Translate this page into:
Spinal epidural angiolipoma: A rare cause of spinal cord compression
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Spinal epidural angiolipomas are rare, benign tumors composed of mature lipocytes admixed with abnormal blood vessels. Only 128 cases of spinal epidural angiolipomas have been reported in literature till now. Spinal angiolipomas are predominantly located in the mid-thoracic region. We report a case of dorsal epidural angiolipoma in a 56-year-old male who presented with paraparesis and was diagnosed to have D4-5 epidural angiolipoma. Total surgical excision of the epidural angiolipoma was done and his paraparesis gradually improved.
Keywords
Angiolipoma
spinal epidural tumor
spinal tumor
Introduction
Spinal epidural angiolipomas are uncommon, benign tumors accounting for 0.04–1.2% of spinal axis tumors and 2–3% of extradural spinal tumors.[12] Angiolipomas are composed of both mature fatty tissue and abnormal vascular elements. They are commonly located in the subcutaneous region of the trunk and extremities. Location of angiolipoma in spine is rare. The commonest location in spine is dorsal epidural region,[1] followed by lumbar region. All angiolipomas show iso- or hyperintensity on T1-weighted images and hyperintensity on T2-weighted images of magnetic resonance imaging (MRI) and most lesions enhance with gadolinium administration.[34] Angiolipomas can be categorized into two subtypes: non-infiltrating and infiltrating.[5] Treatment of spinal epidural angiolipomas is by total surgical excision.
Case Report
Presentation
A 56-year-old male presented with history of numbness below the chest of 3 months duration and heaviness in bilateral lower limbs of 2 months duration and difficulty in walking for 2 months. On clinical examination, multiple subcutaneous lipomas were present. There was decreased sensation below D5 dermatome and spasticity in both lower limbs with hyperreflexia. MRI of dorsal spine revealed a sausage-shaped homogenous lesion at D4-5 level. The lesion was in epidural plane and was compressing the spinal cord anteriorly. It was showing hypointensity on T1-weighted images and hyperintensity on T2-weighted images of MRI [Figure 1a–c].
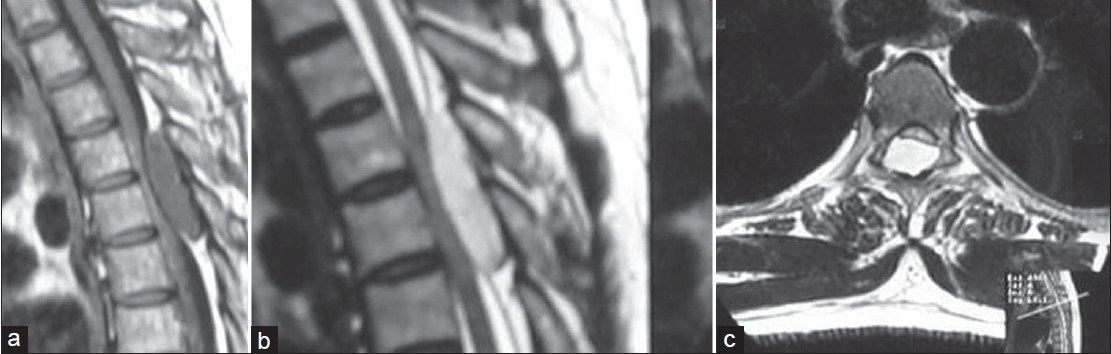
- (a) T1-weighted image of MRI dorsal spine showing hypointense epidural lesion at D4-5 level, compressing the spinal cord; (b) T2-weighted images of MRI dorsal spine showing hyperintense epidural lesion; (c) T2-weighted MRI axial images demonstrating severe cord compression
Surgery
D4-6 laminectomy was done and a reddish vascular epidural lesion of size 2 × 1 cms was seen compressing the cord [Figure 2]. Total excision of the epidural lesion was done.

- Intraoperative photograph showing epidural angiolipoma
Pathology
Pathological examination of the resected lesion showed mature adipose tissue and abundant vascular channels, the caliber of which was variable, ranging from nearly capillary size to cavernous, but mostly several times larger than the fat cells [Figure 3]. There was no cytological atypia or structural abnormalities in the vascular channels. Lipoblasts were not seen.

- Histopathology of angiolipoma showing admixture of mature adipose tissue and vascular elements (H and E, ×200)
Follow-up
Postoperative course was uneventful. Paraparesis gradually improved. Neurological examination at 60 months follow-up revealed full power in the legs with normal tone and no hyperreflexia.
Discussion
Spinal epidural angiolipomas are rare, benign tumors, with only 128 cases reported in the literature till now.[126–12] The most common location of angiolipomas is in the soft tissues of the extremities, trunk, or neck. Berenbruch first described a case of spinal angiolipoma in 1890.[13] In 1960, Howard and Helwig established angiolipoma as a clinicopathological entity containing vascular and mature adipose elements.[14] Location in spinal canal is rare and the commonest location in spinal canal is in dorsal epidural region. Spinal epidural angiolipomas commonly occur in adults in the fourth and fifth decades and have female preponderance.[12] Location in lumbar spine is rare.[11] Location in spinal intramedullary region and intracranially has been rarely reported.[1516]
MRI is the investigation of choice in diagnosing spinal angiolipoma.[12] Angiolipomas are iso- or hyperintense on T1-weighted images and variable in T2-weighted images of MRI, but usually hyperintense. The fat component is typically hyperintense on T1-weighted images and hypointense on T2-weighted images. The degree of central hypointensity on T1-weighted images is predictive of the degree of vascularity.[317] In the current case, hypointensity on T1-weighted images correlated with increased vascularity within the spinal angiolipoma. They are subdivided into two types: non-infiltrating and infiltrating.[25] The non-infiltrating type of spinal angiolipoma is more common and is usually well encapsulated and generally arises from the posterior epidural space. Spinal infiltrating angiolipomas are generally located in the anterior epidural space and can invade the vertebral body.[212] The common clinical presentations of spinal epidural angiolipomas are progressive paraparesis, back pain without radiculopathy, lower extremity sensory changes, and hyperreflexia. Pregnancy can aggravate the symptoms probably because of impaired spinal venous drainage or hormonal changes. Sudden neurological deterioration can occur due to tumor thrombosis or hemorrhage.[6] Non-infiltrating angiolipomas are well defined and separate from the surrounding tissue and can usually be easily removed by laminectomy. In case of infiltrating spinal angiolipomas, wider resection is advised.[1] Most of the patients have good postoperative outcome after surgical excision of spinal angiolipomas in spite of severe preoperative neurological deterioration. Adjuvant radiation has not been recommended to patients with this benign pathological entity, since the prognosis is very good even in the infiltrating variety. Recurrence after surgery is rare and only one case has been reported.[18]
Source of Support: Nil
Conflict of Interest: None declared
References
- Spinal angiolipoma: Case report and literature review. J Spinal Cord Med. 2008;31:315-8.
- [Google Scholar]
- Spinal extradural angiolipoma: Report of two cases and review of the literature. Eur Spine J. 2009;18:324-35.
- [Google Scholar]
- MR imaging of an infiltrating spinal epidural angiolipoma. AJNRAm J Neuroradiol. 2003;24:1008-11.
- [Google Scholar]
- Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer. 1974;34:720-7.
- [Google Scholar]
- Sudden onset of paraplegia caused by hemorrhagic spinal epidural angiolipoma. A case report. Eur Spine J. 2008;17:296-8.
- [Google Scholar]
- Thoracic epiduralangiolipoma with bilateral multilevel extraspinal extensions: A rare entity. Neurol India. 2011;59:134-6.
- [Google Scholar]
- Spinalangiolipoma in a pregnant woman presenting with acute epidural hemorrhage. J ClinNeurosci. 2011;18:849-51.
- [Google Scholar]
- Lumbar spinal extradural angiolipoma: Case report and review of literature. J Korean NeurosurgSoc. 2008;44:265-7.
- [Google Scholar]
- Ein fall von multiplen angiolipomen konnbintert mit eniem angiom des rukenmarks. Tubingen 1890
- [Google Scholar]
- Radiological and histological findings in spinal intramedullary angiolipoma. Neuroradiology. 1999;41:584-7.
- [Google Scholar]
- Intracranial angiolipoma as cause of subarachnoid haemorrhage. Case report and review of the literature. Neuroradiology. 2005;47:91-6.
- [Google Scholar]
- Epidural lipoma producing spinal cord compression.Report of two cases. J Neurosurg. 1974;41:100-3.
- [Google Scholar]






