Translate this page into:
Disappearing lytic lesion of skull
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 9-year-old child presented to our pediatric outpatient department with complaints of recent onset of swelling in scalp over the right lateral frontal region, which was associated with mild pain. Skull radiograph showed a well-defined lytic lesion in the right frontal bone with beveled edges [Figure 1] and a differential diagnosis of eosinophilic granuloma was suggested. Routine blood investigations including peripheral smear, bone marrow, bone scan and ultrasonography of abdomen were normal except for a raised erythrocyte sedimentation rate (ESR). An incisional biopsy of the skull lesion confirmed the diagnosis of eosinophilic granuloma. The patient was managed conservatively and followed up. After 6 months of follow up, complete disappearance of the lytic lesion in the skull [Figure 2] was seen. The patient is asymptomatic till now, that is, after 2-year follow up.
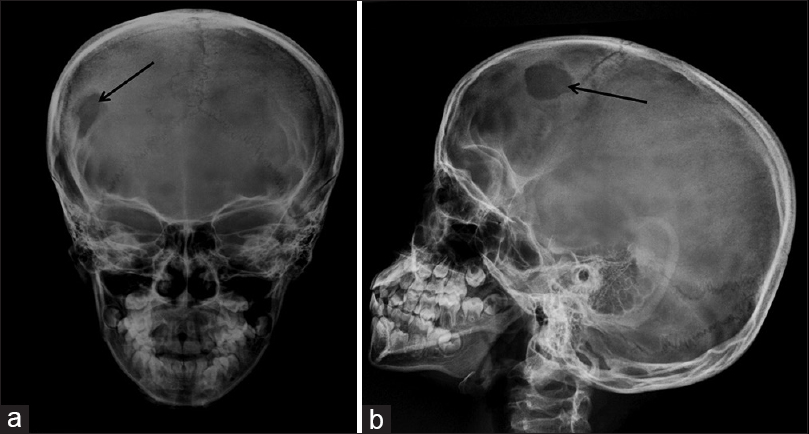
- Anteroposterior (a) and lateral (b) view radiographs of skull show a well-defined lytic lesion with beveled edges involving the right frontal bone (black arrows)

- Skull radiograph (lateral view) taken after 6 months of follow up shows complete resolution of the lytic lesion
Localized Langerhans cell histiocytosis, also known as eosinophilic granuloma, is a benign tumor-like condition characterized by clonal proliferation of Langerhans type histiocytes.[1] The treatment recommended for solitary calvarial eosinophilic granuloma is surgical resection by curettage, craniectomy or craniotomy.[12] Observation alone can be considered in the management of children with solitary calvarial mass which helps in delaying surgical intervention and allow time for spontaneous resolution.[12] There are studies confirming this type of management and our case also establishes the fact that solitary calvarial eosinophilic granuloma can be managed with observation alone also.[12]
References
- Nonoperative management of solitary eosinophilic granulomas of the calvaria. J Neurosurg Pediatr. 2013;12:1-5.
- [Google Scholar]
- Spontaneous resolution of calvarial eosinophilic granuloma in children. Pediatr Neurosurg. 2003;38:247-52.
- [Google Scholar]





