Translate this page into:
Spinal accessory nerve schwannomas masquerading as a fourth ventricular lesion
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Schwannomas are benign lesions that arise from the nerve sheath of cranial nerves. The most common schwannomas arise from the 8th cranial nerve (the vestibulo-cochlear nerve) followed by trigeminal and facial nerves and then from glossopharyngeal, vagus, and spinal accessory nerves. Schwannomas involving the oculomotor, trochlear, abducens and hypoglossal nerves are very rare. We report a very unusual spinal accessory nerve schwannoma which occupied the fourth ventricle and extended inferiorly to the upper cervical canal. The radiological features have been detailed. The diagnostic dilemma was due to its midline posterior location mimicking a fourth ventricular lesion like medulloblastoma and ependymoma. Total excision is the ideal treatment for these tumors. A brief review of literature with tabulations of the variants has been listed.
Keywords
Accessory nerve schwannoma
cisternal variant
cranial nerve schwannoma
11th nerve schwannoma
fourth ventricular tumor
jugular foramen tumors
neurinoma
schwannoma
Introduction
The authors report a case of accessory nerve schwannomas of the cisternal type presenting as a fourth ventricular lesion with cervical extension. Spinal accessory nerve schwannomas are rare with very few cases reported so far [Table 1].[1234567891011121314151617181920212223] The spinal accessory nerve has a cisternal, a foraminal (jugular) and an extracranial course. The tumors can be anywhere along this course. There are only 25 reported cases of the cisternal variant of accessory nerve schwannomas out of which only 1 case has been reported in the fourth ventricle. The fourth ventricular variant differentials include medulloblastoma, ependymoma etc., A brief review of literature has been done with an attempt to list the cases reported so far.

Case Report
A 22-year-old man presented to us with raised intracranial pressure type of headache with obscuration of vision for about 6 months in duration. The patient complained of gradual loss of vision in the left eye since 3 months prior to presentation. Also, over the last month he has had severe gait ataxia and hence was unable to walk without support. His examination revealed florid papilledema in the right eye with concentric field cuts and in the left eye secondary optic atrophy with no perception of light.
MRI of the brain revealed a large contrast enhancing heterogeneous lesion that was hypo intense on T1 weighted image and hyperintense on T2 weighted image with areas of necrosis and calcification. The lesion was expanding the fourth ventricle causing obstructive hydrocephalus. It was found extending inferiorly through the foramen magnum into the upper cervical canal till C2 vertebra level displacing the medulla and cervical spinal cord anteriorly and to the right side [Figure 1].

- Lesion (yellow arrow) is mixed in intensity (Hypo to isointense) on T1-weighted sagittal image. (a) Lesion is heterogeneously contrast enhancing on sagittal image and (b) coronal image (c) on T1-weighted contrast image. On A,B,C images, the lesion was predominantly expanding the fourth ventricle and extending inferiorly through the foramen magnum into the upper cervical canal till C3 vertebra level on left side displacing the medulla and cervical spinal cord anteriorly and to the right side. T2-weighted axial image the lesion is predominantly hyperintense with areas within of iso-intensity filling the fourth ventricle (d)
The patient underwent a midline sub-occipital craniotomy, with removal of posterior arch of C1. The lesion was found arising from the trunk of the left spinal accessory nerve at the level of the foramen magnum [Figure 2b]. The tumor was variable in consistency, mostly firm and vascular with some areas of cystic degeneration. The lesion was extending from C2 and into the fourth ventricle below the vermis, pushing the upper cervical cord and cervicomedullary junction to the right [Figure 2a]. The accessory nerve was thinned out and draped over the lesion and a portion of it was embedded within. The lesion was excised along with the embedded segment of the nerve, preserving the uninvolved portion which was draped over the tumor [Figure 2c].

- Tumor extending from vermis through the foramen magnum into the upper cervical. (a) Spinal accessory nerve origin of lesion. (b) Post excision visualization of the fourth ventricle (labeled) and thespinal accessory nerve trunk free of attachment (marked FNx01) and the cervical cord (marked as X). (c) Postoperative CT scan showing tumor clearance (d)
The patient recovered postoperatively with no obvious sternocleidomastoid or trapezius weakness ascribable to the left accessory nerve partial excision at the time of surgery. His post-operative contrast CT scan showed no residual lesion with resolving hydrocephalus [Figure 2d]. On last follow up after 5 months no neurological deficit was noted and he was doing well.
Pathology report revealed benign schwannoma with hyper cellular (Antoni Type A pattern) and hypo cellular (Antoni Type B pattern) areas.
Discussion
Lower cranial nerve schwannomas are rare and when present are located in the jugular foramen most commonly arise from the glossopharyngeal or vagal nerves with accessory nerve involvement being least common. The other locations in the accessory nerve course where schwannomas arise are extracranial beyond the jugular foramen in the cervical region and cisternal proximal to the jugular foramen. Both of these are very rare locations.[14]
Spinal accessory nerve schwannomas are classified accordingly by their origin as cisternal, foraminal or extracranial/cervical[12] [Figure 3a]. Our patient had a cisternal variant occupying the fourth ventricle and extending across up to the C2 level intradurally.
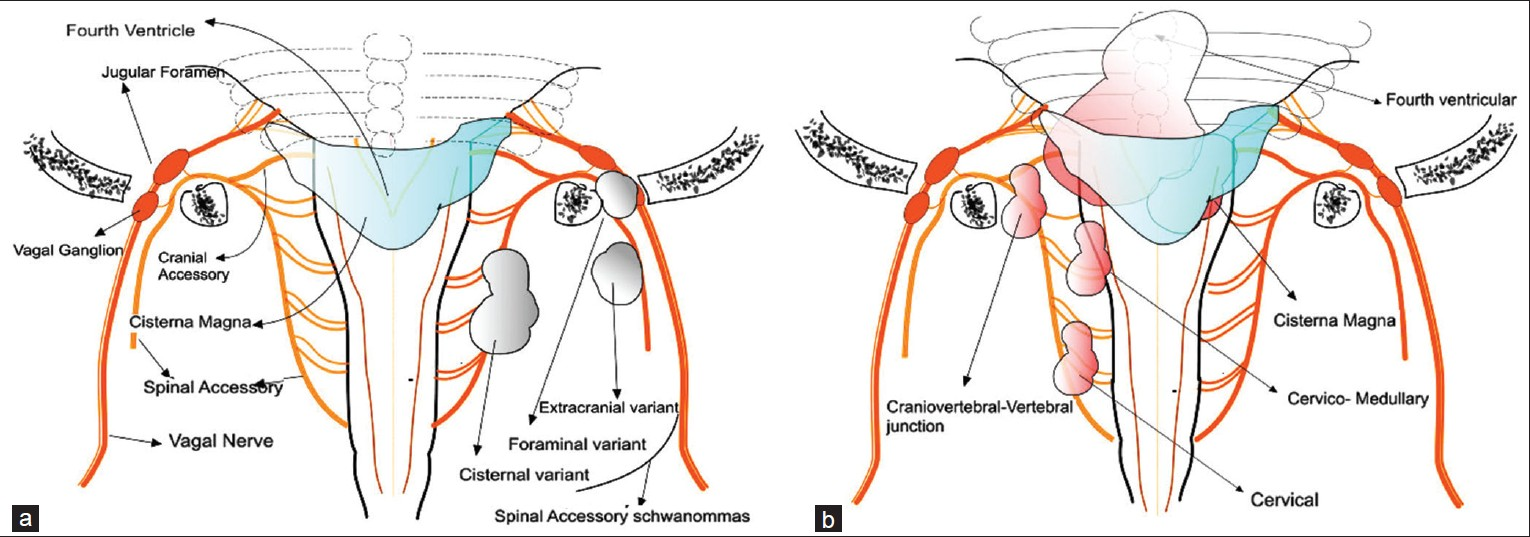
- Anatomical representation of the spinal accessory nerve with tumor types and location marked on the right side of image as 3 basic types: Intracisternal, jugular and extra cranial - grey colored lesions (a) The sub classification of the intracisternal variants based on location - pink colored lesions (b)
The spinal accessory nerve arises from the lateral funiculus of the medulla spinalis as low as the fifth cervical nerve and unites to form a single trunk. It passes between the denticulate ligament and the dorsal roots of the spinal cord through the foramen magnum passing to and entering the jugular foramen. Here it lies in the same dural sheath as the vagus but separate and receives one or two fibers from the cranial part, which arises from the nuclear ambiguous in the medulla. On exiting the jugular foramen, the spinal accessory supplies the sternocleidomastoid and trapezius, whereas the cranial portion contributes to the pharyngeal, superior laryngeal, recurrent nerve and the cardiac nerves.[22]
Intracranial accessory nerve schwannomas were classified by Julow et al.[19] into two types as intrajugular schwannomas and intracisternal schwannomas. The intrajugular variant grows into the cisterna magna whereas the intracisternal variant grows into the jugular foramen. The jugular foramen variant presents with jugular foramen syndrome with the hypoglossal and glossopharyngeal nerve involvement.[14]
The jugular variant was classified by Kaye et al.[23] into:
Type A: Primarily intracisternal with only slight extension into the bone
Type B: Primarily within the bone with or without intracranial component
Type C: Primarily extracranial with only minor extension into the bone or posterior fossa.
Jugular or the foraminal variants reported so far is 12, to the best of our knowledge, but may be unreported or missed in view of difficulty in differentiating the individual tumors by the nerve of origin as these tumors grow large by the time of presentation [Table 1].
The other variant is the pure extracranial variant and only four have been reported so far [Table 1].
Intracisternal variant occupy the cisterna magna, the fourth ventricle, spinal canal or the foramen magnum.[24] To the best of our knowledge, only 26 cases of the cisternal variant have been published so far. Out of these, 13 cases were located in the cisterna magna, 5 in the cervical canal, 5 in the cervicomedullary location, 2 in the cranio-vertebral junction and only 1 in the fourth ventricle [Table 1]. This was the variant, which was found in our patient. The lesion in our patient was also located predominantly in the fourth ventricle but with a large extension unto C2 across the cervicomedullary junction. So far only one case has been reported in the fourth ventricular location [Table 1].
In spite of their origin from the accessory nerve, these tumors tend to be located in the midline and posteriorly, probably because the cisterna magna allows sufficient space for the tumor to expand.[21]
This makes it appear more as a midline lesion and occupy the cisterna magna or the fourth ventricle, as in our case, making it difficult to differentiate from other midline posterior fossa lesions.
Thus, the cisternal variant of accessory nerve schwannomas by virtue of their extension in to various cisternal spaces can be classified by location as: [Table 1, Figure 3b].
-
Cisterna magna
-
Cervical
-
Cervicomedullary
-
Fourth ventricular
-
Craniovertebral junction.
The intracisternal variant often present with neck stiffness, secondary to accessory nerve irritation.[2414]
Unlike other cranial nerve schwannomas, the accessory nerve may or may not present with nerve dysfunction. This is dependent on the extent of nerve involvement.[2415] Our patient presented predominantly with neck pain and no signs of accessory nerve dysfunction. Signs and symptoms of cerebellar involvement, due to extension into the vermis and associated obstructive hydrocephalus was the presentation in our patient.[2]
The MRI appearances of these tumors usually have regular contours and a round or oval shape, lack edema, and enhance homogenously with contrast. Cystic degeneration is generally seen in large tumors and this may alter the otherwise uniform texture of the mass.[414]
Total removal is the primary treatment of schwannomas arising from the spinal portion of the accessory nerve. Excision of an involved segment or rootlet along with the lesion sparing the rest of the nerve in continuity, rarely results in any neurological deficit. This is because the insidious tumor growth in a portion of the nerve causes functional compensation by the remaining intact uninvolved nerve segment.[24] This was the case in our patient who had intact neurological function preoperatively and also postoperatively after removal of lesion leaving the remaining uninvolved nerve in continuity.
Conclusion
We have presented a rare case of an accessory nerve schwannoma in the fourth ventricle. The possibility of the same, as a differential diagnosis for midline posterior fossa and high cervical lesions, is the highlight of our report.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Intrasternomastoid spinal accessory nerve schwannoma: Clinical and radiological correlation. Neurol India. 2005;53:347-8.
- [Google Scholar]
- Schwannoma of the spinal accessory nerve: Case report. Neurol Med Chir (Tokyo). 2003;43:501-4.
- [Google Scholar]
- Spinal accessory schwannoma mimicking a tumor of the fourth ventricle: Case report. Neurosurgery. 2004;54:510-4.
- [Google Scholar]
- Surgical tactics and outcome of treatment in jugular foramen schwannomas. J Clin Neurosci. 2001;8(Suppl 1):32-9.
- [Google Scholar]
- Spinal accessory nerve neurinoma in the C2 spinal canal: Case report. Neurol Med Chir (Tokyo). 1987;27:1190-4.
- [Google Scholar]
- Magnetic resonance imaging of jugular foramen neurinomas. Acta Neurochir (Wien). 1989;96:83-7.
- [Google Scholar]
- Spinal accessory nerve schwannoma involving the jugular foramen. AJNR Am J Neuroradiol. 1995;16(Suppl 4):986-9.
- [Google Scholar]
- Schwannoma of the spinal accessory nerve: A case report. J Clin Diagn Res. 2013;7:1732-4.
- [Google Scholar]
- Benign solitary nerve sheath tumors of the spinal accessory nerve in the posterior triangle of the neck: Report of two cases. J Neurosurg Sci. 1992;36:247-50.
- [Google Scholar]
- Spinal root of accessory nerve shwannoma: About a new case. Neurochirurgie. 2012;58:258-62.
- [Google Scholar]
- Microneural decompression operations in the treatment of some forms of cranial rhizopathy. Acta Neurochir (Wien). 1993;125:64-74.
- [Google Scholar]
- Juxtabulbar neurinoma of the spinal accessory nerve. Neurochirurgie. 1992;38:173-8.
- [Google Scholar]
- Intracisternal schwannoma of the spinal accessory nerve: A case report. Skull Base. 2006;16:175-9.
- [Google Scholar]
- Accessory nerve schwannoma of the intracisternal type: A case report. No Shinkei Geka. 2010;38:831-7.
- [Google Scholar]
- Cerebellopontine angle meningioma associated with cranial accessory nerve neurinoma: Case report. Neurol Med Chir (Tokyo). 1994;34:225-9.
- [Google Scholar]
- Neuroma of the spinal accessory nerve disclosed by a subarachnoid hemorrhage: Case report. Neurosurgery. 1997;41:946-50.
- [Google Scholar]
- Intracisternal schwannoma of the spinal accessory nerve presenting as a normal pressure hydrocephalus syndrome: Case report and review of the literature. Neurosurg Rev. 1994;17:225-7.
- [Google Scholar]
- Neurinoma of spinal accessory nerve: Report of two cases. Acta Neurochir (Wien). 1993;69:219-24.
- [Google Scholar]
- Schwannoma of the spinal accessory nerve in the cisterna magna. Surg Neurol. 2003;59:217-22.
- [Google Scholar]
- Spinal accessory nerve schwannoma involving the jugular foramen. AJNR Am J Neuroradiol. 1995;16(Suppl 4):986-9.
- [Google Scholar]
- Anatomy and evolution of accessory nerve: Cranial or spinal origins.- A review? J Morphol Sci. 2011;28:222-7.
- [Google Scholar]






