Translate this page into:
Giant cystic intradural extramedullary pilocytic astrocytoma of Cauda equina
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Astrocytomas of Conus-Cauda equina region are rare. Astrocytomas, which are intramedullary tumors, may rarely have an extramedullary component. However, primary intradural extramedullary astrocytomas are extremely rare, with very few cases reported in the literature. We describe a giant extramedullary pilocytic astrocytoma of Cauda equina in a 20-year-old male. To the best of our knowledge, this is the first report of such a case in the available literature. This case highlights the fact that astrocytomas can be primarily extramedullary and emphasizes the need to consider pilocytic astrocytoma in the differential diagnosis of cystic Cauda equina tumors.
Keywords
Cauda equina
extramedullary
giant
pilocytic astrocytoma
Introduction
Primary spinal cord tumors account for 4-8% of central nervous system tumors.[1] In adults, ependymoma[12] is the most common primary spinal cord tumor followed by astrocytomas,[2] which are rare tumors constituting 6-8% of spinal cord tumors.[3] Cervical and thoracic regions of the spine are the most common locations for spinal astrocytomas to occur,[4] with only 4% of all spinal astrocytomas occurring in the conus-Cauda equina region.[56] It is thus rare for astrocytomas to occur in the Conus-Cauda region, where myxopapillary ependymomas account for 80% of the tumors.[7] Astrocytomas are typically intramedullary tumors and occurrence of a predominantly extramedullary astrocytoma is extremely rare.
We describe such a rare case of giant extramedullary pilocytic astrocytoma of Cauda equina. To the best of our knowledge, giant extramedullary pilocytic astrocytoma of Cauda equina has not been previously described in the available English literature.
Case Report
A 20-year-old male patient presented to us with complaints of progressive weakness in bilateral lower limbs, saddle anesthesia and bladder dysfunction for past 2 years. Clinical examination revealed weakness of bilateral lower limbs (Medical Research Council grade: 4/5), asymmetrical sensory loss in bilateral L5-S3 distribution. Patient had Foley's catheter in situ. Rest of the neurological examination was normal. Patient did not have any neurocutaneous markers.
Magnetic resonance imaging (MRI) of the lumbosacral spine showed an intradural lesion that extended from L4 to S4 vertebral segments causing scalloping of the posterior surface of vertebral bodies and expansion of the spinal canal. There was no extension into the vertebral foramina. The lesion was hypointense on T1-weighted images and hyperintense on T2-weighted images. The conus medullaris was low lying and reached up to the level of L4 vertebral body. The tumor was abutting the conus medullaris. The wall of the lesion showed intense contrast enhancement. The lesion did not extend into the foramina [Figure 1]. A screening MRI of the rest of the cranial-spinal axis was done to rule out any other lesion was done. MRI of the rest of the spine was normal [Figure 2]. However, patient was found to have right cerebellopontine angle enhancing lesion suggestive of acoustic schwannoma and another lesion in the suprasellar region suggestive of hypothalamic glioma [Figure 2].

- Cauda equina pilocytic astrocytoma. T1-weighted sagittal (a) and axial (d) images show a hypointense intradural lesion within the spinal canal extending from L4 to S4 spinal segments, causing scalloping of the posterior surface of vertebral bodies and expansion of the canal. In T2-weighted sagittal (b) and axial (e) images, the mass is predominantly hyperintense. The cord is reaching up to L4 vertebral bodies and is low-lying. The mass is not seen separate from the cord. Following contrast administration, mass lesion shows peripheral enhancement (c and f)

- Brain magnetic resonance imaging showing associated right acoustic schwannoma (a) and suprasellar contrast enhancing lesion suggestive of hypothalamic glioma (b-d). Screening MRI whole spine did not reveal any other spinal lesion (e)
Patient was operated in the prone position. Midline incision was made. The posterior bony elements were absent in the sacral region. A large intradural cystic lesion, with a thin cyst wall formed by the tumor tissue, was present in the lumbosacral region. The cyst contained xanthochromic fluid. Yellowish, soft, mildly vascular tumor was covering the nerve roots of Cauda equina and the filum terminale. The wall of the tumor and the filum terminale covered with the tumor were removed. The tumor draping the nerve roots was left behind as it entailed the risk of causing neurological deficits. Post-operative course was uneventful. Patient developed no fresh neurological deficits. Histopathological examination showed features consistent with pilocytic astrocytoma [Figure 3]. As the patient was asymptomatic for intracranial lesions a decision to conservatively follow the patient was taken.
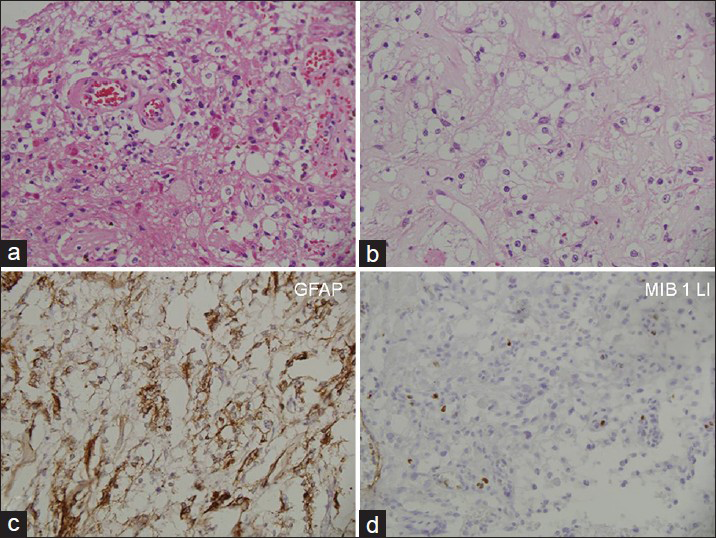
- Photomicrographs showing a sparsely cellular tumor with interspersed rosenthal fibers and granular bodies and clearing of cytoplasm of some neoplastic cells (a and b; H and E, ×200 and ×400 respectively). Tumor cells are immunoreactive for glial fibrillary acidic protein and MIB 1 labeling index is low (c and d ×200 each)
During follow-up, patient's bladder dysfunction improved gradually and presently patient is able to void himself. However, patient's motor and sensory symptoms showed neither improvement nor deterioration during 2 years follow-up.
Follow-up MRI revealed recurrence of the lesion [Figure 4]. The intracranial lesions did not increase in size during follow-up. Patient is currently awaiting second surgery.

- Follow-up magnetic resonance imaging 2 years after surgery. T1-weighted (a), T2-weighted (b) and contrast (c) sagittal views and axial T2-weighted (d) and contrast images (e) show recurrent tumor
Discussion
Spinal astrocytomas constitute 6-8% of spinal cord tumors. Only 4% of spinal astrocytomas occur in Conus-Cauda region.[56] Spinal astrocytomas can be classified histologically into diffuse fibrillary and pilocytic types.[8] Pilocytic astrocytomas of Conus-Cauda region are very rare. In a study of 79 patients with intramedullary astrocytomas by Minehan et al.[8] none of the patients had pilocytic astrocytoma in the Conus-Cauda region. Rarely astrocytomas may have an exophytic component;[9] however, extramedullary gliomas of Cauda equina region are extremely rare with only few cases reported in the literature[210111213] and a giant pilocytic astrocytoma of Cauda equina has not been previously described in the available English literature.
The extramedullary gliomas likely arise from heterotopic nests in pia and arachnoid membranes.[9] Bailey[14] was the first to suggest the glial heterotopias as the site of origin of extramedullary gliomas. Cushing and Eisenhardt[15] first reported an extramedullary spinal glioma. Patient was operated with a clinical impression of meningioma, but histopathology revealed its true identity to be an astrocytoma. In our case also, there was a preoperative diagnostic dilemma with regard to nature of the lesion and a possibility of giant cystic schwannoma was considered, though lack of involvement of foramina was against this diagnosis. The histopathological report surprised us with the diagnosis being pilocytic astrocytoma. This case emphasizes the need to consider pilocytic astrocytoma in the differential diagnosis of cystic Cauda equina tumors.
To the best of our knowledge, this is the first case of a giant Cauda equina pilocytic astrocytoma in the literature; though, there have been few reports of extramedullary astrocytoma of conus region.[101216] Singh et al.[16] reported an extramedullary astrocytoma of conus region with no attachment to surrounding neural structures. It adds another differential in the list of differential diagnoses of cystic Cauda equina lesions.
The management of pilocytic astrocytomas of spinal cord involves surgery with or without adjuvant radiation therapy. As these lesions are benign, the patients can be followed-up after surgery and radiation therapy can be given in case of recurrence/regrowth.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Descriptive epidemiology of primary spinal cord tumors. J Neurooncol. 2008;87:173-9.
- [Google Scholar]
- Intradural spinal tumors: Current classification and MRI features. Neuroradiology. 2008;50:301-14.
- [Google Scholar]
- Spinal cord tumors in adults. In: Youmans JR, ed. Neurological Surgery (2nd ed). Philadelphia: WB Saunders; 1984. p. :3196-214.
- [Google Scholar]
- Long-term results of the surgical treatment of 129 intramedullary spinal gliomas. J Neurosurg. 1981;54:323-30.
- [Google Scholar]
- Primary Medullary Tumours of the Spinal Cord and Filum Terminale. Philadelphia, London: WB Saunders; 1964. p. :165-6.
- [Google Scholar]
- MRI features of intramedullary spinal cord ependymomas. J Neuroimaging. 2003;13:346-51.
- [Google Scholar]
- Spinal cord astrocytoma: Pathological and treatment considerations. J Neurosurg. 1995;83:590-5.
- [Google Scholar]
- Tumors of the spinal cord; primary extramedullary gliomas. Surg Gynecol Obstet. 1951;92:183-90.
- [Google Scholar]
- Intradural extramedullary Cauda equina astrocytoma. Case illustration. J Neurosurg. 1999;91:241.
- [Google Scholar]
- Intradural conus and Cauda equina tumours: A retrospective review of presentation, diagnosis and early outcome. J Neurol Neurosurg Psychiatry. 1993;56:69-74.
- [Google Scholar]
- Relation of glioma of leptomeninges to neurological nests. Report of a case of astrocytoma of the leptomeninges. Arch Pathol (Chicago). 1936;21:584-600.
- [Google Scholar]
- Meningiomas, their Classification, Regional Behaviour, Life History and Surgical Results. Springfield: Chalrles C Thomas; 1978. p. :785.
- [Google Scholar]
- Extramedullary astrocytoma of conus region: A short report. Neurol India. 2001;49:97-9.
- [Google Scholar]






