Translate this page into:
Elevated antimeasles antibody titre: An association in autoimmune encephalitis
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Autoimmune encephalitis is a group of treatable noninfective encephalitic disorders with great clinical implications. They have a close resemblance to prion disease and some slow virus infections. We report the presence of significant titers of antimeasles antibody in some of our patients with autoimmune encephalitis resulting in diagnostic and therapeutic problems.
Patients and Methods:
Patients seen by us in the last 4 years with high titers (1:625 dilution) cerebrospinal fiuid (CSF) antimeasles antibody positivity were reviewed retrospectively. The data collected were assessed using SPSS- Statistical Package for Social Sciences Version 15.0 (IBM corporation) software. The groups which showed elevated antimeasles antibody titers but did not have other parameters suggestive of subacute sclerosing panencephalitis (Group 2) were segregated and compared with those who had the typical features (Group 1) using Fisher's Exact Test.
Results:
There were 33 patients with antimeasles antibody in CSF. Group 1 had 27 and Group 2 had 6 patients. Group 1 had lower age, cognitive dysfunction, slow myoclonus, less generalized tonic-clonic seizures, and focal seizures. Group 2 patients belonged to the higher age, had significant psychosis (P = 0.02), incontinence of bowel and bladder (P = 0.0001). Slow myoclonus was significant in the first group (P = 0.028), and weakness was significant in the second group (P = 0.028) and double incontinence in the second group (P = 0.0001). Magnetic resonance imaging showed significant gray matter and cerebellar involvement in Group 2 P = 0.005 and P = 0.028, respectively.
Conclusions:
Patients who show significant titers of antimeasles antibodies in the CSF but belonging to older age group with psychosis, generalized tonic-clonic seizures, double incontinence, focal myoclonus, and electroencephalographic and imaging noncorroborative need to be investigated for autoimmune encephalitis in view of the great prognostic and therapeutic relevance.
Keywords
Antimeasles antibody
autoimmune encephalitis
subacute sclerosing panencephalitis
Introduction
Autoimmune encephalitis is a group of treatable noninfective encephalitic disorders with great clinical implications. They share clinical, radiological, and immunological features with a spectrum of disorders and diagnosis depends on careful integration of clinical, and laboratory features. Limbic encephalitis was first described in the year 1960 as both paraneoplastic and also as a de novo entity.[1] They are of several types with well-characterized oligoclonal antibodies in paraneoplastic disorders and voltage-gated potassium channel (VGKC), N-methyl-D-aspartate (NMDA), glutamic acid decarboxylase (GAD) antibodies in nonparaneoplastic conditions.[23] Patients often present with limbic symptoms like depression, panic disorder, anxiety, confusion, psychosis, poor concentration, memory problems, etc. They can, in addition, have a variety of other features like myoclonic jerks, seizures, transient ischemic attacks, and strokes.[3] Thus, they mimic a variety of common problems. Imaging can be normal or show subtle changes in limbic areas. Corsellis et al. described the syndrome in a case of bronchogenic carcinoma.[4] Diagnostic criteria for paraneoplastic limbic encephalitis was laid by Gultekin et al. which includes: (1) Pathology demonstrating limbic inflammation (2) all of the following: (a) Short-term memory, psychiatric problems and seizures. (b) <4 years between diagnosis of malignancy and the syndrome. (c) Response to immunomodulation and removal of the tumor. (d) At least one of the following. (a) Cerebrospinal fiuid (CSF) showing inflammation. (b) Temporal lobe changes in magnetic resonance imaging (MRI). (c) Changes in electroencephalographic (EEG).[3]
In this paper, we report the presence of significant titers of antimeasles antibody in some of our patients with autoimmune encephalitis resulting in diagnostic and therapeutic problems.
Antigens, antibody, and their importance
Antigens are antibody generators and are recognized by antigen receptors - B-cell receptors or T-cell receptors. Antigens can be exogenous, endogenous, tumor antigens or self-antigens. They are proteins, polysaccharides or lipids and joining with an adjunct produce immune response. Antigen specificity is the ability of the host to recognize the antigen as a unique molecular entity and distinguish it with precision. Antibodies are immunoglobulins belonging to the family of glycoproteins. They neutralize foreign antigens by locking to a specific epitope of the antigen. Memory B-cells remain in the body, remember the antigen and act faster on re-exposure. A small region at the tip of proteins if variable allows for millions of antibodies with slight differences in structure.[5] Elevated titer of antibody against an organism indicates infection has occurred, and elevated antibodies against self-antigens indicate autoimmune disease. Natural antibody can be present without any previous infection or any known cause. Elevated measles antibody in CSF with IgG indicates old infection and IgM indicates recent infection. Subacute sclerosing panencephalitis (SSPE) is a rare late complication of measles occurring in 1/1,00,000 children in the age group of 5–14 years. It is characterized by cognitive decline, slow myoclonus, seizures and is potentially fatal. Incubation period varies from few months to years. No definite treatment is available for cure. It has as a characteristic EEG picture showing periodic complexes consisting high amplitude slow waves recurring at intervals of 4–6 s and with a normal background to start with, as it is of subcortical origin. As the disease advances, background becomes altered with appearance of slow waves and in few cases, the superimposed discharges can disappear. This classical periodic complex of subcortical origin is diagnostic of SSPE. CSF is considered confirmatory.[6] However, the antibody tests cannot clearly distinguish between intrathecal synthesis and intrathecal introduction due to damage to blood-brain barrier or lumbar puncture.[78] Elevated measles antibody is reported in patients with multiple sclerosis and other neurodegenerative diseases.[9]
Patients and Methods
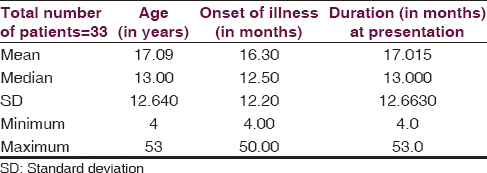
Patients who had CSF measles antibody titers positive in significant titers seen by us in the last 4 years were retrospectively analyzed and the data was entered in an Microsoft Excel Worksheet (.xlsx) for the following parameters: Age, gender, vaccination status, onset of symptoms, duration from onset to peak, presenting symptoms, bowel and bladder involvement, seizures, focal signs, myoclonus, psychosis, EEG changes, imaging changes, hyponatremia, hypokalemia, presence of autoantibodies, treatment received and outcome at 6 months, 1-year and 3 years [Table 1 and Figure 1]. Measles antibody titers standardization in our institute is done as follows. It is done using ELISA technique and standardization and cut-off values were established in the neurovirology laboratory of NIMHANS between 1986 and 1987. 300 CSF samples belonging to patients with various neurological disorders were taken during spinal anesthesia for minor procedures. Raised IgG > 1:25 antimeasles antibody titer was considered as diagnostic by studying the above samples correlating with the clinical picture.[8] Oligoclonal band to decide on intracranial synthesis of IgG antibodies against measles antigen was not carried out in all the cases. Microneutralization test and immunofluorescence tests were carried out in few cases where the CSF antibody titers were very high for antimeasles IgG antibody but clinical, radiological, and EEG picture was not typical of SSPE [Figures 2 and 3].

- Age wise distribution of patients

- Microneutralization test to see the difference between the positive and the negative

- Immunofluorescence test
Those who showed clinical and laboratory mismatch underwent testing of oligoclonal band, anti-NMDA, thyroid peroxidase (TPO) VGKC antibody, and complete vasculitic and chronic meningitis workup.
Treatment given and follow-up
Those with typical clinical, electrophysiological, radiological, and microbiological picture which included 27 cases were treated with Isoprinosine, Sodium Valproate, and Clobazam. The other 6 patients received Methyl prednisolone Pulse of 5 g every month for 6 months in all cases. All the 6 patients had received antipsychotics and anticonvulsants from other institutions. Four of them had received Isoprinosine, and five of the patients were told that they are suffering from an incurable slow virus disease. 2 patients received a single pulse of IvIg in addition at 2 g/kg. 1 patient in addition to the methyl prednisolone pulse had to be initiated on 5 large volume plasmapheresis monthly for 6 months.
Of the 33 patients with CSF antimeasles antibody titers positive in very high titers, 27 patients had a follow-up up to 1-year and out of the rest 6 patients, 1 patient has 1-year follow-up, 2 patients have 4-year follow-up and 3 patients have 2½ year follow-up. Of the 27 patients on 1-year follow-up, 15 patients have become bedbound. The rest 12 patients have severe cognitive impairment, but myoclonic jerks and seizures are under moderate control. They are not available for follow-up after that. The 4-year follow-up group has gone into complete remission with complete independence for activities of daily living, and 1 patient had fully resumed her job as a beautician. Other 3 patients of this group have not been able to take up the high intellectual jobs they were doing before. The 2 patients who were available for the 2½ years of regular follow-up are cognitively active for activities of daily living but could not return to their jobs.
Observations
Clinical picture, imaging, lab data, and results
All the patients presented with rapidly progressive cognitive impairment. 27 patients out of 33 had slow myoclonus, and seizures were present in 13 out of 33 and 7 out of 27. Psychosis was present in all 6 patients with atypical presentation and 3 patients out of the 27 with the typical presentation. History of fever with rash was given by 6 patients, and 5 patients gave the history of vaccination for measles. Seizures were present in 14 patients whereas cognition was affected in 28 patients. Myoclonus (slow and fast) was seen in all 33 patients. Speech abnormalities were detected in 12 patients. 24 patients had psychosis, and 4 had hyponatremia. Anti VGKC antibodies were seen in 2 patients, anti-NMDA and anti-TPO antibodies were seen in 1 patient each.
Cerebrospinal fiuid antimeasles IgG antibody titer was 1:625 in all cases which was considered to be highly significant as per the normative data of our laboratory.[8] CSF cell count varied from 0 to 20, proteins 17–151 mg/dl, sugar 15–100 mg/dl, chlorides 111–133 mEq/dl in the 27 typical cases. In the other 6 patients, cell count varied from 0 to 20/mm3, and protein from 15 to 59. CSF oligoclonal band was done in only 4 of the 27 patients which showed a positive peak reported as infection related oligoclonal bands.
In the other six atypical cases, VGKC antibody was positive in 2 patients, NMDA positive in one case, TPO antibody 3-fold elevated in one case and the other 2 patients could not afford VGKC, NMDA, or GAD antibody profiling. TPO antibody was negative in them.
Electroencephalography in group 1 showed a wide range of abnormalities varying from background slowing, burst suppression, and asymmetry [Figure 4a]. However, high voltage synchronous, symmetrical, recurrent slow waves at intervals of 4–12 s were seen in 26 out of the 27 typical SSPE cases. Sensory evoked potential (SEP) showed giant potential in 4 out of 27 patients [Figure 5]. MRI done in 18 patients out of 27 showed white matter changes in 14 and 1 patient showed features of thalamic and brainstem signal changes suggestive of necrotizing encephalitis.

- (a) Midpositive triphasic waves, sharp waves, and slow waves resembling creudzfeldt jakob disease in autoimmune encephalitis, (b) electroencephalographic showing classical periodic complexes in sub-acute sclerosing panencephalitis

- Giant sensory evoked potential seen in sub-acute sclerosing panencephalitis and not in autoimmune encephalitis
Electroencephalography showed recurrent mid positive triphasic waves in 2 patients and slow waves in group 2. Classical periodic complex of SSPE was not seen in any of the six cases [Figure 4b]. MRI showed cingulum and insular signal changes in 2 patients. Bilateral hippocampal and medial temporal change in one case. Periventricular white matter changes in one case. Other 2 patients showed mild diffuse atrophy [Figures 6a, b and 7].

- (a) Hashimoto's encephalopathy showing periventricular white matter changes (b) hyperintensities in cingulum and insular region seen in autoimmune encephalitis

- Magnetic resonance imaging images in sub-acute sclerosing panencephalitis showing white matter and cerebellar changes
Statistical evaluation also showed out of the 33 patients with antimeasles antibody in CSF, 6 belonged to the higher age group ranging from 22 to 53 years. Cognitive dysfunction was seen in both the groups, but there was no statistical significant difference between the two groups. Psychosis was seen in the second group of patients and there was significant difference between the two groups (P = 0.02), slow myoclonus significant in first group (P = 0.028) and weakness was significant in the second group (P = 0.028) and double incontinence in the second group (P = 0.0001). Early bladder and bowel involvement were seen in the second group (P = 0.0001).
Magnetic resonance imaging showed significant gray matter involvement in group 2 as compared to the first group (P = 0.005) as well as significant cerebellar involvement (P = 0.028).
Discussion
Measles antibody in CSF can become elevated in situ ations other than SSPE probably due to damage to blood-brain barrier. In conditions like multiple sclerosis, it is consistently reported which could indicate it can be a nonspecific epiphenomena in autoimmune disorders. Intrathecal synthesis may occur postulating an active immunogenic role for the measles virus in autoimmune disorders and great caution is required in interpretation of results without proper clinical correlation in view of the gravity of the consequences of such diagnosis. Older age group, longer duration from onset to peak, significant psychosis, generalized seizures in addition to myoclonus, presence of bladder, bowel involvement, hyponatremia, hypokalemia, lack of involvement of macula, nonspecific changes in the EEG, and normal SEP are negative predictors of SSPE even when the antibody titers against measles antigen are high in the CSF. This should be taken as an indication to look for the possibility of other autoimmune illnesses before the diagnosis of SSPE is confirmed. However, we did not have the facility to assess serum levels of antimeasles antibody in our patients and compare the titers with CSF antibody which could have given us some insight into the leakage of antibody from serum to CSF.
Conclusion
A small subgroup of patients showing significant titers of CSF IgG antimeasles antibody but lacking other features do not suffer from SSPE. Those who present at a later age have psychosis more than cognitive decline, generalized tonic-clonic seizures and focal myoclonus more than slow myoclonus, early incontinence of urine and motion with nonspecific EEG changes and MRI showing gray matter and cerebellar changes need caution and careful assessment of the specificity of high titers of antimeasles antibody and further evaluation like microneutralization and indirect immunofluorescence tests are indicated. Evaluation for autoimmune encephalitis is mandatory in those patients who show the discordance between CSF antimeasles antibody titers and other parameters. It is very important to correlate all the features before they are labeled as suffering from this untreatable slow virus infection in view of the great therapeutic and prognostic importance in these cases.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Limbic encephalitis: Extension of the diagnostic armamentarium. J Neurol Neurosurg Psychiatry. 2007;78:332-3.
- [Google Scholar]
- Limbic encephalitis not associated with neoplasm as a cause of temporal lobe epilepsy. Neurology. 2000;55:1823-8.
- [Google Scholar]
- Paraneoplastic limbic encephalitis: Neurological symptoms, immunological findings and tumour association in 50 patients. Brain. 2000;123(Pt 7):1481-94.
- [Google Scholar]
- The Immune System in Health and Disease, Immunobiology. (5th ed). New York: Garland Science; 2001. p. :12-50.
- [Google Scholar]
- Pam Tomlin, Rachel Keen, SSPE Factsheet. Available from: http://www.encephalitis.info/files/5413/4012/7902/FS_004V1.pdf
- [Google Scholar]
- Association of parental vaccination reports with measles, mumps, and rubella protective antibody levels: Comparison of Somali Immigrant, Hispanic Migrant, and US Children in Rochester, Minn. Mayo Clin Proc. 2002;77:241-5.
- [Google Scholar]
- Isoelectrofocussing profile of CSF proteins in subacute sclerosing panencephalitis. In: Pant B, Prabhakar S, eds. Proceedings of the Third International Symposium on SSPE. Vellore: Christian Medical College; 1989. p. :145.:149.149.
- [Google Scholar]
- Does Disease-Irrelevant Intrathecal Synthesis in Multiple Sclerosis Make Sense in the Light of Tertiary Lymphoid Organs? Frontiers in Neurology. ;5:27. doi:10.3389/fneur.2014.00027
- [Google Scholar]






