Translate this page into:
Corneomandibular reflex: Anatomical basis
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Corneomandibular reflex is a pathological phenomenon evident in cases of severe brainstem damage. It is considered to be a pathological exteroceptive reflex, associated with precentro bulbar tract lesions. The sign is useful in distinguishing central neurological injuries to metabolic disorders in acutely comatose patients, localizing lesions to the upper brainstem area, determining the depth of coma and its evolution, providing evidence of uncal or transtentorial herniation in acute cerebral hemisphere lesions, and it is a marker of supraspinal level impairment in amyotrophic lateral sclerosis and multiple sclerosis. This sign was evident in a patient with severe brain damage. We discuss the literature findings and its relevance in prognosis establishment.
Keywords
Brainstem damage
bulbar tract lesion
corneomandibular reflex
Introduction
The corneomandibular reflex, also known as Wartenberg reflex, consists in the contralateral deviation of the jaw, after corneal stimulation. The early description dates from the early 1900s, and it has been found and described in different severe encephalic diseases.[1] It is probably an expression of severe supranuclear impairment or rostral brainstem dysfunction (Gordon Wartenberg). This clinical sign is extremely rare, and the pathophysiological basis is still unclear. Herein, we describe a clinical case we observed, with etiopathogenetic considerations together with literature revision.
Case Report
A patient aged 62 years reported multiple injuries following serious motorcycle accident. In the emergency department, he arrived awake, with evidence of severe abdominal and chest trauma, pelvic and legs fracture. He underwent immediate surgery, for the correction of orthopedic and abdominal trauma. Few hours later, he entered in a deep coma status (Glasgow Coma Scale 3). Neurological examination showed absence of any voluntary motor and sensorial activity, absence of plantar responses. Pupils were reactive and corneal reflexes present. We observed bilateral prominent corneomandibular reflex with contralateral jaw deviation on both sides after immediate stimulus of the corneal surface with a simple cotton swab, lasting 1–2 s.
Brain computed tomography scan demonstrated severe diffused cerebral edema. Upper limb somatosensory evoked potentials showed the bilateral absence of cortical evoked components (N20). Electroencephalography revealed background activity of 4–5 Hz with voltage diffusely and significantly reduced, interposed with rare monomorphic delta activity at 1–2 Hz. Intracranial pressing (ICP) >28 mmHg (normal values 7–15). The patient died a few days later.
Discussion
The corneomandibular reflex is a pathological phenomenon evident in cases of severe encephalopathy.[1] It is usually bilateral, sometimes more prominent on one side, usually associated with severe neurological abnormalities, typically motor, associated with severe depression of consciousness. It was first described in 1902 by Von Solder, who interpreted it as a physiological reflex, more expressed and visible under certain conditions.[2] Subsequently, Tromner described this sign in 1918, unaware of Von Solder observations. He stated it was evident only in pathological conditions. Tromner felt the origin of this sign secondary to suprabulbar lesions.[3] Wartenberg in 1948 characterized the phenomenon of jaw deviation associated forced contralateral eye closure, following corneal stimulation. Lesion of the supranuclear trigeminal tract was suspected which consequent associated movement of the orbicularis muscle oculi and external pterygoid muscles (Gordon). In amyotrophic lateral sclerosis (ALS), a bilateral response was evident, possible impairment of rostral pontine fibers.[4] Guiot in 1946 specified that this sign was not evident in healthy subjects, or in simple elderly and in sleep condition, but rather in patients with severe brainstem lesions. This phenomenon appeared to be related to the level and severity of the injury and to the depth of unconsciousness, most frequently in acute severe head trauma.[5] He also mentioned, without describing a patient with the comatose state following a tumor of the pineal region. Subsequently, histopathological characterizations, determined that the corneomandibular reflex is an expression of brainstem dysfunction, and in the presence of supratentorial disease, this sign is an indicator of transtentorial herniation.[1] Neurophysiological studies established that this reflex is considered to be a pathological exteroceptive reflex; an association with precentro bulbar tract lesions was also reported.[6] Large cerebral hemispheric lesions with secondary brainstem pressure, intrinsic lesions of the upper brainstem (often accompanied by raised ICP), and involvement of corticobulbar pathways in ALS or multiple sclerosis (MS) were the most common settings where the reflex occurred. This sign provided evidence of uncal or transtentorial herniation in acute cerebral hemisphere lesions, suggesting the supraspinal level impairment in cases of ALS and MS. It is also useful in distinguishing structural from metabolic processes.[7]
To be properly elicited, it is required a firmus stimulus of the cornea. It is often associated with the normal corneal reflex with bilateral blink. The jaw movement is primarily related to the blink rather than the corneal stimulus, but corneal stimulation may be necessary to overcome a higher threshold for expression of the synkinesia,[8] and this represents a further evidence that pons neural pathways are crucial in determining this reflex. It can be rarely observed in patients with other neurological diseases, without consciousness impairment, as ALS. This abnormal sign must be unequivocal and prominent. It is more common than we think, because it is rarely sought and recognized. However, when clearly presented, it provides evidence of severe structural supranuclear pathways damage and or brainstem dysfunction.
The afferent limb of the corneal reflex travels in the ophthalmic division of the trigeminal nerve from light touch receptors in the conjunctiva and cornea. Back through the superior orbital fissure and trigeminal ganglion, the nerve fibers then pass to the main sensory nucleus of the trigeminal nerve.[9] From here, the efferent pathway passes via interneurons to the motor nuclei of the facial nerve, causing closure of the eyelids on triggering of the reflex. In detail, inside the mesencephalic trigeminal nucleus, the presence of an inhibitory interneuron, located close to the ipsilateral motor nucleus of V cranial nerve, is determined, preventing further massive activation of trigeminal motor neurons. In presence of a cortico-pontine boundaries lesions, or less probably, intra brainstem pathology, this inhibitory influence disappear, so activation of the entire trigeminal motor neurons elicited by corneal stimulation, is possible, resulting in a contraction of the masseter of both sides, realizing the cornea mandibular reflex.[101112] In our experience, the presence of normal corneal and photomotor reflexes, together with the increased ICP and the absence of somatosensory evoked potentials, mostly suggests the failure of supranuclear inhibitory pathways, as possible origin of this sign [Figure 1]. Hereafter we would like to remind the meaning of always looking for all the clinical signs, even if uncommon, since their presence or absence, could allow better characterization of the possible neurophysiological impairment, particularly in critical patients, where is difficult perform prolonged neuroradiological imaging, especially if an active cooperation is required.
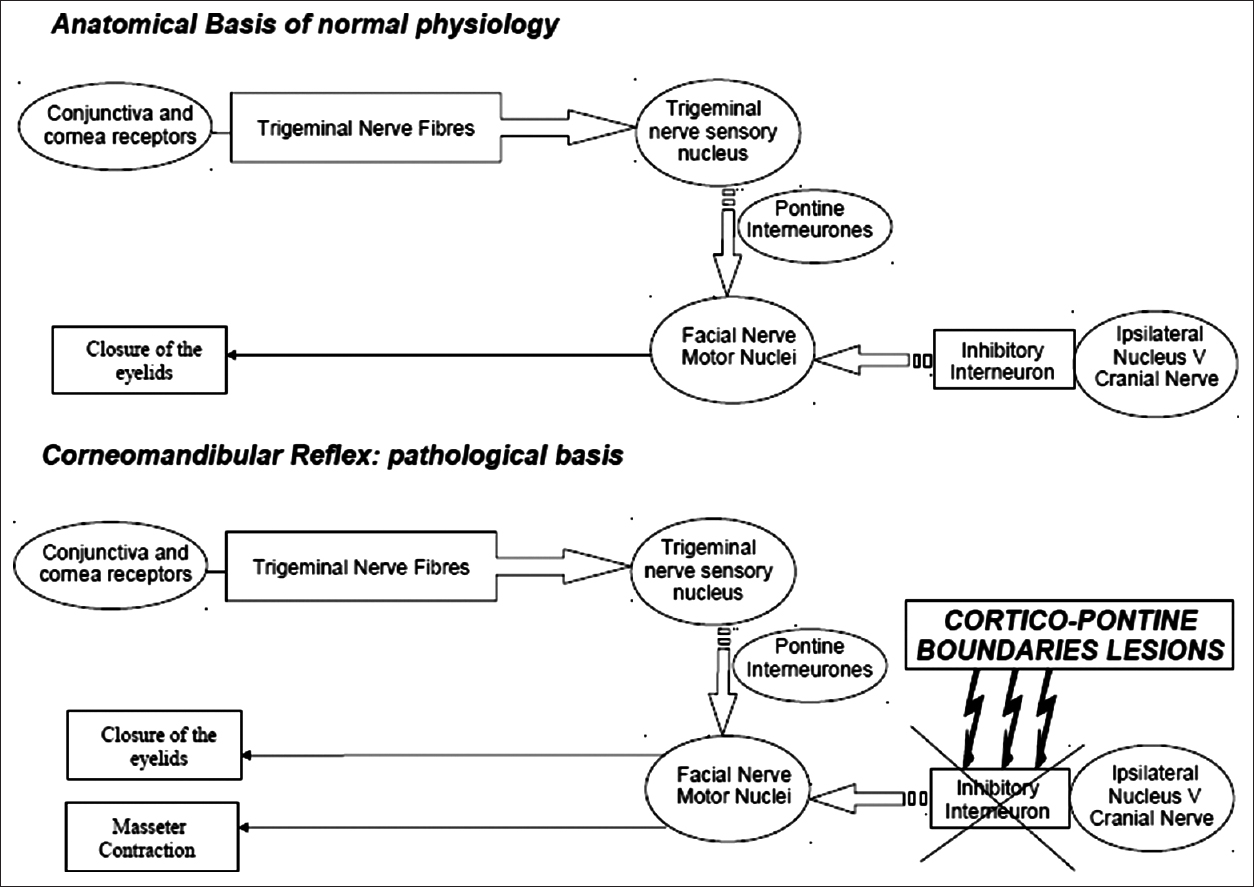
- Corneomandibular reflex: Physiology and pathology
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
References
- The horny-pterygoid reflex. The phenomenon of lateral excursion of the lens maillaire. Rev Neurol. 1946;78:48-9.
- [Google Scholar]
- The recorded corneo-mandibular reflex. Electroencephalogr Clin Neurophysiol. 1986;63:25-31.
- [Google Scholar]
- Spontaneous palpebromandibular synkinesia: A localizing clinical sign. Ann Neurol. 1994;35:222-8.
- [Google Scholar]
- The trigeminal mesencephalic nucleus. II. Electron microscopy. Am J Anat. 1970;127:303-19.
- [Google Scholar]
- Neurophysiological assessment of trigeminal nerve reflexes in disorders of central and peripheral nervous system. Clin Neurophysiol. 2005;116:2255-65.
- [Google Scholar]
- The role of trigeminal interpolaris-caudalis transition zone in persistent orofacial pain. Int Rev Neurobiol. 2011;97:207-25.
- [Google Scholar]
- Brainstem reflexes: Electrodiagnostic techniques, physiology, normative data, and clinical applications. Muscle Nerve. 2002;26:14-30.
- [Google Scholar]






