Translate this page into:
Calcified epidural hematoma in pediatric age group: A report of two cases
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The authors present a rare case of calcified (ossified) chronic epidural hematoma developed in a six-and-a-half-year-old female patient who was operated for cerebellar astrocytoma 6 months earlier. There was no history of trauma. Ossified epidural hematoma was seen as an incidental finding in the follow-up in computed tomography scan after 6 months of primary glioma surgery. Ossified chronic epidural hematoma with thick collagenous wall and newly formed bone on dura was excised. The development of calcified chronic subdural hematoma after decompressive intracranial surgery is a well-known occurrence, but the fact that a calcified epidural hematoma, which is rare and which can also develop after decompressive surgery, and the occurrence of calcified (ossified) epidural hematoma after postfossa a glioma surgery is not yet reported. The second case is a 9-year-old male anemic child with a history of fall while playing 5 months earlier who presented with headache of 3 months duration. He had bifrontal calcified epidural hematoma operated by craniotomy and excision of calcified dural edge.
Keywords
Epidural hematoma
pediatric epidural hematoma
calcified
Introduction
Calcification or ossification in a chronic subdural hematoma or cephalhematoma has been already reported. However, ossification of epidural hematoma has been reported earlier.[1–6] Nagane et al[4] reported incidental finding of calcified epidural hematoma after severe head injury. Other authors also reported similar lesions after decompressive brain surgery.[56] We report here two rare cases of ossified epidural hematoma: Case 1—a six-and-a-half-year-old girl operated for right cerebellar pilocytic astrocytoma 6 months earlier, with no history of any trauma; and Case 2: a 9-year-old boy presenting with a mild headache with a history of fall 5 months earlier.
Case Reports
Case 1
A six-and-a-half-year-old right-handed female, an operated case of right cerebellar astrocytoma 6 months earlier in our department, presented in the outpatient department for follow-up, with complaints of mild headache located in the left parietal region without vomiting; she took analgesics that were prescribed for headache. On examination, the child was conscious, alert, afebrile, obeyed verbal commands, had mild right cerebellar signs with normal cranial nerves, and had no motor or sensory deficits.
Computed tomography (CT) scan revealed isodense chronic biconvex type lesion enclosed in a thick and regular (3–4 mm) layer of ossification along the inner border of hematoma. The skull over the outer surface of hematoma was normal. A left parietal osteoplastic flap craniotomy was performed, and after the bone flap was removed, a yellowish, thick, elliptical capsule was noted. The capsule was easily dissected from the surrounding bone. The bisected hematoma capsule revealed a watery fluid. A newly formed bone at the inner border of the hematoma capsule was completely covering the underlying dura. The bone that was attached to the dura was 3 mm thick. The bone was excised by Kerrison punch in piecemeal. After removal of the bone, the dura started coming up. The postoperative course was uneventful. The patient was asymptomatic when discharged. The operative procedure and CT imaging pictures are shown in Figures 1 and 2 in detail.
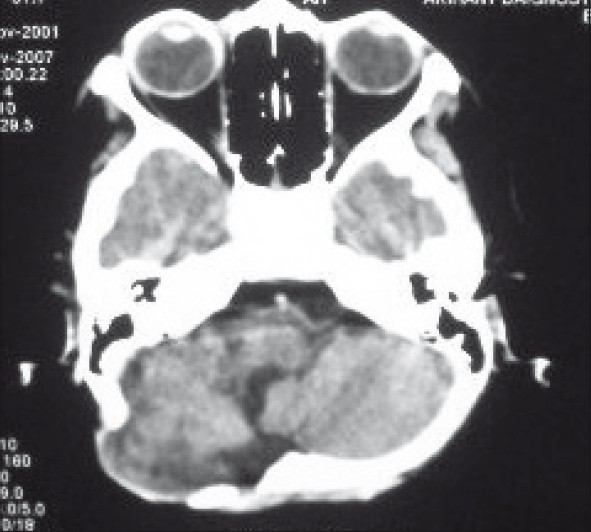
- CT scan showing postoperative posterior fossa craniectomy defect
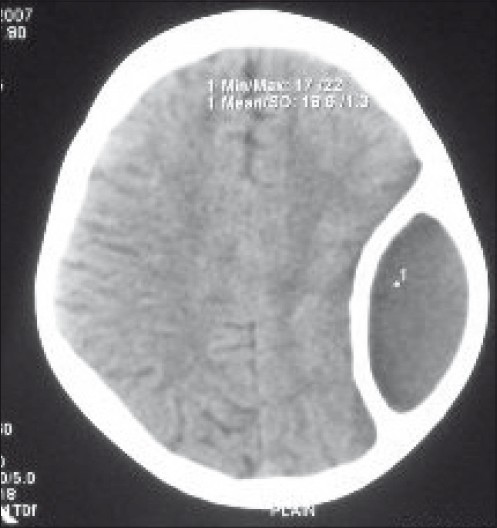
- CT scan axial cuts showing extradural hematoma surrounding calcification
Case 2
A 9-year-old boy presented to us with holocranial headache with dullness since 4 months and was unable to walk properly since 3 months. There was a history of fall at home, while playing 5 months earlier for which no treatment was offered.
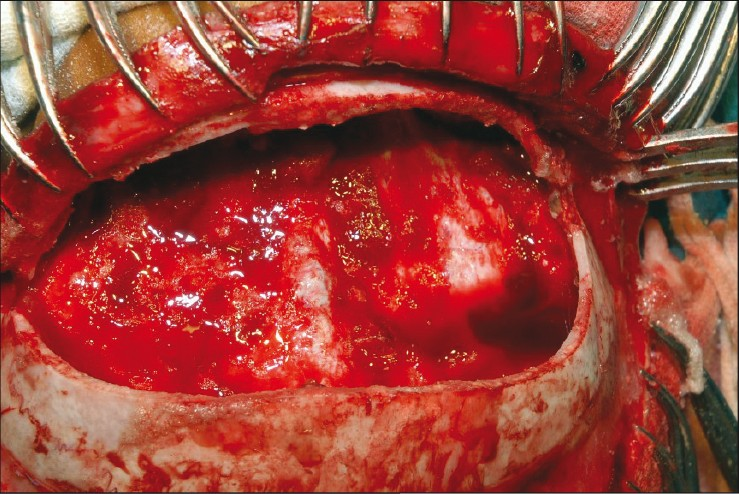
On examination, the patient was grossly anemic, conscious, dull but obeying verbal commands, and there was no gross motor or sensory deficit except papilledema grade II. CT scan revealed a large calcified bilateral epidural hematoma with hypodensity at the center. Hemoglobin was 6 gm%. A bifrontal craniotomy was done and a large chronic hematoma involving the frontal region and liquefied altered blood with thick hard calcified walls, adherent to the duramater, was encountered. Plain was well preserved between the calcified wall and the duramater. Postoperative period was uneventful and the patient was discharged on the 7th postoperative day without neurologic deficit. The patient was given packed cells and investigations for anemia were normal. Operative details are shown in Figures 3–Figure 5.
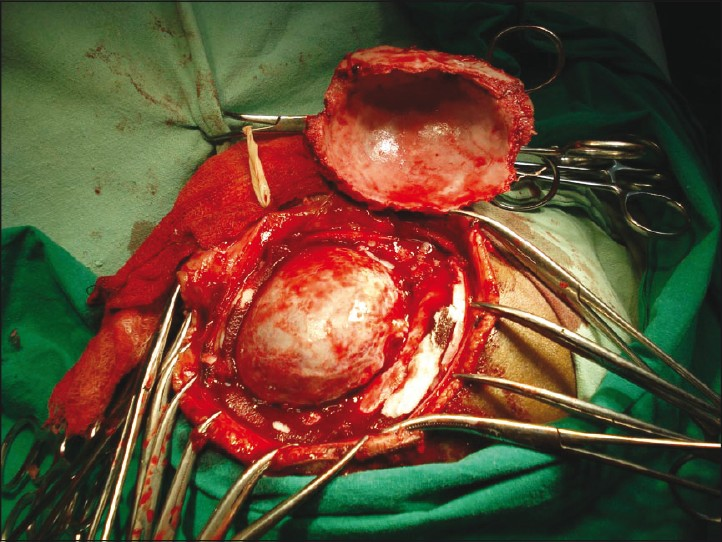
- Intraoperative photograph showing extradural hematoma
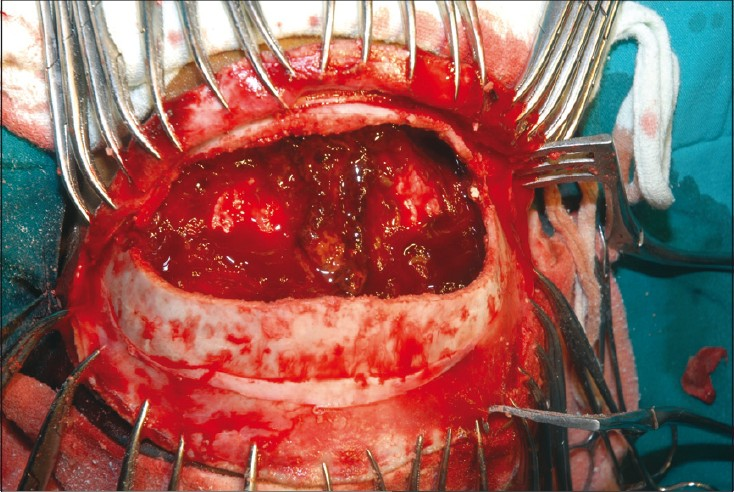
- Ossified dural surface (Case 2)
- After excision of ossified surface (Case 2)
Discussion
In the pediatric age group, an extradural hematoma (EDH) is unusual because the duramater is relatively firmly attached to the inner table and the suture line rather than bleeding from the middle meningeal artery, which is common in adults. In children, the cause of a hematoma can be a hemorrhage of venous blood, which takes longer to accumulate before it causes a significant mass effect, and this could be the reason why most of the children and infants with epidural hematoma show no deterioration of consciousness, and presented with chronic form.[78]
In our case, the patient was operated for right cerebellar astrocytoma 6 months earlier. The patient was asymptomatic for 2 months and then developed mild headache without any neurologic deficits indicating that the first surgery reduced the intracranial pressure and some venous blood oozed out and accumulated at the left parietal region and became chronic. Consequently, ossification developed in a short period before the natural absorption of blood.
Reports have shown that cephalhematoma in neonates is commonly absorbed within 1 month and if it persists for more than a month, it begins to calcify The subperiosteal osteogenesis is responsible for ossification and deformity of the skull in cephalhematoma.[9–12]
Ikakuma and Brunngraber[13] reported that encapsulated epidural hematoma and microscopic ossification were found in the thin layer of granulation tissue on the dural surface. Nakamura et al suggested that a fibroblast layer emerges adjacent to the dura as early as 4 days after bleeding, which develops into sinusoidal channel layers in 2 or 3 weeks. These fibrous layers then extend toward the cranial vault from the hematoma margin and subsequently form a connective tissue layer to form the fibrous capsule around the hematoma.
Iwakuma and Brunngraber[3] also suggested that active bone formation starts at the junction between dura and hematoma, but Nagane et al[4] reported that epidural hematoma ossified in both active and regressive manner, however, require more time. In our case, the ossification developed because of an active process. Osteogenesis occurred at periosteal layer of dura that was in contact with epidural hematoma. The mechanism of ossification in our case is similar to the ossification of cephalhematoma in neonates. The present case is unique in terms of ossification of EDH in contralateral supratentorial space after posterior fossa surgery.
Head injuries are a public health problem worldwide. Incidence of surgical and nonsurgical EDH among patients with traumatic brain injury has been reported to be in the range of 2.7%–4% with mortality around 5% in children and 7%–12.5% in adults. The precise mechanism of an osseous transformation is still not well understood, and it has been hypothesized that damage to vascularized tissues, such as bone and dura provokes inflammation, repair, and remodeling, in the tissues.[14] This natural sequence of healing is more rapid in children than in adults. Moreover, expansion of an EDH may result from repeated bleeding in the inner table of the skull[14] or because of oozing of blood from the dural surface veins.[15]
In conclusion, it can be stated that the blood accumulates slowly from a venous source and becomes chronic EDH and becomes ossified, especially in the pediatric age group. Therefore, close surveillance with serial CT scans are mandatory and urgent removal of EDH should be considered for children with progressive neurologic deficits.
We recommend a detailed examination of the history and serial CT scan after decompressive intracranial surgery and head injury, especially in the pediatric population to identify the early formation of epidural hematoma and removal before it gets ossified.
Source of Support: Nil,
Conflict of Interest: None declared.
References
- Ossified epidural hematoma: Report of case with epilepsy. J Neurosurg Sci. 1985;29:285-8.
- [Google Scholar]
- Chronic extradural hematoma: Report of a case of hematoma in anterior cranial fossa. Bull Los Angeles Neurol Soc. 1944;9:156-62.
- [Google Scholar]
- Extradural ossification following an extradural hematoma. J Neurosurg. 1974;41:104-6.
- [Google Scholar]
- Ossified and calcified epidural hematoma incidentally found 40 years after head injury: Case report. Surg Neurol. 1994;42:65-9.
- [Google Scholar]
- Ossified epidural hematoma following posterior fossa exploration.Report of case. J Neurosurg. 1965;23:214-6.
- [Google Scholar]
- Mild head injury in children. In: Youmans JR, ed. Neurological surgery. Philadelphia: Saunders; 1996. p. :1719-29.
- [Google Scholar]
- Birth trauma. In: Youmans JR, ed. Neurological surgery. Philadelphia: Saunders; 1996. p. :1767-76.
- [Google Scholar]
- Large chronic cephalohematoma without calcification. Pediatr Neurosurg. 1999;30:39-42.
- [Google Scholar]
- Calcification in cephalhematoma of the newborn infant. Am J Obstet Gynecol. 1944;48:702-5.
- [Google Scholar]
- Healing of musculoskeletal tissues. In: Rockwood CA, Green DP, Bucholz RW, eds. Fracture in adults Vol 1. (3rd ed). Philadelphia: Lippincott; 1991. p. :181-22.
- [Google Scholar]
- Chronic epidural haematoma in childhood: Increased recognition and non surgical management. Pediatr Neurol. 1985;1:255-9.
- [Google Scholar]






