Translate this page into:
Multiple oligodendroglioma with pseudoprogression
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 72 year-old male hospitalized with aphasia, abnormal behavior, and rapidlyprogressive dementia.Magnetic resonance imaging (MRI) enhanced by contrast media demonstrated multiplebrain tumors in left parietal lobe and left paraventricular region. Biopsy was performed,andhistopathological examination and genetical evaluation revealed anaplasticoligodendroglioma. Local radiation 50Gy was given, and Temozolomide via orallyadministered for 42 days. After the chemoradiotherapy, even though the parietal tumorshowed lessening of the size, enlargement of the tumor in the left paraventricularregion was observed, and we considered that phenomenon was pseudoprogression. 5courses of Temozolomide therapy was added, but cerebellar tumor appeared andenlarged with hydrocephalus, and died 1 year and 3 months after the firsthospitalization.
Keywords
Anaplastic
multiple oligodendroglioma
pseudoprogression
temozolomide
Introduction
Although, the incidence of multicentricglioma accounts nearly 2.5% of all gliomas, mostcases are glioblastoma or anaplastic gliomas.[12] Oligodendroglioma cells are detectablein the cerebrospinal fluid in up to 14% of patients, and we recently treated a case of multiple anaplastic oligodendrogliomas, describe the case in detail and discuss the distinction between “multicentric” and “dissemination via cerebrospinal pathways” and the treatment.
Case Report
A 72-year-oldman revealed aphasia, abnormal behavior, and rapidly progressivedementia since October 13, 2009, and hospitalized in our department on Oct. 17, 2009.Magnetic resonance imaging (MRI) enhanced by contrast media demonstrated multiplebrain tumors in left parietal lobe and left paraventricular region [Figure 1a]. Computed tomography (CT) scan showed high density of microbleeding in the left paraventricularregion [Figure 1b]. Biopsy for the tumor in the left parietal tumor was performed. In the permanent section, the hematoxylin and eosin-stained specimen showed that thetissue was composed of cells with clear cytoplasm and with round or irregular nucleushaving dense chromatin (so called honey comb appearance) that existed in between highly proliferative vasculature [Figure 2]. The nuclei had pleomorphism and a variety ofsize, a lot of mitosis were observed. Microvascular proliferation and necrotic findingswere also seen. Occasionally, calcification deposit and microbleeding were observed.Immunocy to chemical study showed positive for glial fibrillary acidic protein, stronglypositive for the olig-2 (oligodendrocyte lineage genes) stain. MIB-1 labeling index was68%. These findings were compatible for anaplastic oligodendroglioma, so geneticalevaluation was performed, showing loss of heterozygosity (co-deletions) in chromosome1p19q. Local brain for the left parietal regionradiotherapy was given to a total dose of 50Gy, in34 fractions of 1.5Gy daily on weekdays from November to December, 2009. At the sametime, Temozolomide of 120mg daily was orally administrated for 42 days. MRI was performed just after these combined chemo- and radiotherapy showed lessening of themass effect in the left parietal tumor, but enlarging the size of the tumor in the left paraventricular region [Figure 3]. We considered that enlargement of the paraventriculartumor was pseudoprogression, as consolidating therapy, Temozolomide of 240mg daily (150mg/m2/day) for 5 days was orally administered for 5 times from February to October 2010 at outpatient clinic. Despite of the high levels of promoterhypermethyltransferase (MGMT) activity, temozolomide is the first linechemotherapeutic agent against anaplastic oligodendroglioma,[34] so we tried temozolomide. But during those period, cerebellar tumor appeared and graduallyenlarged and hydrocephalus was observed [Figure 4]. In October 2010, one cycle of Temozolomidevia intravenous administration was performed and lessening of the masseffect was seen, so the patient was transferred to rehabilitation hospital. In the end ofNovember 2010, the patient's consciousness deteriorated because of the enlargement ofthe 4th ventricle tumor, hydrocephalus and abnormality of serum electrolyte. Theconsciousness of the patient recovered for a while by correcting the electrolyte balance, but consciousness level worsened again, and respiration and clinical state wasdeteriorated, and died on January, 2011.
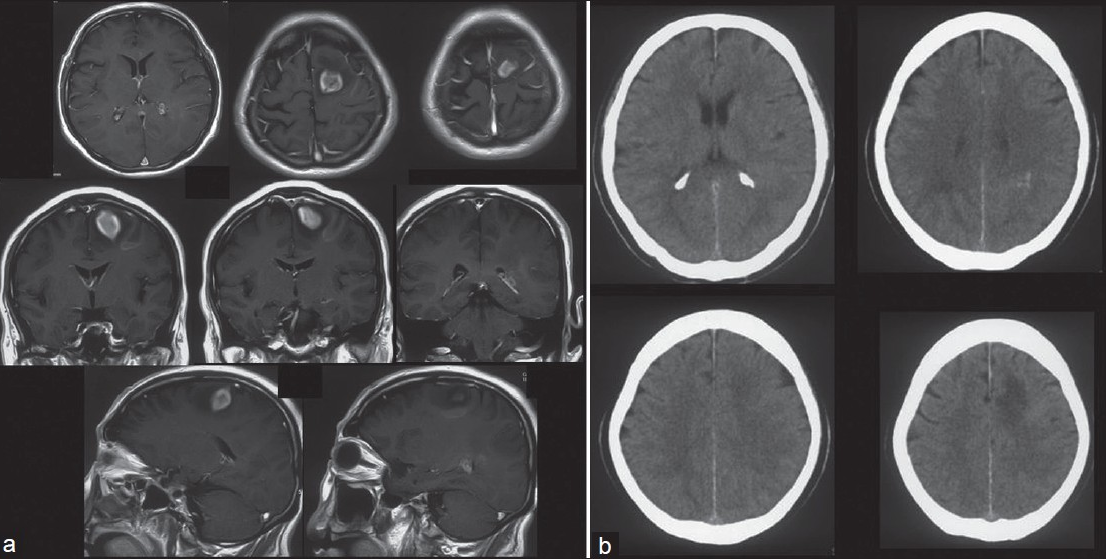
- (a) Magnetic resonance imaging (MRI) enhanced by contrast media obtained atthe first hospitalization.Multiple brain tumors in the left parietal and leftparaventricular region were observed. Upper: axial view, middle: coronal view, lower:sagittal view. (b) Computed tomography (CT) scan at the first hospitalization. Microbleedinginleft paraventricular region was observed

- Histopathological findings of the tumor specimen. The tissue was composed ofcells with clear cytoplasm and with round or irregular nucleus having dense chromatin (so called honey comb appearance). Microvascular proliferation was also observed. Hematoxylin and eosinstained specimen, ×400

- MRI after radiotherapy 50Gy and Temozolomide of 120mg daily for 42 days. Although, lessening of the mass effect of left parietal tumor was observed, enlargementof the paraventricular tumor was seen, which seemed to be pseudoprogression

- MRI performed about 1 year after initial hospitalization. Cerebellar tumorwas observed and enlarged with hydrocephalus. It was not detected in the initial MRI atthe first hospitalization
Discussion
The incidence of multicentricglioma is reported to be approximately 2.5% of all gliomas. Most cases are glioblastoma or anaplastic astrocytoma, and oligodendroglioma is veryrare.[12] Salvati M. et al.reported 25 cases with multicentricgliomas, 11 cases aremulticentricglioblastomas, 6 cases are multicentric anaplastic astrocytomas, and othercases are combinations of glioblastomas, anaplastic astrocytomas, and low gradegliomas, and no oligodendrogliomas were found.[5]
We considered whether our patient's tumor was multicentric or metastatic. Solomon etal. stated a clear distinction must be made, in cases of multiple tumors, amongdissemination via cerebrospinal pathways, direct extension across commissures,satellitosis, and true multicentrism.[6] Multicentric tumors are widely separated, arisingin different lobes or hemispheres, which is not readily explained by one of the pathwaysmentioned above.In our case, the 4th ventricle tumor which arose about 1 year afterinitial treatment might have been a metastasis via cerebrospinal fluid, although one ofthe multiple sites cannot be dismissed entirely. However, left parietal tumor and lefttrigonal area tumor were found at the same time, and those two tumors were separated,arising in the distinct sites, and were not explained either by the dissemination viacerebrospinal pathways or direct extensions, so we considered those tumors weremulticentric.The pathogenesis of multicentricgliomas is unknown.The most quoted hypothesis is the two-step process reported by Willis.[7] In the firststage a large area of the brain undergoes neoplastic transformation, while in the secondstage one or more foci of tumor proliferation develop within the affected area, givingorigin to separate lesions. The pathogenesis of multicentricglioma include theembryonal rest theory and the two-stage theory, but Zülch pointed out the metastasisvia an unknown pathway.[8]
Multicentricgliomas are characterized by rapid progression, which may be related tothe fact that they tend to exhibit malignant features on histology, this fact is also validfor the oligodendrogliomas. The course of our case from initial diagnosis to death was 1year and 3 months, despite of the combined chemoradiotherapy.In our case, the 4thventricle portion tumor which appeared about one year after the initial treatment andwas not detected in the MRI taken at initial hospitalization, might be the metastasis viacerebrospinal fluid, as histological type of malignant oligodendroglioma is a risk factor of cerebrospinal fluid dissemination.[9]
Finally, the tumor in the left paraventricular region showed progression even just after the temozolomide treatment, and we presumed it was pseudoprogression, because in the first 6 months of post-chemoradiotherapy period, showed a high incidence of pathologically confirmed pseudoprogression associated with treatment-related necrosiswithout viable tumor cells. Various imaging techniques including MR spectroscopy havebeen studied but neither has been found to be powerful to identify pseudoprogression,and unfortunately, the diagnosis of pseudoprogression still depends on pathologicexamination.The disruption of blood-brain barrier with the resultant observation of an earlyradiologic increase in contrast enhancement at MRI, which may falsely mimic trueprogression,[10] and this fact made the treatment of this case more complicated.
Source of Support: Nil
Conflict of Interest: None declared
References
- Phase II study of first-line chemotherapy with temozolomide in recurrentoligodendroglial tumors: The European Organization for Research and Treatment of Cancer Brain Tumor Group Study 26971. J ClinOncol. 2003;21:2525-8.
- [Google Scholar]
- MGMTgene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352:997-1003.
- [Google Scholar]
- Multicentricgliomas: Our experience in 25 patients and critical review of the literature. Neurosurg Rev. 2003;26:275-9.
- [Google Scholar]
- Multicentricgliomas of the cerebral andcerebellar hemispheres. J Neurosurg. 1969;31:87-93.
- [Google Scholar]
- Pathology of tumors. London: Butterworth; 1960. p. :121-2.
- Brain tumors. In: Their biology and pathology, 116-20, 240-58 (1st ed). New York: Springer; 1957. p. :74-6.
- [Google Scholar]
- Dissemination of supratentorial malignant gliomasvia the cerebrospinal fluid in children. Neurosurgery. 1992;30:64-71.
- [Google Scholar]
- Pseudoprogression in patientswithglioblastomamultiforme after concurrent radiotherapy and temozolomide. Am J ClinOncol. 2012;35:284-9.
- [Google Scholar]






