Translate this page into:
Headache in a 27-year-old man: Bilateral serous retinal detachment
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 27-year-old man with a complaint of headache, tinnitus, and visual obscuration presented to a neurologist. Neurologic evaluations, including MRI and CT scan, were within normal limit. The prescribed medicines were propranolol, sumatriptin, valproate sodium, and dexamethasone. Ophthalmic examination was associated with reduction of visual acuity of eyes, bilateral uveitis, and serous retinal detachment. The most probable diagnosis was Vogt-Koyanagi-Harada (VKH) disease. Prescribing high-dose oral steroid and acetazolamide-improved systemic and ocular symptoms. Although HLAB5 is positive in Behηet disease, it also may be seen in VKH.
Keywords
HLA-type
retinal finding
Vogt-Koyanagi–Harada
Introduction
There is a broad spectrum in the differential diagnosis of serous retinal detachment (SRD), particularly when it is bilateral and a history of ocular trauma is lacking.[1] Serous retinal detachment is common in chronic central serous chorioretinopathy (CSCR), posterior scleritis, rhegmatogenous retinal detachment with uveal detachment, multifocal choroiditis, uveal melanoma, metastatic tumor, severe hypertensive choroidopathy, Vogt–Koyanagi–Harada disease, and systemic diseases (myxedema, multiple myeloma).[2]
Behçet disease is chronic-relapsing with multisystemic inflammatory disorders that are characterized by obliterative vasculitis.[3]The major diagnostic criteria were the acute onset of diffuse uveitis in both eyes involving exudative retinal detachment, iridocyclitis, and/or papillary edema and the irritative signs of meningitis. The early ocular change of the disease was confirmed by fluoroscein angiography.[4] Anterior uveitis and occlusive retinal vasculitis with or without retinitis are characteristic of Behçet disease. Rhegmatogenous retinal detachment has been reported. An unspecified type of retinal detachment was observed subsequent to severe necrotizing retinitis.[5]
Very rare cases indicate signs of bilateral SRD, such as Anemic retinopathy secondary to gall bladder cancer, carotid cavernous fistulas, dilated cardiomyopathy, multiple sclerosis, and Waldenström macroglobulinemia.[6–10]
Case Report
A healthy 27-year-old smoker man complaining about prodrome clinical findings, such as severe headache, tinnitus, nausea, and nuchal rigidity for the previous 1 month. He consulted a neurologist; a diagnosis of migranious attack was made and medicine was prescribed accordingly without any relief. He subsequently developed ophthalmic symptom, including red eyes, photophobia, and visual blurring. He has an unremarkable medical and ocular history prior to his complaints. He was not on any systemic medications and had no surgeries in the past. At presentation eyes were red, best corrected visual acuities were 20/100 and 20/200 OD and OS, respectively. Pupils were normal and reactive to light without an RAPD. There was nongranulomatous uveitis and anterior segment examination revealed 2+ of anterior chamber reaction without any other abnormal findings in anterior segmen.
Funduscopic examination showed bilateral 2+ vitritis accompanying with posterior pole and peripheral SRDs [Figure 1]. The fluorescein angiography showed leakage on papilla more prominent in the right eye and uniform hyperautofluorescence in the retina mixed with hypoautofluorescence in the areas of SRD contributed to the diagnosis of VKH [Figures2 and 3].The patient had 3 weeks history of severe headache that did not improve in spite of prescription of propranolol, sumatriptin, valproat sodium, and dexamethason by neurologist. The MRI and CT-scan were within normal limit in neurological evaluations. Laboratory evaluations, including complit blood count, blood chemistries, syphilis serology, antinuclear antibody, angiotensin converting enzym, and purified protein drivative were negative. The patient refused lumbar puncture. He was thought to have presumed VKH in the acute stage with classic intraocular findings thereafter. After ruling out infectious causes that could account for the clinical presentation, the patient was started on 60 mg of prednisone and topical prednisolone 4 times a day. The day after beginning the medicine, his headache was not relieved but his vision was improved; 250 mg oral acetazolamide was also added to medicine once every 6 h. The day after taking acetazolamide the headache relieved and 2 weeks after medical treatment, visual acuities were 20/20 in the both eyes, anterior chamber was quiet and serous detachments were resolved.The steroid was slowly tapered after resolution of the ocular inflammation but 5 mg of prednisolon was continued for 16 months of follow-up without the appearance of any integumentary findings.
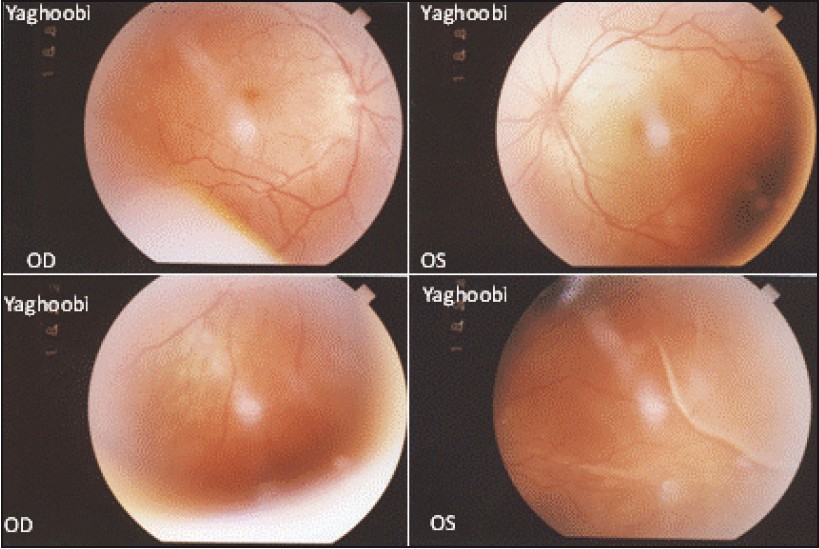
- Serous retinal detachment right and left eye

- The 7th weeks of diseases, both eyes show reduced subretinal accumulation of fluorescein with certain multifocal hyperfluorescent dots (white arrow).

- Fluorescein angiogram on 7th week of diseases showing reduced of bilateral optic disc and retinal detachment and uniform hyperautofluorescence in the macula mixed with hypoautofluorescence in the areas of serous retinal detachment
Discussion
Based on the ophthalmic and systemic manifestations, we present a case of bilateral SRD as a presenting sign of Vogt–Koyanagi–Harada's disease in a HLAB5-positive man. Various investigators have used the criteria proposed by Sugiura, the American Uveitis Society as well as the revised diagnostic criteria proposed by the First VKH International Workshop Group. These 3 sets of criteria share several clinical features that are considered to be essential for establishing the diagnosis of VKH.[111] This disease can be associated with panuveitis as an ocular sign, and can be accompanied by meningismus, auditory findings without integumentary problems. There are genetic factors implicated as one of the pathogenetic signs of VKH and Behçet diseases. As described by Horie et al, certain patients have risk alleles, such as human leukocyte antigen (HLA)-B51 and DR4, but others do not. They report a sister case sharing the same HLA haplotypes but, while the elder sister became ill with Behçet disease the younger was affected with VKH disease.[12]
The present case also showed the positive HLAB5 in VKH disease supporting the risk alleles, such as human leukocyte antigen, in certain diseases. Hashida et al reported a case of VKH subsequently to recurrent of malignant lymphoma, they suggested an association between soluble interleukin-2 receptor levels and disease activity in VKH and malignant lymphoma, which provides additional evidence providing that VKH can be induced by immune disorders caused by high sIL-2R levels in ML.[13]
Vrabechas reported the importance of differential diagnosis between Behçet exudative retinal detachment and other posterior uveitis. He has concluded to consider VKH diseases well, especially if it is recurrent or associated with hemorrhagic retinal vasculitis. He suggested that ocular inflammation often is not the presenting manifestation of Behçet disease and the human leukocyte antigen testing may support the diagnosis.[5] This report provides some insight into the pathogenesis of VKH disease, however the lack of echography findings, optical coherent tomography, and cerebrospinal fluid evaluation are limitations of this report. A study about immunity by Yah et al also explains the role of clinical course in the patient and fine balance between tumor-specific immunity and loss of self-tolerance. They define the ocular and systemic autoimmune sequels resembling VKH, which may develop after successful melanoma immunotherapy.[14]
This case had an interesting clinical presentation in a HLAB5-positive patient without appearing any integumentary findings, but responded well to a combination of oral steroid and acetazolamide against intractable headache. During 16 months of follow-up the patient did not have any recurrences or ocular and systemic complications.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Bilateral retinal detachment in a patient with Vogt-Koyanagi-Harada syndrome. Emerg Radiol. 2005;11:366-71.
- [Google Scholar]
- Systemic corticosteroid treatment in Vogt-Koyanagi-Harada disease. Graefes Arch Clin Exp Ophthalmol. 1982;218:9-13.
- [Google Scholar]
- Bilateral serous macular detachment in a patient with anaemic retinopathy secondary to gall bladder cancer. Br J Ophthalmol. 2002;86:1456-7.
- [Google Scholar]
- Serous retinal detachment following carotid-cavernous fistula. Br J Ophthalmol. 2006;90:1440.
- [Google Scholar]
- Dilated cardiomyopathy, sudden cardiac death, hypoplastic discs, and retinal detachment: A new autosomal dominant syndrome. J Med Genet. 2002;39:221-3.
- [Google Scholar]
- Retinal detachment diagnosed by magnetic resonance imaging. Emerg Med J. 2009;26:304.
- [Google Scholar]
- Bilateral serous macular detachments in Waldenström's macroglobulinaemia. Postgrad Med J. 2009;85:382.
- [Google Scholar]
- Sister cases of Behçet's disease and Vogt–Koyanagi–Harada disease. Br J Ophthalmol. 2008;92:433-4.
- [Google Scholar]
- A Case of Vogt-Koyanagi-Harada Disease Associated with Malignant Lymphoma. JJO. 2005;49:253-6.
- [Google Scholar]
- Ocular and Systemic Autoimmunity after Successful Tumor-Infiltrating Lymphocyte Immunotherapy for Recurrent Metastatic Melanoma. Ophthalmology. 2009;116:981-9.
- [Google Scholar]






