Translate this page into:
Frontal intraparenchymal “White epidermoid cyst”: A rare occurrence
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Epidermoid cysts are benign, slow growing, extra-axial rare inclusion lesions accounting for approximately 0.5%–1.5% of all brain tumors. Cerebellopontine angle, petrous apex, suprasellar region, and the fourth ventricle are the usual locations. Only few cases of parenchymal epidermoid cysts have been reported.[12] Frontal lobe epidermoid cyst is extremely unusual.[2] They present with seizures. The symptoms of raised intracranial pressure are conspicuous by their absence. Although computed tomography (CT) scan usually shows a low-density area without contrast enhancement, abnormal CT findings have been reported.[3] Magnetic resonance imaging (MRI) plays an important role in the diagnosis of intraparenchymal epidermoid cysts. They are usually hypointense on T1-weighted sequences and hyperintense on T2-weighted sequences. There may be unusual variation in MRI features..[3] Epidermoid cyst with hyperintensity on T1-weighted images is termed as white epidermoid.[4] We report a rare case of frontal intraparenchymal “white epidermoid cyst” managed at our institute.
A 39-year-old male was admitted with a history of repeated generalized tonic–clonic seizures for 8 months. Neurologic examination revealed no abnormality. CT scan brain showed a 3 × 2.5 × 2 cm, well-defined hypodense mass lesion not enhancing on contrast in the right frontal lobe without perilesional edema [Figure 1]. MRI study showed a similar size contrast nonenhancing lesion, which was hyperintense on T1-weighted images and hypointense on T2-weighted images [Figure 2a and b]. With these imaging findings, a preoperative diagnosis of dermoid cyst vis-à-vis lipoma was considered. Complete removal of the lesion was carried out through a right frontal craniotomy. The cyst was yellowish, thin-walled, containing thick, dirty brown, grumous, oily material [Figure 3]. No hair or other dermal elements were observed. Histopathologic examination showed features of epidermoid cyst, namely, keratinizing squamous epithelium arranged in laminated layers with a thin layer of fibrous connective tissue [Figure 4].
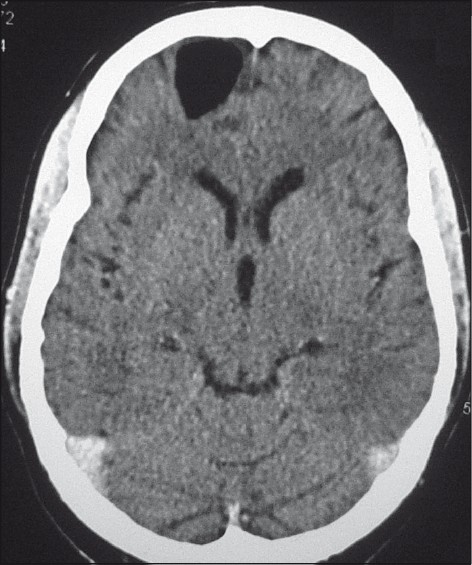
- CT brain (axial view) showing a hypodense lesion in the right frontal lobe

- (a) MRI brain T1-weighted image (coronal view) showing hyperintense lesion in the right frontal lobe. (b) MRI brain T2-weighted image (axial view) showing hypointense lesion in the right frontal lobe

- Intraoperative photograph showing yellowish cystic lesion

- Histopathologic section of the resected specimen showing lamellar keratin flakes. (H and E stain)
MRI appearance depends on the chemical composition of the intracystic contents (cholesterol, keratin, and calcium). The hypointensity on T1-weighted images is due to cholesterol in crystalline form or from calcium. On T2-weighted images, the commonly seen hyperintensity is due to keratin. These lesions usually do not show enhancement on administration of contrast. However, occasionally, they may show mild enhancement, however, exact mechanism of the same is not clear. Abnormal MRI findings include heterogenous appearance on T1- and T2- weighted images.[5] Rarely, these lesions are hyperintense on T1-weighted images and hypointense on T2-weighted images, as in this case. This is because of the higher protein content in the cyst. Horowitz studied five patients having epidermoid cyst and described hyperintensity on T1-weighted images. He felt that this was because of high lipid concentration comprising mixed triglycerides and unsaturated fatty acid residues.[6] No details were reported regarding T2-weighted images.
Since fat (cholesterol) is an irritant for the pachymeninges, care should be taken during excision of these lesions. Due to the cystic nature of the lesion, greater care should be taken to ensure that the cyst does not rupture thereby leading to chemical meningitis. For the same reason, needle aspiration should be avoided and every attempt should be made to excise the cyst completely.
References
- Intracranial epidermoid cyst: Magnetic resonance imaging features. Neurol India. 2009;57:359-60.
- [Google Scholar]
- Intraparenchymal epidermoid cyst of the right frontal lobe: A case report. No Shinkei Geka. 1985;13:695-9.
- [Google Scholar]
- Unusual MR and CT appearance of an epidermoid tumor. AJNR Am J Neuroradiol. 1991;12:771-2.
- [Google Scholar]
- Magnetic resonance imaging of the Fourth ventricular epidermoid tumors. Arch Neurol. 1991;48:438-40.
- [Google Scholar]





