulmonary dysfunction in GBS is common even during subacute phase. It needs to be identified and managed appropriately for better clinical outcome.
Keywords
Fatigue
Guillain–Barre syndrome
pulmonary dysfunction
INTRODUCTION
Pulmonary involvement is present in Guillain–Barre syndrome (GBS), and approximately one-third of patients develop respiratory failure requiring mechanical ventilation.[1] GBS causes progressive respiratory muscle weakness involving both the inspiratory and the expiratory muscles. The weakness of the diaphragm is thought to be caused by phrenic nerve demyelination.[2] The classic signs of respiratory failure occur late, and the early manifestations consist only of tachypnea, tachycardia, air hunger, broken sentences, and a need to pause between sentences; later, use of the accessory respiratory muscles, paradoxical breathing, and orthopnea indicate severe diaphragmatic weakness.[3]
A number of studies have been done to show the prognosis and mortality in GBS patients requiring mechanical ventilation, but after a thorough literature search, we could not find any study to show the prevalence of respiratory involvement in subacute phase of the illness. We planned a study to evaluate the pulmonary function in GBS patients in subacute phase and find clinical correlates of pulmonary dysfunction.
METHODS
This was a single-center, prospective, cross-sectional, hospital-based study in GBS patients who attended the inpatient services of the Department of Neurological Rehabilitation of a tertiary care institute. The study was approved by the Institute Ethics Committee.
All consecutive patients diagnosed with GBS (satisfying National Institute of Neurological and Communicative Disorders and Stroke criteria), in the age group of 18–65 years, with duration of illness less than or 6 weeks, who had received treatment based on current guidelines, participated in the study. The patients with a history of chronic obstructive airway disease and patients on mechanical ventilation or tracheostomy were excluded from the study.
Information on age, gender, type of GBS based on the electrophysiological study, duration of illness at time of admission, history of antecedent factors, presence of respiratory distress, requirement of ventilator support, presence of pain, and paresthesias was recorded. A detailed clinical and neurological examination was done in all patients. Clinical examination for pulmonary function was done by measuring chest expansion in centimeters. In addition, Medical Research Council (MRC) sum-scores scale, Hughes Disability Scale (HDS), and Fatigue Severity Scale (FSS) were administered within 24 h of admission. The pulmonary function tests were carried out at Autonomic Laboratory of the Institute. All patients received regular rehabilitation program.
Spirometry test was performed using Spirometry kit Microquark Cosmed, Italy. The participants were explained about the procedure, and best of three measurements with interval of 2 min between the tests was used for analysis. The percentage predicted values of forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), the peak expiratory flow rate (PEFR) and maximum voluntary ventilation (MVV), inspiratory reserve volume, and the ratio of actual values of FVC/FEV1 (%) and FEV1/PEFR were considered for analysis. The actual values of maximum expiratory pressure and maximum inspiratory pressure were expressed as absolute value in cm of H2O measured by fabricated digital peak pressure monitor, designed on Black and Hyatt principle (Black LF et al., 1969). Predicted values were calculated by kit Spiro instrument's software according to Europe reference mode using Knudson for flow-volume curve (Knudson RJ et al., 1983) and Lindall (Lindall A et al., 1967) and Kory for MVV (Kory RC, 1961).
Other study tools were included as follows:
Medical research council scale
The MRC sum-score is a summation of the MRC grades (range, 0–5) given in full numbers of the following muscle pairs: Upper arm abductors, elbow flexors, wrist extensors, hip flexors, knee extensors, and ankle dorsiflexors. The MRC sum-score ranges from 0 (total paralysis) to 60 (normal strength). Good validity and interobserver reliability for this scale have been demonstrated in patients with GBS.[4]
Hughes disability scale
Hughes et al. in his study used a scale for the assessment of outcome in GBS patients.[5] It focuses mainly on walking. It ranges from Grade 0 to Grade 6 (Grade 0 = healthy; Grade 1 = minor signs or symptoms of neuropathy but capable of manual work; Grade 2 = able to walk without support of a stick but incapable of manual work; Grade 3 = able to walk with a stick, appliance, or support; Grade 4 = confined to bed or chair bound; Grade 5 = requiring assisted ventilation; and Grade 6 = dead).
Fatigue severity scale
It is a unidimensional fatigue scale frequently used in neuromuscular disorders. It measures fatigue by assessing the consequences of fatigue on daily functioning. It is a self-report questionnaire, easy to use in clinical practice, as the nine items of the test can be answered within <5 min. A mean score on these statements ranges from 1 (no signs of fatigue) to 7 (most disabling fatigue). An average score of 4 and higher is indicative for fatigue and a score of 5 and higher for severe fatigue. This questionnaire has been applied to patients with GBS and shown to be most appropriate for evaluating fatigue.[67]
Statistical analysis
Statistical analysis of data was performed by Stata 11 (StataCorp. 2009, College Station, TX, USA). Cross tables were analyzed using Pearson Chi-square test or Fisher's exact probability test. Continuous variables were compared (across two categories) using independent samples t-test. The significance of P value was adjudged against an alpha of 0.05.
In this study, we did a comparison between two groups that is those with normal pulmonary function tests and those with abnormal pulmonary function tests. For continuous variables, we applied independent samples t-test. For categorical variables, we applied Chi-squar test of independence.
RESULTS
A total of 28 patients satisfied inclusion criteria in the study period. The mean age was 31 ± 11.87 years (range - 18–51 years) and there were 17 (61%) men. The median duration of symptoms at the time of admission in neurological rehabilitation was 16.5 days (range - 10–42 days) and the median duration at the time of test was 27.5 days (range - 14–45 days). Among the clinical subtypes, there were 10 (36%) demyelinating and 18 (64%) axonal variants.
Historically, antecedent events were observed in 17 (60%) patients. Respiratory distress was present in 4 (14%) cases and all of them required ventilator assistance. Facial palsy was seen in five (18%) patients and bulbar symptoms in the form of drooling in four (14%), dysphagia in nine (32%), dysphonia in nine (32%), and need for nasogastric tube in seven (25%) patients. Sensory symptoms were prevalent in the form of neuropathic pain in 14 (50%) and paresthesias in 24 (86%) patients. Bladder symptoms were present in five (18%) patients and 3 (11%) patients had newly diagnosed hypertension. Based on body mass index, patients were categorized into underweight (<18.5), normal (18.5–24.9), overweight (25–29.9), and obese (30 or greater).
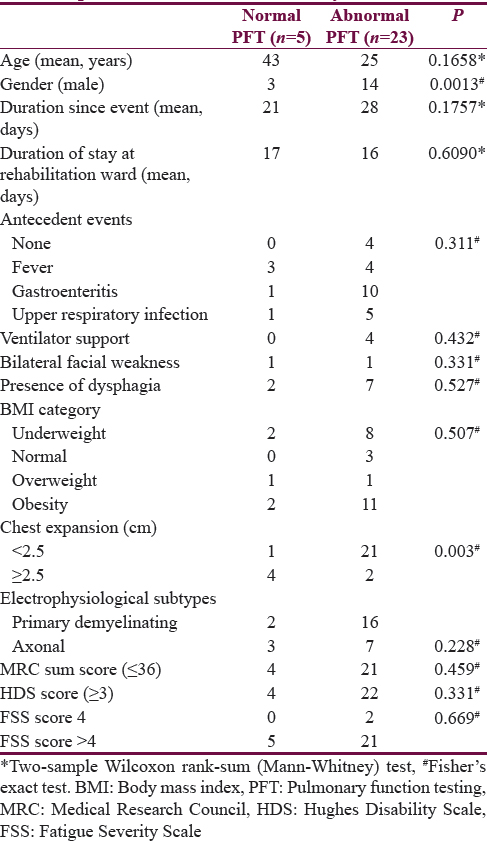
Twenty-six (93%) patients scored more than 2 on HDS. All the study participants reported fatigue (FSS score 4 and more). Twenty-six (93%) patients had severe fatigue (FSS score of 5 and higher). This is important to note that none of our patients had any underlying causes of fatigue such as severe anemia, hypothyroidism or uncontrolled/untreated diabetes, or any chronic illness, which could be contributing to fatigue in our patients. On clinical examination, 22 (78.6%) patients had chest expansion of <2.5 cm. There were no other clinical diffeferences noted between the two groups, normal and abnormal, which could serve as an indicator of impaired lung function. Spirometry showed pulmonary dysfunction (restrictive type) in 23 (79%) patients. Among patients with restrictive abnormality, 2 (7%) had mild, 5 (17%) had moderate, 3 (10%) had moderately severe, and 13 (45%) had severe restrictive abnormality. Table 1 summarizes the clinical correlates of pulmonary involvement in study patients. Significant correlation was found between abnormal pulmonary function test and chest expansion (P = 0.003).
DISCUSSION
This study was carried out to evaluate pulmonary function both clinically and objectively in GBS patients during subacute phase and to find its clinical correlates. The median duration of illness at the time of test was 27.5 days suggesting subacute phase.
All of the studies on respiratory involvement in GBS have reported respiratory insufficiency during the acute phase of the disease. Our study reports the presence of significant respiratory insufficiency both clinically and qualitatively during the subacute phase of GBS. Spirometry showed restrictive pulmonary dysfunction in 23 (79%) patients. Thus, there is a need to monitor these patients for pulmonary involvement during the subacute phase and manage the complications arising due to pulmonary dysfunction.
All our study patients reported fatigue and 93% had severe fatigue, in contrast to study by Garssen et al. where authors observed severe fatigue in 60% of all GBS patients.[8] Ranjani et al. have reported that the presence of fatigue was associated with ventilator requirement (P = 0.021) implying that fatigue was more prevalent in severe form of disease.[9] Even though the majority of patients in our study were severely fatigued, we did not find any significant association between FSS scores and pulmonary dysfunction in our study. This could be due to small sample size.
Pulmonary involvement was not significantly different between the acute inflammatory demyelinating polyneuropathy and acute motor axonal neuropathy group similar to study by Kalita et al. where 100 of 328 study patients had respiratory involvement and 13.1% patients required ventilator support.[10] The risk of respiratory involvement is higher in patients with demyelinating subtype in some studies.[1112] Our study participants consisted primarily axonal subtype (n = 18) as compared to demyelinating type (n = 10). Our results showed respiratory dysfunction in a majority of the patients (79%) in contrast to previous studies though there was no significant difference between the demyelinating and axonal subtypes.
Walgaard et al. studied 397 GBS patients to predict the chance of respiratory insufficiency and need for mechanical ventilation in the acute stage of the disease and concluded that days between onset of weakness and admission, MRC sum score, and presence of facial, and/or bulbar weakness were the main predictors of mechanical ventilation.[13]
Various other studies have identified risk factors for respiratory insufficiency in GBS including cranial nerve deficits,[111415] disability grade on admission,[1116] rapid progressive motor weakness,[14] areflexia,[16] descending weakness,[17] dysautonomia,[14] and electromyographic features of nerve conduction block.[1112] Our study results reported no significant association of pulmonary dysfunction with any of these factors during subacute stage of GBS. However, none of these studies have reported a correlation between simple bedside clinical tests such as chest expansion and pulmonary dysfunction. We recorded chest expansion of all study patients and found that out of 22 individuals who had chest expansion <2.5 cm, 21 (95.4%) individuals had restrictive abnormality on spirometry. Thus, we would emphasize on bedside examination mainly chest expansion, as it is indicative of respiratory insufficiency. It should be performed meticulously in GBS patients even during the subacute stage.
Respiratory dysfunction in GBS patients in rehabilitation setting can lead to complications including chronic obstructive pulmonary disease, restrictive respiratory disease, and respiratory muscle insufficiency.[18] Physical therapy measures (chest percussion, breathing exercises, and resistive inspiratory training) may be required to clear respiratory secretions to reduce work of breathing.[1920] However, one must be careful not to overfatigue the muscles of respiration during the initial period of motor unit recovery because this may push the patient into respiratory failure.[20] The rehabilitation measures provided in our patients with pulmonary dysfunction included physical therapy measures such as chest percussion and breathing exercises. All patients were made to practice respiratory muscle exercises with spirometer as well.
Limitation of the study
The study had small sample size and there was no follow-up, so resolution of pulmonary dysfunction could not be determined.
CONCLUSION
The study suggests that pulmonary dysfunction in GBS is common even during subacute phase. It should be monitored by simple bedside clinical examination, quantified by respiratory function tests, and managed appropriately.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Long term ventilation in neurogenic respiratory failure. J Neurol Neurosurg Psychiatry. 2003;74(Suppl 3):iii24-30.
- [Google Scholar]
- Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndrome. Muscle Nerve. 1991;14:1103-9.
- [Google Scholar]
- Connecting impairment, disability, and handicap in immune mediated polyneuropathies. J Neurol Neurosurg Psychiatry. 2003;74:99-104.
- [Google Scholar]
- Amantadine for treatment of fatigue in Guillain-Barre syndrome: A randomised, double blind, placebo controlled, crossover trial. J Neurol Neurosurg Psychiatry. 2006;77:61-5.
- [Google Scholar]
- Residual fatigue is independent of antecedent events and disease severity in Guillain-Barré syndrome. J Neurol. 2006;253:1143-6.
- [Google Scholar]
- Prevalence of fatigue in Guillain-Barre Syndrome in neurological rehabilitation setting. Ann Indian Acad Neurol. 2014;17:331-5.
- [Google Scholar]
- Guillain-Barré syndrome: Subtypes and predictors of outcome from India. J Peripher Nerv Syst. 2014;19:36-43.
- [Google Scholar]
- Clinical and electrophysiological predictors of respiratory failure in Guillain-Barré syndrome: A prospective study. Lancet Neurol. 2006;5:1021-8.
- [Google Scholar]
- Electrophysiology to predict mechanical ventilation in Guillain-Barré syndrome. Eur J Neurol. 2003;10:39-44.
- [Google Scholar]
- Prediction of respiratory insufficiency in Guillain-Barré syndrome. Ann Neurol. 2010;67:781-7.
- [Google Scholar]
- Anticipating mechanical ventilation in Guillain-Barré syndrome. Arch Neurol. 2001;58:893-8.
- [Google Scholar]
- Tongue weakness is associated with respiratory failure in patients with severe Guillain-Barré syndrome. Acta Neurol Scand. 2009;119:364-70.
- [Google Scholar]
- Predictive factors and long-term outcome of respiratory failure after Guillain-Barré syndrome. Am J Med Sci. 2004;327:336-40.
- [Google Scholar]
- Clinical predictors of mechanical ventilation in Fisher/Guillain-Barré overlap syndrome. J Neurol Neurosurg Psychiatry. 2009;80:60-4.
- [Google Scholar]
- Guillain-Barre´ Syndrome. New York: Thieme Medical Publishers; 1993.
- Guillain-Barre´ Syndrome: An update in rehabilitation. Int J Ther Rehabil. 2009;16:451-60.
- [Google Scholar]






