Translate this page into:
Epidermoid cyst causing hemifacial spasm epidermoid cyst in cerebellopontine angle presenting with hemifacial spasm
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hemifacial Spasm (HS) occurs idiopathically or secondary to the lesions compressing the root exit zone of the facial nerve symptomatically. Symptomatic HS is generally due to vascular compression. We report on a 23-year-old male with right sided HS for a month. Magnetic resonance imaging (MRI) of the brain revealed a well-demarcated epidermoid cyst in the right cerebellopontine cistern. It was hypointense on T1-weighted imaging, hyperintense on T2-weighted imaging without contrast enhancement, hyperintense on DWI, and slightly hypointense on ADC relative to the brain. Although it caused shifting of the pons and medulla to the left side and compression of the right cerebellar peduncles and fourth ventricle, the sole symptom of the patient was HS. Clinicians are advised to request MRI/scan for brainstem lesions from the patients with HS. Epidermoid cysts in cerebellopontine cistern may present with HS as the sole symptom.
Keywords
Cerebellopontine angle
epidermoid cyst
hemifacial spasm
Introduction
Hemifacial Spasm (HS) is a disorder characterized by involuntary contractions of the muscles (spasms) on one side of the face (hemifacial). It is generally the result of vascular loop compression of the facial nerve at its root exit zone from the brainstem. It may also be associated with other organic lesions like tumors, aneurysms, vertebral artery dolichoectasia, cerebral infarctions, multiple sclerosis plaques, etc. Although the occurrence of tumor compression causing HS was previously recognized, cerebellopontine angle epidermoid cysts have rarely been described.[12]
Epidermoids are one of the rare benign, congenital, developmental tumors, usually located in the cerebellopontine angle and parasellar regions. They cause various symptoms, especially ones in the cerebellopontine angle. These symptoms could be associated with cerebellar signs (ataxia), increased intracranial pressure (headache, nausea, vomiting) or cranial nerve disturbances (hearing loss or tinnitus, facial nerve palsy, trigeminal neuralgia, etc.). Herein, we report on a patient with a cerebellopontine angle epidermoid cyst having HS as the sole presenting complaint.
Case Report
A 23-year-old male was admitted to the hospital with the complaint of intermittent twitching of the muscles on the right side of his face. First, the muscles over the right side of his mouth and lower eyelid were affected 1 month before being admitted to the hospital. Then, it spread to all of the muscles on the right side of his face. Upon admission to the hospital, these involuntary spasms occurred repetitively within 10–15 minute intervals for a day. The spasms were also observed during physical examination [Figure 1]. There was no alteration of consciousness or associated involuntary movements of any other body parts of his body during the spasms. The neurological examination was normal. He had no history of convulsion, neurotrauma or developmental delay in childhood. There was no family history of neurological disease.
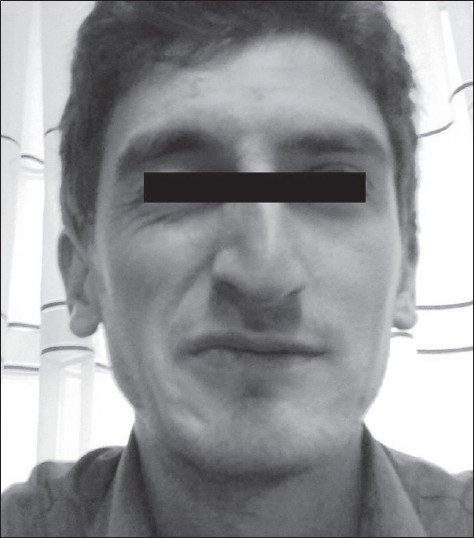
- Hemifacial spasm on right side of our patient's face
Magnetic resonance imaging (MRI) of the brain was requested. It revealed a well-demarcated cyst (hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging without contrast enhancement) in the right cerebellopontine cistern. This cyst had diameters of 28 mm and 25 mm in its largest portion on transverse images. It caused shifting of the pons and medulla to the left side and compression of the right cerebellar peduncles and fourth ventricle. To differentiate between the epidermoid cyst and the arachnoid cyst, diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) mapping were done. It was hyperintense on DWI and slightly hypointense on ADC relative to the brain [Figure 2].

- (a) Coronal, (b) saggital, (c) axial T1-weighted, and (d) axial T2-weighted MRI scans of the brain revealing a well-demarcated epidermoid cyst, which is hypointense on T1-weighted images and hyperintense on T2-weighted images without contrast enhancement in the right cerebellopontine cistern. The cyst appears (e) hyperintense on DWI and (f) slightly hypointense on ADC relative to the brain
The results of the laboratory tests including hemogram, biochemical tests, and tumor markers were normal. Audiogram showed normal hearing patterns. EEG results were also normal. The patient was informed about his disease and advised to have neurosurgery treatment option. He was operated with the retrosigmoid (lateral suboccipital) approach in an external neurosurgery department. The diagnosis was also confirmed histologically. Only a slight hypophonia was noted during the outpatient clinic visit 15 days after the operation. HS completely disappeared after the surgery. The patient remains asymptomatic during 18 months postoperative follow-up.
Discussion
HS is a clinical symptom consisting of brief clonic jerking movements of the facial muscles, usually beginning in orbicularis oculi and then spreading to the other muscles innervated by facial nerve. HS is frequently caused by vascular compression at the root exit zone of the facial nerve. Besides compressive neurovascular structures, it can also be caused by other organic lesions like tumors. The incidence of tumor-related HS is very low (0.3–2.5%).[3–6] The main tumors found in cistern of the cerebellopontine angle are vestibular schwannomas, meningiomas, and epidermoid cysts. The epidermoids represent 0.2–1.8% of all primary intracranial tumors, and approximately 5% of all masses encountered in cerebellopontine angle.[7]
HS is a hyperactive dysfunction of facial nerve, which is generated at the facial root exit zone at pontomedullary junction. It usually occurs when the structural lesions compress root exit zone and atypical neuronal signal is generated and conducted to facial muscles.[8] As for HS induced by benign tumors in many cases, as in our patient, previous researchers suggested that the vascular compression under the tumor is the main cause of the HS.[910]
Typical MRI appearance of an epidermoid tumor is hypo to slight hyperintense on T1W images, iso to hyperintense on T2W images, and hyperintense on DWI.[1112] Arachnoid cysts and schwannomas also appear as hyperintense on T1W images and hyperintense on T2W images. As the schwannomas show contrast enhancement and follow the anatomic course of the nerve, it could be easily recognized. However, DWI is an important technique to differentiate epidermoid cysts and arachnoid cysts. In case of an arachnoid cyst, DWI reveals a hypointense lesion, which is isointense to CSF. However, epidermoid cysts appear hyperintense on DWI as in our case.[12]
Clinicians need to be aware that patients with HS should be scanned for brainstem lesions. MRI studies are essential to detect the vascular structures running adjacent to the root exit zone that might distort the facial nerve and compress the brain stem around the root exit zone, and to exclude other organic causes like tumors, MS plaques or cystic lesions. As in our case, an epidermoid cyst in cerebellopontine cistern, compressing the pons, which contains the nuclei and root exit zone of the facial nerve, may present with HS as the sole symptom.
Source of Support: Nil
Conflict of Interest: None declared
References
- Hemifacial spasm due to posterior fossa tumors: The impact of tumor location on electrophysiological findings. ClinNeurolNeurosurg. 1998;100:104-11.
- [Google Scholar]
- Cerebellopontine angle epidermoids presenting with cranial nerve hyperactive dysfunction: Pathogenesis and long-term surgical results in 30 patients. Neurosurgery. 2002;50:276-85. discussion 285-6
- [Google Scholar]
- Microsurgical treatment for 55 patients with hemifacial spasm due to cerebellopontine angle tumors. Neurosurg Rev. 2010;33:335-9. discussion 339-40
- [Google Scholar]
- Hemifacial spasm due to tumor, aneurysm, or arteriovenous malformation. SurgNeurol. 1992;38:204-9.
- [Google Scholar]
- Bilateral hemifacial spasm: A series of 10 patients with literature review. Parkinsonism RelatDisord. 2008;14:154-6.
- [Google Scholar]
- Hemifacial spasm due to posterior fossa tumors: The impact of tumor location on electrophysiological findings. ClinNeurolNeurosurg. 1998;100:104-11.
- [Google Scholar]
- MR imaging of epidermoids at the cerebellopontine angle. MagnReson Med Sci. 2003;2:109-15.
- [Google Scholar]
- Microvascular decompression of the facial nerve for the treatment of hemifacial spasm: Preoperative magnetic resonance imaging related to clinical outcomes. ActaNeurochir(Wien). 2000;142:901-6. discussion 907
- [Google Scholar]
- Hemifacial spasm associated with an ependymal cyst in the cerebellopontine angle. Case report. J Neurosurg. 2002;97:482-5.
- [Google Scholar]
- Hemifacial spasm caused by epidermoid tumor at cerebello pontine angle. J Korean NeurosurgSoc. 2009;45:196-8.
- [Google Scholar]
- Typical and atypical MR imaging features of intracranial epidermoid tumours. AJR Am J Roentgenol. 1997;169:883-7.
- [Google Scholar]
- Unusual lesions of the cerebellopontine angle: A segmental approach. Radiographics. 2001;21:419-38.
- [Google Scholar]






