Translate this page into:
Spontaneous intracerebral hemorrhage: Clinical and computed tomography findings in predicting in-hospital mortality in Central Africans
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background and Purpose:
Intracerebral hemorrhage (ICH) constitutes now 52% of all strokes. Despite of its deadly pattern, locally there is no clinical grading scale for ICH-related mortality prediction. The first objective of this study was to develop a risk stratification scale (Kinshasa ICH score) by assessing the strength of independent predictors and their association with in-hospital 30-day mortality. The second objective of the study was to create a specific local and African model for ICH prognosis.
Materials and Methods:
Age, sex, hypertension, type 2 diabetes mellitus (T2DM), smoking, alcohol intake, and neuroimaging data from CT scan (ICH volume, Midline shift) of patients admitted with primary ICH and follow-upped in 33 hospitals of Kinshasa, DR Congo, from 2005 to 2008, were analyzed using logistic regression models.
Results:
A total of 185 adults and known hypertensive patients (140 men and 45 women) were examined. 30-day mortality rate was 35% (n=65). ICH volume>25 mL (OR=8 95% CI: 3.1-20.2; P<0.0001), presence of coma (OR=6.8 95% CI 2.6-17.4; P<0.0001) and left hemispheric site of ICH (OR 2.6 95% CI: 1.1-6; P=0.027) were identified as significant and independent predictors of 30-day mortality. Midline shift > 7 mm, a consequence of ICH volume, was also a significant predictor of mortality. The Kinshasa ICH score was the sum of individual points assigned as follows: Presence of coma coded 2 (2 × 2 = 4), absence of coma coded 1 (1 × 2 = 2), ICH volume>25 mL coded 2 (2 × 2=4), ICH volume of ≤25 mL coded 1(1 × 2=2), left hemispheric site of ICH coded 2 (2 × 1=2), and right hemispheric site of hemorrhage coded 1(1 × 1 = 1). All patients with Kinshasa ICH score ≤7 survived and the patients with a score >7 died. In considering sex influence (Model 3), points were allowed as follows: Presence of coma (2 × 3 = 6), absence of coma (1 × 3 = 3), men (2 × 2 = 4), women (1 × 2 = 2), midline shift ≤7 mm (1 × 3 = 3), and midline shift >7 mm (2 × 3 = 6). Patients who died had the Kinshasa ICH score ≥16.
Conclusion:
In this study, the Kinshasa ICH score seems to be an accurate method for distinguishing those ICH patients who need continuous and special management. It needs to be validated among large African hypertensive populations with a high rate of 30-day in–hospital mortality.
Keywords
Clinical and neuroimaging data
intracerebral hemorrhage
predictors of mortality
sub-Saharan Africa
Introduction
Stroke is a leading cause of mortality and a long-term disability with an enormous economic burden in developed countries[1–3] and Democratic Republic of the Congo (DRC),[4–9] a poor and very indebted country. In 1988, computed tomography (CT) equipment was introduced in DRC. This resulted in a rapid advance of epidemiology of stroke among central Africans.[4–9]
Spontaneous intracerebral hemorrhage (ICH) is the deadliest and least treatable complication of stroke despite sophisticated management of the disease in developed countries.[10–12] There is no therapy which reduces risk of mortality or long-term disability after ICH.[3]
Various and complex prognosis models have been reported from many settings out of Africa.[13–22] In this context with low rates of ICH,[2324] the original scores of Hemphill et al.[19] have been tested in geographically and culturally different communities.[20–22] In our current clinical practice, the CT scan shows that hemorrhagic stroke type (52%)/ischemic type (48%) ratio is closed to 1.[9] However, data on prognosis of various anatomical sites and volume of ICH, cerebral hemisphere involved and shifts of midline from CTscan, demographic, lifestyle, and clinical variables are not available in Kinshasa, DRC.
The first objective of this study was to develop a risk stratification scale (Kinshasa ICH score) by assessing the strength of independent predictors and their association with in-hospital 30-day mortality. The second objective of the study was to create a specific local and African model for ICH prognosis.
Materials and Methods
Institutional Review Board approval and informed consent of patients or their representatives were obtained for all aspects of this study. This short prospective study was carried out at the LOMO Medical Centre, Kinshasa University Hospital, and Gombele Medical Centre, Kinshasa, DRC, between January 2005 and December 2008. There were 185 adults and known hypertensive patients, including 140 men and 45 women (sex ratio of 3 men:1 woman). Each center has an intensive care unit for acute cardiovascular event with 8 beds for Lomo Medical Centre, 10 beds for Kinshasa University hospital, and 5 for Gombele Medical Centre.
Patients with hemorrhage secondary to brain tumors, trauma, hemorrhagic transformation of cerebral infarction, anticoagulant therapy, aneurismal, or vascular malformations were excluded. CT examinations at admission were performed within the 48 h of onset, using the same Toshiba SDCT Xpress/GX machine (Toshiba, Tokyo, Japan) installed at the Gombele Medical Centre. CT information was evaluated at the coordinating Centre of Lomo Medical by the single investigator (LTM). Topographic classification of the hematoma was defined according to Castillo et al.[25] ICH volume was calculated using the ABCs of measuring ICH volume method of Kothari et al.[26] The hemisphere involved and the midline shift were also noted. The midline shift was defined as the displacement of the septum pellucidum, being a reproducible landmark, in relation to the midline, and was registered in millimeters as described by “The American Association of Neurological Surgeons, 2000”.[27]
Other recorded information included sex, age, tobacco use, coma, alcohol intake, treatment, and the status at discharge (death or survivorship).
“Poor” Glasgow Coma Scale (GCS) score on admission was defined as 3-8 of a top score of 15, and the Oxfordshire Community Stroke Project (OCSP) clinical classification of stroke.[2829]
ICH, a spontaneous bleeding into the brain parenchyma, was hyperdense on CT scan relative to gray matter [Figure 1]. Patients were divided into ICH volume ≥25 mL or ICH volume <25 mL median value in the study population. The midline shift by ≥7 mm (median value) on cranial CT was reported. Standardized treatment of ICH included nursing, prevention, and treatment of raising intracerebral pressure as recommended by the AHA Scientific Statement,[10] antioxidant (Vitamin C), and piroxicam. In these patients facing demographic transition, age was defined by adults aged ≤60 years versus Elderly aged >60 years. Classical cardiovascular risk factors considered were cigarettes smoking (regular vs. non-smoking, number of cigarettes/day), and alcohol intake (abstinence, moderate, and excessive alcohol intake defined by 1-3 drinks and ≥3 drinks/day, respectively).
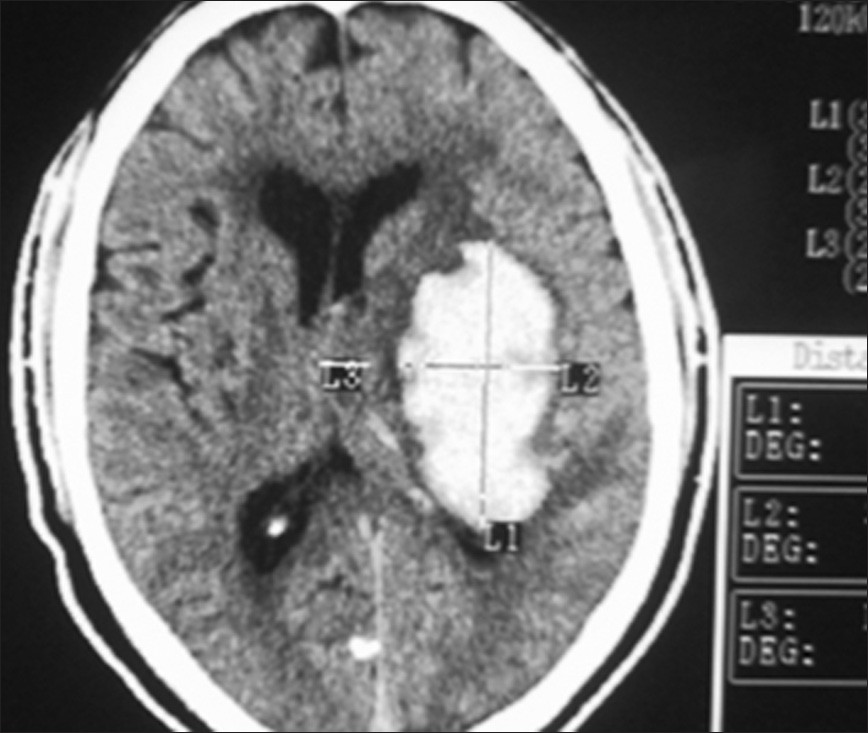
- CT scan image of the hyperdense lesion (Intracerebral hemorrhage)
Statistical analysis
Univariable statistical analysis
Comparisons of proportions (%) for categorical variables between groups (died vs. survived) were made using the Chi-square test. Continuous variables were expressed as means±standard deviations (SD), and compared using the Student t-test or the Mann-Whitney U test as appropriate.
Multivariable analysis
Logistic regression analysis was used to find the best predictive model of in-hospital mortality (30 day – case fatality) as the dependent variable. The variables that were significantly related to in-hospital mortality in univariate analysis were entered within the logistic regression model using a forward stepwise selection. The maximum like hood approach was used after adjusting for confounding factors and identifying independent predictors of mortality.
Significant level was defined for the tolerance level at P<0.05. Statistical analysis was performed using SPSS software version 16 (SPSS Inc., Chicago, IL, USA).
Results
Patients and follow-up
Out of the 185 known hypertensive patients with ICH [Figure 1] and followed-up over a 30-day period, 140 were men (75%) and 45 women (25%: Sex ratio of 3 men:1 woman. The mean age of patients was 53.7 ± 9.2 years (range: 33 years and 77 years). Table 1 presents the profile of cardiovascular, clinical, and neurological imaging characteristics with reference to sex.

Out of the 185 studied patients, 68 died (36.8%). Table 2 presents the comparison of characteristics according to outcome. Younger age, higher levels of ICH volume and midline shift, left hemispheric side, presence of coma, and males were more observed in fatal cases than non fatal cases. The J-shaped relationship between in-hospital mortality and ICH volume was also significant (P<0.0001) [Figure 2].


- Relationship between intra-hospital and intracerebral hemorrhage volume
Independent predictors of mortality
Four logistic regression models were performed to identify independent and significant predictors of mortality. Adjusted for sex, moderate alcohol intake, and hemispheric involvement (Model 1), only the presence of coma (OR=2.5 95% CI: 1.3-5; P=0.005) and age <60 years (OR=3.3 95% CI: 1.6-6.5; P<0.0001) were identified as significant and independent predictors of mortality.
Adjusted for all univariate and significant cardiovascular risk factors, midline shift >7 mm, infratentorial origin, deep location of ICH (Model 2), the significant and independent predictors of mortality were ICH >25 mL, the presence of coma, and left hemispheric site of hemorrhage [Table 3].

The Kinshasa ICH score was the sum of individual points assigned as follows: Presence of coma coded 2 (2 × 2 = 4), absence of coma coded 1 (1 × 2 = 2), ICH volume ≥25 mL coded 2 (2 × 2 = 4), ICH volume of <25 mL coded 1 (1 × 2 = 2), left hemispheric site of ICH coded 2 (2 × 1 = 2), and right hemispheric site of hemorrhage coded 1 (1 × 1 = 1). All patients with the Kinshasa ICH score <7 survived and the patients with a score ≥7 died (Model 2).
In considering sex influence (Model 3), points were allowed as follows: Presence of coma (2 × 3 = 6), Absence of coma (1 × 3 = 3), men (2 × 2 = 4), women (1 × 2 = 2), midline shift <7 mm (1 × 3 = 3), and midline shift >7 mm (2 × 3 = 6) [Table 4]. Patients who died had Kinshasa ICH score ≥16 versus Kinshasa score ≥16 points for surviving patients.

Discussion
This study was designed to develop a risk stratification scale (the Kinshasa ICH score) using weighting of independent predictor strength of their association with in-hospital 30-day mortality. The study population included black hypertensives from DRC, the poorest sub-Saharan country despite the potential of minerals from DRC. The present data confirmed the increasing rates of important risk factors for stroke such as hypertension, type 2 diabetes mellitus (T2DM) and cigarette smoking in Africa.[30–32] This is the first study, as far as we are aware, to have included the neurological imaging findings among predictive factors of ICH-related mortality in a sub-Saharan African setting. The present findings about ICH-related outcome are consistent with high rates of coma and in-hospital mortality worldwide.[6733–41] The observed 35% mortality rate was in the interval of 20.2-50% mortality rates reported in the literature.[3941–43]
Contrary to well-established deleterious effect of older age[44–47] in predicting ICH-related mortality in developed countries, the present study showed a significant and univariate association between younger age <50 years and ICH-related mortality. This discrepancy may be explained by the epidemiologic/demographic transition and smoking: Young adults smoke and experience atherosclerotic diseases than children and elderly (Longo-Mbenza, unpublished data). There was no risk of mortality in patients consuming moderate alcohol intake as reported elsewhere.[48] Our findings confirm the predictive role of coma in stroke and ICH mortality.[4849] Coma with hyperventilation induces dehydration which is exacerbated during rainy season of tropical climate of DRC.[67] The majority of our patient with ICH had hypertension which is often unknown or not controlled in Africans with stroke.[6] However, the impact of T2DM, smoking, and males on mortality in univariate analysis disappeared in multivariate analysis. The literature recognizes T2DM, smoking, hypertension, and males as predictive factors of ICH-related mortality.[36] Using logistic regression models, our results support the validity of neuroimaging features in predicting overall 30-day mortality in these black Africans with ICH as reported in developed countries.[1920224849]
The present findings confirmed the literature reports[1948–51] that ICH volume is a significant and independent predictor of mortality. ICH volume ≥ 25 mL was the most important and independent predictor of mortality as reported by other studies.[1940414346] This may be explained by the elevated intracranial pressure and cerebral edema associated with the hemorrhagic volume.[52]
The median volume cut-off point ≥25 mL used in this study was different from those of 10 mL[49] 30 mL,[19] 40 mL,[52] and 60 mL[46] used by other authors. However, there was a curvilinear J-shaped relationship between mortality and quartiles of ICH volume. Thus, both lowest and highest ICH volumes were identified for higher risk of mortality, respectively. The midline shift was also identified as a significant and independent predictor of mortality together with males and presence of coma. The midline shift is a consequence of ICH volume.
Among the rest of neuroimaging features such as hemispheric involved by ICH, infratentorial or supratentorial origin of the ICH, and deep or lobar site of the ICH, only left hemispheric location was identified as a significant and independent predictor of mortality in these black people. It seems difficult to explain our findings which contrast with studies from developed countries identifying intra-ventricle and infratentorial origin of ICH as predictors of mortality.[194445] We found that the ICH in black African is often located on the left hemisphere as did Obajimi et al. in Ghana.[49]
Clinical implications
These findings will be useful to distinguish those ICH patients who need continuous and special management. Indeed, ICH scale has proven to be reliable in predicting 30-day mortality in different settings and clinical conditions.[2022] Younger patients and patients with coma might be the potential targets for special ICH treatment. The present ICH score may help to improve the selection of ICH patients for care intensive Units or clinical trials.[50] Its validation is necessary for a long period and other populations.
Limitations
There are some potential limitations of the present ICH score. First, this study was limited to a short time of follow-up and to the variables that were available in this limited resources setting. These variables did not include laboratory and other clinical predictor of mortality following ICH such as time of onset, apolipoproteins, and other factors which may lead to self-fulfilling prophecies.[5152] Second, these findings may be influenced by various levels in assessment and treatment after ICH hospital admission. Also, repeated CT examinations were not done routinely within a few days of admission or performed when a clinical deterioration was noticed. Despite these potential limitations, the present study provides a robust but simple tool for predicting 30- day mortality of ICH patients. CT machines should be available in each sub-Saharan reference hospital.
Conclusion
In conclusion, the Kinshasa ICH score appears to strongly predict in-house 30-day mortality; however, it needs to be validated in large hypertensive populations. Appropriated management in ICH patients is urgent to avoid the observed high case fatality.
Source of Support: Kinshasa University School of Medicine and Hospital, Kinshasa, DR Congo and Lomo Medical Clinic, Kinshasa, DRC
Conflict of Interest: The authors declare that they have no competing interests.
References
- Mortality by cause for eight regions of the world: Global burden of disease study. Lancet. 1997;349:1269-76.
- [Google Scholar]
- Evaluation tomodensitométrique des accidents vasculaires cérébraux à Kinshasa, Zaire 1993:166-8.
- CT scan features of stroke in the urban black African. Afr J Neuro Sci. 1994;13:29-30.
- [Google Scholar]
- Hematocrit and stroke in black Africans under tropical and meteorological influence. Ann Med Interne (Paris). 1999;150:171-7.
- [Google Scholar]
- Predictor of stroke associated mortality in Africans. Rev Epidemiol Santé Publique. 2000;48:31-9.
- [Google Scholar]
- Bases physiologiques de la prise en charge de l’œdème erebral lié à l’accident erebral ischémique. Congo Méd. 2006;4:837-42.
- [Google Scholar]
- Rates of predictors of stroke-associated case fatality in black central Africans patients. Cardiovasc J Afr. 2008;19:2.
- [Google Scholar]
- Guidelines for management of spontaneous intracerebral hemorrhage: A statement for healthcare professionals from a special writing group of the stroke Council, American Heart Association. Stroke. 1999;30:905-15.
- [Google Scholar]
- Early surgery versus conservative treatment in patient with spontaneous intracerebral heamatoma in the International Surgical trial in intracerebral hemorrhage (STICH): A randomized trial. Lancet. 2005;365:387-97.
- [Google Scholar]
- Volume of ventricular blood is a determinant of outcome in supratentorial intracerebral hemorrhage. Crit Care Med. 1999;27:617-21.
- [Google Scholar]
- Hydrocephalus is a determinant of early mortality in putaminal hemorrhage. Stroke. 2000;31:2157-62.
- [Google Scholar]
- Pronostic factor in a serie of 185 consecutive spontaneous supratentorial intracerebral hematoma. Br J Neurosurg. 2000;16:355-61.
- [Google Scholar]
- Multivariate analysis of predictors of hematoma enlargement in spontaneous intracerebral hemorrhage. Stroke. 1998;29:1160-6.
- [Google Scholar]
- Risk factors for impaired outcome after spontaneous intracerebral hemorrhage. Arch Neurol. 1995;52:1193-200.
- [Google Scholar]
- The ICH score: A simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32:891-7.
- [Google Scholar]
- Predicting mortality in spontaneous intracerebral hemorrhage can modify to the original score improve the prediction? Stroke. 2006;37:1038-44.
- [Google Scholar]
- Grading scale for prediction of outcome in primary intracerebral hemorrhage. Stroke. 2007;38:1641-4.
- [Google Scholar]
- Intracerebral hemorrhage more than twice as common as subarachnoid hemorrhage. J Neurosurg. 1993;78:188-91.
- [Google Scholar]
- Projected number of stroke by subtype in the year 2050 in the United State. Stroke. 1998;29:322.
- [Google Scholar]
- The American Association of Neurological Surgeons. The Joint Section on Neurotrauma and Critical Care. Computed tomography scan features. Review. J Neurotrauma. 2000;17:597-627.
- [Google Scholar]
- Validation of a clinical classification for subtypes of acute cerebral infarction. J Neurol Neurosurg Psychiatry. 1994;57:1173-9.
- [Google Scholar]
- Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991;337:1521-6.
- [Google Scholar]
- Changing causes of death in a West African town: 1942-1997. Bull World Health Org. 2001;79:133-41.
- [Google Scholar]
- Stroke mortality in urban and rural Tanzania. Adult morbidity and mortality Project. Lancet. 2000;355:1684-7.
- [Google Scholar]
- Stroke in rural South Africa-contributing to the little known about a big problem. S Afr Med J. 1999;89:63-5.
- [Google Scholar]
- J-shaped relationship between mortality and admission blood pressure in black patients with acute stroke. J Hypertens. 1995;13:1863-8.
- [Google Scholar]
- ICH: External validation and extension of a model for prediction of 30-day survival. Ann Neurol. 1991;29:658-63.
- [Google Scholar]
- Early presentation of hemispheric ICH: Prediction of outcome and guidelines for treatment allocation. Neurology. 1994;44:133-9.
- [Google Scholar]
- Aspects épidémiologiques des accidents vasculaires cérébraux dans le service de tomodensitométrie à l’hôpital du point G. Med Trop. 2005;65:453-7.
- [Google Scholar]
- Changing prognosis of primary ICH: Result of a clinical and CT follow-up study of 104 patients. Stroke. 1988;19:192-5.
- [Google Scholar]
- Prediction of death in patients with ICH: A prospective study of a defined population. J Neurosurg. 2002;97:531-6.
- [Google Scholar]
- Previous antiplaquet therapy is an independent predictor of 30-day mortality after spontaneous supratentorial ICH. J Neurol. 2005;252:412-6.
- [Google Scholar]
- Factors associated with in-hospital mortality following intracerebral hemorrhage: A three-year study in Tehran, Iran. BMC Neurol. 2004;4:9.
- [Google Scholar]
- Risk stratification for in-hospital mortality in spontaneous intracerebral haemorrhage: A Classification and Regression Tree Analysis. QJM. 2006;99:743-50.
- [Google Scholar]
- Site of bleeding and early outcome in primary ICH. Acta Neurol Scand. 2002;105:282-8.
- [Google Scholar]
- Prognostic factors in patients with intracerebral haematoma. J Neurol Neurosurg Psychiatry. 1992;55:653-7.
- [Google Scholar]
- Spontaneous intracranial haemorrhage: Computed tomographic patterns in Accra. West Afr J Med. 2002;21:60-2.
- [Google Scholar]
- Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling Prophecies. Neurology. 2001;56:766-72.
- [Google Scholar]
- Applied logistic regression. New York: John Wiley and Sons; 2000.






