Translate this page into:
A microsurgical anterior cervical approach and the immediate impact of mechanical retractors: A case control study
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
A microsurgical anterior cervical approach with discectomy and fusion (MACDF) is one of the most widely used procedures for treating radicular disorders. This approach is highly successful; however, it is not free from complications. These can be associated with soft tissue injuries.
Aim of the Study:
The recognition of the risks for these complications should be identified for timely prevention and safe treatment.
Materials and Methods:
Study Design: Retrospective case control study. This study includes a retrospective case series of 37 patients, paying special attention to immediate complications related to the use of mechanical retraction of soft tissue (dysphagia, dysphonia, esophageal lesions and local hematoma); and a comparative analysis of the outcomes after changes in the retraction method.
Results:
All selected cases had a positive neurological symptom response in relation to neuropathic pain. Dysphagia and dysphonia were found during the first 72 h in 94.1% of the cases in which automatic mechanical retraction was used for more than one hour during the surgical procedure. A radical change was noted in the reduction of the symptoms after the use of only manual protective blades without automatic mechanical retraction: 5.1% dysphagia and 0% dysphonia in the immediate post-operative period, P = 0.001.
Conclusions:
Soft tissue damage due to the use of automatic retractors in MACDF is not minor and leads to general discomfort in the patient in spite of good neurological results. These problems most often occur when automatic retractors are used continuously for more than 1 hour, as well as when they are used in multiple levels. Dysphagia, dysphonia and local pain decreased with the use of transient manual blades for retraction, and with intermittent release following minimally invasive principles.
Keywords
Anterior cervical discectomy and fusion
dysphagia
dysphonia
soft tissue complications
Introduction
Cervical spine pain is one of the most common complaints from patients with spinal disorders. Total of 75% of symptomatic disk hernias are found in 30- to 50-year-old patients and neurological disability due to osteoarthrosis is predominant in patients over 50 years of age, with cervical spondylosis being the most common cause of spinal cord and nerve root compression.[1]
Nerve root pain may originate in several anatomical points and includes myofascial, neurological or visceral abnormalities, as well as those found in bones or ligaments. Most of the pain is due to compression of neurological structures, the most common causes being disk herniation and degenerative disease from arthrosis. Inflammatory, neoplastic and infectious processes should also be considered. Intervertebral foramen narrowing, ostophytes, spondylosis and ossification of ligaments are included among the diseases caused by degenerative arthrosis.[2]
Up to 70% of reported cases with cervical disk pathology involve levels C5–C6 and C6–C7. The current treatment for this diagnosis is done by using anterior cervical approach with discectomy and fusion (ACDF) as described by Smith and Robinson.[34] Resulting as the procedure of choice for neurosurgeons, because of its short surgical time, anatomical approach, fast recovery, and good cervical stabilization. Due to the different anatomical structures manipulated during this procedure, multiple complications can arise; these are most of the time considered transient and therefore underestimated, in spite that they are associated to the main complaints stated by patients in the immediate post-operative period (72 h): Dysphagia, dysphonia, esophageal dysfunction and local hematoma. The majority of patients have a good recovery in one week. The indiscriminate use of automatic retractors can increase these symptoms, and we need to think in the best way to prevent it.[5678910]
Materials and Methods
Patient selection
It is a retrospective case-series study of 37 patients in a non-random historical sequence of microsurgical anterior cervical approach with discectomy and fusion (MACDF) performed by the same surgeon. There were two groups of patients in the study: Group A: [First historical group] MACDF using a fixed mechanical retractor (20 patients 80% one level, 20% two levels), and Group B [Second historical group]: MACDF without fixed mechanical retractor and only using manual protective blades as a Deavers modified spatula (17 patients 82% one level, 18% two levels). Our cases adjustment involving only vertebral levels of segments C5–C6 and C6–C7 were included. An inclusion criterion was that the patient should have improved at least 5 points in the visual analogue scale (VAS), after the procedure compared to preoperative neurological pain level. Consequently, the study focused only on the comparative analysis of complications pertaining to mechanical retraction of soft tissue; local pain with greater than five in VAS, dysphagia (VAS applied to pain related to swallowing time), dysphonia (we evaluated the clinical changes in phonation until the patient felt that his voice was standard as in previous conditions to surgery), injury of the recurrent laryngeal nerve, esophageal lesion, local hematoma, and others. The immediate post-operative data (72 h) was collected in both groups of patients with follow-up every 3 months during 1 year. The selection of the retraction technique was determined in non-random sequential historical evolution, where the first group was carried out under mechanical automatic retraction and the second group with manual retraction with a Deavers modified spatula.
Ethical issues
All ethical considerations and informed consent were approved by the bioethics committee of our institution. Registration as a clinical trial was not required because it is a retrospective descriptive study without experimental intervention.
Surgical technique
Every patient was approached with a transverse 5 cm incision in the right anterolateral segment, at the corresponding level, confirmed with fluoroscopy. A conventional surgical access in the platysma was used, and only blunt dissection was performed in the segment medial to the sternocleidomastoid. In Group A, automatic retractors were placed at the corresponding level in lateral points of the longus colli muscles for the entire duration of the surgery. The variant used in Group B undergoing surgery without automatic retractors was, the exclusive use of protective blades spatula without traction for the vascular carotid-jugular bundle (lateral wall), and a medial 5 cm. Wide curve retractor of a different shape, as a Deavers modified spatula with blunt and angulated borders, with intermittent manual retraction and support in the arm of the vertebral retractor itself [Figures 1 and 2], exerting no pressure on tissue during silent times (fluoroscopy time). The rest of the procedure was done with conventional microsurgical approach and micro-drill, using a rectangular titanium cage (RABEA, Signus-Germany) in one or two levels as required for the case [Figures 3 and 4].
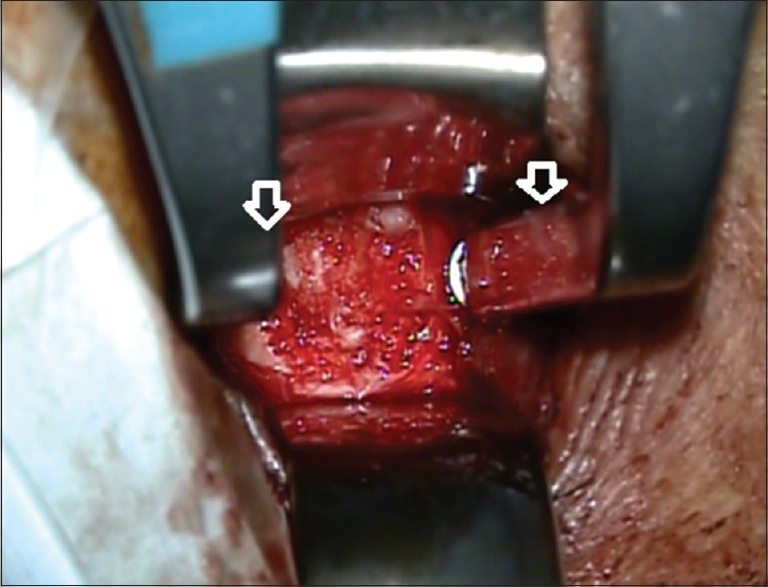
- Anterior cervical approach without fixed automatic retractors, note the use of lateral protective (vascular bundle) and medial support of lever arms fixing vertebral spacer screws (a). The intersomatic space and microscope visibility are acceptable

- The approach allows deep plane maneuvering with instruments. Is evident the microsurgical view of anatomical structures as the posterior longitudinal ligament, uncinate apophysis and interbody platforms

- Image of the reach of the instruments through intra-operative fluoroscopy, with no evidence of automatic retractors. Note the effect of the milling on the edge of bone spurs, as evidence that deep access
is possible without the need for automatic separators

- Position of the interbody titanium implant is shown in position at a supraselective space
Statistical analysis
The results are expressed as percentage, odd radio and mean. The data was analyzed using Fisher's Exact Test, taking P ≤ 0.05, as the limit of significance.
Results
In every case selected, radicular symptoms improved (inclusion criteria). Patients had a good post-operative evolution in terms of neurological symptoms and mechanical type pain, with at least a 5-point reduction in the VSA. The results only include outcomes related to discomfort in the surgical site associated with the use of mechanical retraction on soft tissue.
Immediate dysphagia and dysphonia were found in 94.1% of cases in which automatic mechanical retraction was used permanently over 1 hour or more. Only one case which persisted with dysphonia was evaluated by the ear nose and throat service to propose rehabilitation. In the case of local hematoma only clinical inspection was required.
We found a post-traumatic esophageal diverticulum in one case that had history of two surgical interventions [Figure 5]. A radical change in the reduction of local symptoms was noted after only using protective blades without automatic mechanical retraction (P = 0.001), resulting in only 5.9% dysphagia and 0% dysphonia in the post-operative period at 72 h. These symptoms were transient and subsided in the first 5 days after the procedure [Table 1] [Graphic 1].

- Diverticulum esophagicus as a cause of dysphagia, developed after trauma brought about by the use of mechanical fixed retractors that weakened the wall. In this case, it required surgery for esophageal repair in a second surgical procedure


- Evidence of soft tissue symptoms after microsurgical anterior cervical approach with discectomy and fusion at 72 hours. Fisher's exact test: P=0.001
Discussion
The microsurgical anterior cervical approach with discectomy and fusion (MACDF) is one of the most used surgical techniques and widely accepted for treatment of radicular pain, over the past 50 years.[3411121314] Although this procedure is highly successful, it is not exempt of complications, affecting soft tissue adjacent to the surgical site, nerve or vertebral tissue, causing most of the discomfort in patients during the immediate post-operative period.
Several studies evaluate the outcome of the procedure in terms of neuropathic pain control, functional recovery from myelopathy, as well as functionality and biomechanical stability. The most common complications in deep planes are dural perforation, cerebrospinal fluid leakage, meningitis, spinal epidural hematoma, contusion of a spinal nerve, nerve root lesion, transient or permanent myelopathy or, long-term disease in the adjacent segment.
Reports on soft tissues damage are scant and these complications are underestimated since they are assumed to be a “normal” part of the recovery process; however, they are the main cause of discomfort stated by the patient in the immediate post-operative period of 72 h. Some of the most common complications are as follows: Dysphagia, post-operative hematoma that may or may not require surgery due to airway obstruction, dysphonia (which can be either transient or permanent) caused by recurrent laryngeal nerve injury, esophageal perforation, tracheal injury, Horner's syndrome, superficial wound infection, pneumothorax, jugular vein or carotid artery injury, aneurysm or carotid dissection in the post-operative period, and cerebral ischemia from obstruction in the cervical carotid artery.[789101516171819]
Dysphagia is the main soft tissue complication stated by patients, which is associated to pressure on tissue exerted by the automatic retractor system. Several authors have warned about the pertinence of intermittent relaxation of the retractor as a way to prevent it, as well as to reduce the compression time of the retractor. However, in our experience, there was no significant complication reduction until the retraction method was modified. Instead of using automatic retractors, the 5 cm wide modified blade system with a blunt border and an angulated border began to be used in the lateral segment of the vascular bundle, with no retraction. In the medial border, the blade is supported as a lever by the arms of the vertebral retraction system for exposure of an intersomatic disk space, with manual support and total release in the “silent” periods of the surgical procedure (fluoroscope use and instrument check), allowing to have intermittent relaxation. Applying this variant of the technique, along with minimally invasive strategies as a microscope, we tried to preserve neural, vertebral structures, and soft tissue structures, obtaining a significant reduction in soft tissue complication and discomfort rates.
The secondary changes for repeated trauma and local ischemia during mechanical retraction for the period over 1 hour are the most important recognized factors as the cause of the inflammatory process that determines the appearance of the symptoms in the immediate period. Therefore, we believe that even when the majority of the patients are stable after 1 week and no symptoms related to the soft tissue inflammation are seen, the microsurgical approach strategy under the premise of minimal invasion may be beneficial in the immediate outcome of patients and satisfaction index.[111213141620212223]
Conclusion
Mechanical soft tissue injuries produced by automatic retractors in MACDF are not minor and lead to patient discomfort in the immediate post-operative period in spite of good neurological and biomechanical results. Dysphagia, dysphonia, local hematoma, and esophageal lesion were the most common complications. These symptoms are often found when retractors are used continuously for more than 1 hour, as well as from the use of multilevel approach compared to single level. There is a remarkable reduction of symptoms using the transient manual retraction technique with only protective blades and intermittent relaxation of the spatula, following the minimally invasive principle.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Anterior cervical discectomy and fusion: Analysis of surgical outcome with and without plating. J Clin Neurosci. 2007;14:639-42.
- [Google Scholar]
- Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Johns Hopkins Hospital Bull. 1955;96:223-4.
- [Google Scholar]
- The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A:607-24.
- [Google Scholar]
- On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine (Phila Pa 1976). 2000;25:2906-12.
- [Google Scholar]
- The impact of automatic retractors on the esophagus during anterior cervical surgery: An experimental in vivo study in a sheep model. J Neurosurg Spine. 2009;11:547-54.
- [Google Scholar]
- Can airway complications following multilevel anterior cervical surgery be avoided? J Neurosurg. 2001;94(Suppl):185-8.
- [Google Scholar]
- Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007;32:2310-7.
- [Google Scholar]
- Airway compromise due to wound hematoma following anterior cervical spine surgery. Open Orthop J. 2012;6:108-13.
- [Google Scholar]
- Complications of multilevel anterior cervical fusion. Tzu Chi Med J. 2004;16:79-84.
- [Google Scholar]
- Illiac crest autograft versus alternative constructs for anterior cervical spine surgery: Pros, cons, and costs. Surg Neurol Int. 2012;3(Suppl 3):S143-56.
- [Google Scholar]
- Cervical disc arthroplasty: Pros and cons. Surg Neurol Int. 2012;3(Suppl 3):S216-24.
- [Google Scholar]
- Anterior endoscopically assisted transcervical reconstruction of the upper cervical spine. Eur Spine J. 2011;20:1526-32.
- [Google Scholar]
- Full-endoscopic technique for anterior cervical discectomy and interbody fusion: 5-year follow-up results of 67 cases. Eur Spine J. 2011;20:899-904.
- [Google Scholar]
- Effect of retropharyngeal steroid on prevertebral soft tissue swelling following anterior cervical discectomy and fusion: A prospective, randomized study. Spine (Phila Pa 1976). 2011;36:2286-92.
- [Google Scholar]
- Anterior cervical discectomy with fusion in patients with cervical disc degeneration: A prospective outcome study of 258 patients (181 fuses with autologus bone graft and 77 fused with PEEK cage) BMC Surg. 2010;21(10):10.
- [Google Scholar]
- Retropharyngeal cerebrospinal fluid collection as a cause of postoperative dysphagia after anterior cervical discectomy. Surg Neurol. 2007;67:499-503.
- [Google Scholar]
- Dysphagia after anterior cervical decompression and fusion: Prevalence and risk factors from a longitudinal cohort study. Spine (Phila Pa 1976). 2005;30:2564-9.
- [Google Scholar]
- Intra-Esophageal retraction pressure during anterior cervical plating versus cervical disc replacement: A cadaveric study. J Spinal Disord Tech. 2006;19:312-7.
- [Google Scholar]
- Less exposure surgery for multilevel anterior cervical fusion using 2 transverse incisions. J Neurosurg Spine. 2012;17:194-8.
- [Google Scholar]
- Posterior surgery for cervical myelopathy: Laminectomy, laminectomy with fusion, and laminoplasty. Asian Spine J. 2008;2:114-26.
- [Google Scholar]
- Alternative grafts in anterior cervical fusion. Clin Neurol Neurosurg. 2013;115:2049-55.
- [Google Scholar]
- Developing an anterior cervical discectomy and fusion simulator for neurosurgical resident training. Neurosurgery. 2013;73(Suppl 1):100-6.
- [Google Scholar]






