Translate this page into:
First-drug treatment failures in 42 Turkish children with idiopathic childhood occipital epilepsies
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The early and late benign occipital epilepsies of childhood (BOEC) are described as two discrete electro-clinical syndromes, eponymously known as Panayiotopoulos and Gastaut syndromes. The purpose of this study was to identify predictors of failure to respond to the initial antiepileptic drug (AED).
Materials and Methods:
A total of 42 children with BOEC were enrolled. Predictive factors were analyzed by survival methods.
Results:
Among the 42, 25 patients (59.5%) were boys and 17 (40.5%) were girls and the mean age at the seizure onset was 7.46 ± 2.65 years (4–14 years). Of the 42 patients, 34 (81.0%) were treated relatively successfully with the first AED treatment, and 8 (19.0%) were not responded initial AED treatment. There was no correlation between response to initial AED treatment and sex, consanguinity, epilepsy history of family, age of seizure onset, frequency of seizures, history of status epilepticus, duration of starting first treatment, findings on electroencephalogram. However, history of febrile seizure and type of BOEC were significantly associated with failure risk.
Conclusions:
Factors predicting failure to respond to the AED were history of febrile seizure and type of BOEC in children with BOEC.
Keywords
Children
failure risk factors
first antiepileptic drug
idiopathic occipital epilepsies of childhood
Introduction
The benign occipital epilepsies of childhood (BOEC) are classified into two apparently discrete groups comprising an early (Panayiotopoulos-PS) and late (Gastaut-GS) form.[1] In PS, children present at a mean of 4.7 years (range 1–14 years) with rare seizures, which are prolonged and nocturnal. Seizures begin with autonomic features such as vomiting, pallor and sweating followed by tonic eye deviation, impairment of consciousness and may evolve to a hemi-clonic or generalized convulsion. Autonomic status epilepticus may occur. Prognosis is excellent.[23] Gastaut syndrome presents at a mean of 8 years (range 3–16 years). Seizures are frequent, brief and diurnal. They comprise simple partial seizures characterized by initial visual hallucinations such as phosphenes and/or ictal blindness and illusions; post-ictal headache is common. Impairment of consciousness is rare unless associated with hemi-clonic or generalized convulsions. Seizures remit within 2–5 years.[45]
In literature, we have not found studies are re-available on factors associated with initial poor response to antiepileptic drugs (AED) with BOEC. Therefore, we conducted a retrospectively study designed to identify the risk factors associated with initial poor response to AEDs in children with BOEC.
Materials and Methods
This study was conducted a retrospective study of 42 children diagnosed with BOEC and started on an AED in the pediatric neurology department of our hospital.
Children were included in the study if they met both the clinical and electroencephalographic criteria of benign childhood epilepsy with BOEC as set out by the International League against Epilepsy in 1989[1] and treated with AEDs for the 1st time. The AED treatment has started if they have atleast two unprovoke typical seizures and abnormal findings on electroencephalogram (EEG). Children with obvious neurological deficit were excluded from the study.
The data were retrospectively collected from the clinic files and included sex, consanguinity, history of family epilepsy and febrile seizure, age of seizure onset, frequency of seizures, type of BOEC, history of status epilepticus, duration of starting first treatment, and EEG findings (lateralization and suppressed by eye opening).
Success of initial AED was defined as obtaining complete seizure control with the first AED. Failure of initial AED treatment was defined as the inability to attain complete seizure control with the first appropriate AED.
The SPSS version 19.00 was used for statistical analysis. Statistical significance was accepted at P < 0.05. The Chi-square tests were used to determine the associations between categorical data. We carried out univariate and multivariable analyzes of potential predictors of recurrence risk using by Cox regression analysis. The level of statistical significance was established at P < 0.05. Initially, first we performed a univariate analysis, in order to determine which would use in multivariate analysis.
Results
A total of 42 children, mean age 7.46 ± 2.65 years (4–14 years), were included in this study. Among the 42 patients, 25 (59.5%) were boys and 17 (40.5%) were girls, and the mean age at the seizure onset was 6.53 ± 2.02 years (3–13 years). Of the 42 patients, 34 (81.0%) were treated relatively successfully with the first AED, and 8 (19.0%) were not responded to initial AED treatment.
Of these 42 patients, 29 (69.0%) (17 boys, 12 girls) satisfied the criteria for PS type; the average age for onset of seizures was 5.41 ± 1.34 years (range, 3–9 years). The remaining 13 (31.0%) patients (8 boys, 5 girls) met the criteria for GS type; the average age for onset of seizures was 8.92 ± 1.97 years (range, 6–13 years).
Of the 29 patients with PS, 26 (89.7%) were treated relatively successfully with the first AED, and 3 (10.3%) were not responded initial AED treatment. Whereas, in 13 patients with GS, 8 (61.5%) patients were treated relatively successfully with the first AED, and 5 (38.5%) were not responded initial AED treatment.
Among the 42 treated patients, 27 patients (64.3%) were treated with carbamazepine (CBZ), 12 patients (28.5%) were treated with valproic acid (VPA), and 3 patients (7.2%) were treated with levetiracetam (LEV).
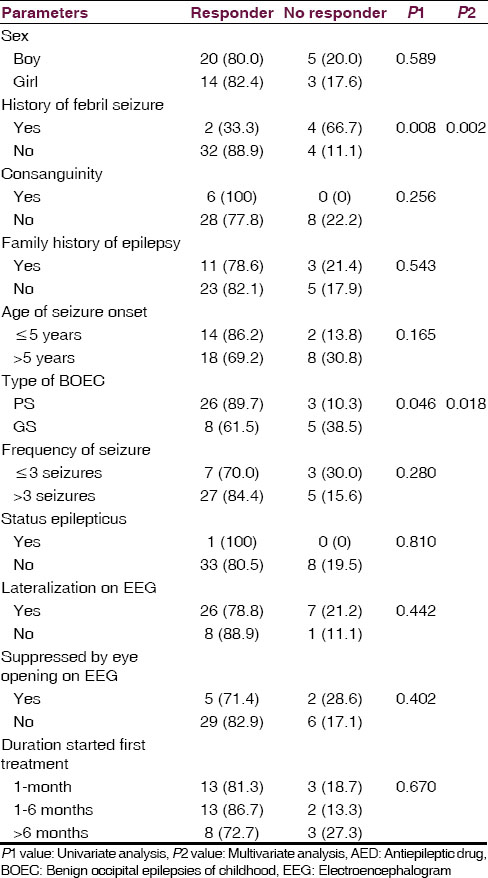
There was no correlation between response to initial AED treatment and sex, consanguinity, epilepsy history of family, age of seizure onset, frequency of seizures, history of status epilepticus, duration of starting first treatment, findings on EEG. However, there was statistically significant correlation between response to initial AED treatment with a history of febrile seizure and type of BOEC in the univariate analysis. In the multivariate analysis, history of febrile seizure and type of BOEC were found as the risk factors influencing response to initial AED treatment.
The general characteristics of children treated with initial AED treatment, overall and for successful vs. failed treatment shown in Table 1.
Discussion
Occipital epilepsies account for approximately 5–10% of all epilepsies.[6] The cause may be idiopathic or symptomatic. Symptomatic occipital seizures may start at any age and at any stage after or during the course of the underlying causative disorder. Idiopathic occipital epilepsy usually starts in childhood.[67]
There have been many studies for determining the risk factors affecting failure to respond to the initially prescribed AED in epileptic children in literature.[89] Reported rates have varied from 16% to 56% in the literature.[9] Furthermore, in children with epilepsy, if the initial AED fails to control seizures, the prognosis for seizure control is often thought to be poor. There are no studies specifically in with BOEC associated with the prognostic significance of initial AED failure.
We detected 19.0% of children were not responding successfully for the first AED treatment in our study. This rate was 10.3% in patients with PS, whereas, this rate was 38.5% in patients with GS.
Gökçay et al.[10] reported male dominance, whereas Du et al.[11] noted female to dominance in BEOC cases. In our study, there was a male predominance (59.5%). We did not find sex as a significant risk factor for respond to treatment with the first AED treatment.
We found that the history of febrile seizure and type of BOEC were a significant risk factor for failure to respond to the initial AED treatment. In GS type, we detected high rate failure to respond to the initial AED than PS. This pointed that GS type especially was a significant risk factor for failure to respond to the initial AED treatment. In our study, we were found that the history of febrile seizure and type of BOEC were significantly increased failure risk in both univariate and multivariate analysis.
We did not identify family history of epilepsy, consanguinity, frequency of seizures, history of status epilepticus, and duration of starting first treatment as risk factors for failure to respond to the initial AED treatment.
In our study, we considered background rhythm, lateralization of interictal spikes and suppressed by eye opening findings on EEG. We detected no on EEG findings as a risk factor for failure to respond to the initial AED.
Antiepileptic drug treatment is similar to that for any other type of focal seizures, is usually effective, and should be initiated as soon as possible. Recommended AEDs for monotherapy include CBZ, oxcarbazepine, VPA, LEV, and lamotrigine. There is no convincing evidence, that any therapy will be more effective than other to control seizures, and it is reported that some patients are sometimes resistant to treatment. Most clinicians treat seizures with CBZ or VPA.[121314] García and Rubio[15] reported that LEV used in three children with PS type. They found efficacy on seizure control in PS. We used CBZ treatment in 27 patients, VPA treatment in 12 patients, and LEV treatment in 3 patients. We did not consider efficacy difference with relation of AEDs.
Conclusion
We found the history of febrile seizure and type of BOEC is as risk factors for failure to respond to the initial AED treatment in this study. There is still no general agreement on the criteria to predict respond to treatment with the first AED. We think the differences reported regarding the effect of risk factors can be attributed to differences in the study designs and characteristics of the studied populations.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1989;30:389-99.
- [Google Scholar]
- Benign childhood epilepsy with occipital paroxysms: A 15-year prospective study. Ann Neurol. 1989;26:51-6.
- [Google Scholar]
- Panayiotopoulos syndrome: A benign childhood autonomic epilepsy frequently imitating encephalitis, syncope, migraine, sleep disorder, or gastroenteritis. Pediatrics. 2006;118:e1237-43.
- [Google Scholar]
- A new type of epilepsy: Benign partial epilepsy of childhood with occipital spike-waves. Clin Electroencephalogr. 1982;13:13-22.
- [Google Scholar]
- Clinical and electroencephalographic findings in early and late onset benign childhood epilepsy with occipital paroxysms. Brain Dev. 2001;23:401-5.
- [Google Scholar]
- Occipital lobe developmental malformations and epilepsy: Clinical spectrum, treatment, and outcome. Epilepsia. 1997;38:175-81.
- [Google Scholar]
- Seizure relapse following medication withdrawal in childhood epilepsy. Arch Dis Child. 2011;96:113.
- [Google Scholar]
- Antiepileptic drug withdrawal in childhood epilepsy: What are the risk factors associated with seizure relapse? Eur J Paediatr Neurol. 2012;16:599-604.
- [Google Scholar]
- Clinical analysis of childhood occipital lobe epilepsy in 43 Taiwanese patients. Pediatr Neurol. 2007;36:387-92.
- [Google Scholar]
- Occipital lobe epilepsies. In: Panayiotopoulos CP, ed. A Clinical Guide to Epileptic Syndromes and their Treatment. London: Springer; 2010. p. :473-82.
- [Google Scholar]
- Panayiotopoulos syndrome and Gastaut type idiopathic childhood occipital epilepsy. In: Roger J, Bureau M, Dravet C, Genton P, Tassinari CA, Wolf P, eds. Epileptic Syndromes in Infancy, Childhood and Adolescence. France: John Libbey Eurotext; 2005. p. :227-53.
- [Google Scholar]
- Childhood epilepsy with occipital paroxysms: Clinical variants in 134 patients. Epilepsia. 2000;41:1522-33.
- [Google Scholar]
- Efficacy and safety of levetiracetam in the treatment of Panayiotopoulos syndrome. Epilepsy Res. 2009;85:318-20.
- [Google Scholar]






