Translate this page into:
Brain metastasis from papillary carcinoma of thyroid gland
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Papillary carcinoma of thyroid is the commonest type of thyroid malignancy.[1] It has an excellent prognosis with a very low incidence of distant metastases.[2] Lung and bone are the usual sites for metastases and associated with an unfavorable prognosis.[3] Brain metastasis from papillary thyroid carcinoma is very rare with a frequency of 0.1 to 5 %.[134]
A 46-year-old lady presented with mild to moderate, continuous, dull-aching left sided frontal headache for two months, along with a history of change in personality. Neurological examination revealed impairment in her recent and remote memory as well as judgment and emotional functions. She had undergone surgery for neck swelling (papillary carcinoma of the thyroid gland) previously. Subsequently she received radiotherapy and was on supplementary dose of thyroxin of 0.1mg/day. There was no history of similar cancer in the family. Magnetic resonance imaging (MRI) brain revealed a contrast enhancing 3 × 2 cm sized lesion in the left frontal lobe, which was isointense on T1WI and hypo intense on T2WI with marked perilesional edema [Figure 1A–C]. X-ray chest as well as an isotope bone scan revealed no abnormalities. Ultrasound scan of abdomen was also normal. Other biochemical parameters were within normal limits. She underwent left frontal craniotomy; intraoperatively a reddish brown, solid, firm, well capsulated minimally vascular lesion was found and excised completely. Histopathological examination was suggestive of metastasis from papillary thyroid carcinoma [Figure 2]. She received radiotherapy (4500 rad, 180 rad / day, for five days a week over a period of five weeks). At one-year follow-up, she was neurologically stable with only mild impairment of her remote memory.
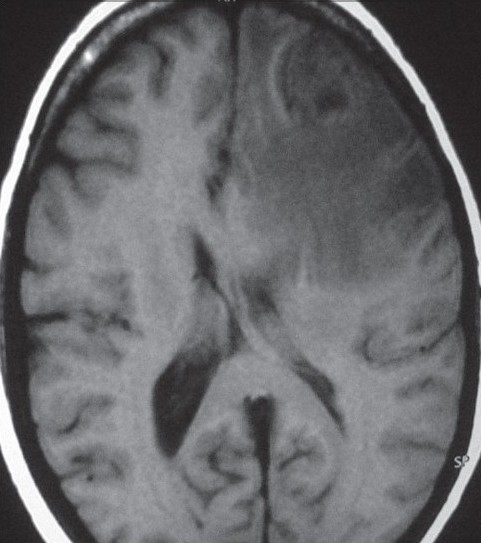
- MRI Brain T1WI (axial view) showing isointense to hypo intense lesion in the left frontal lobe
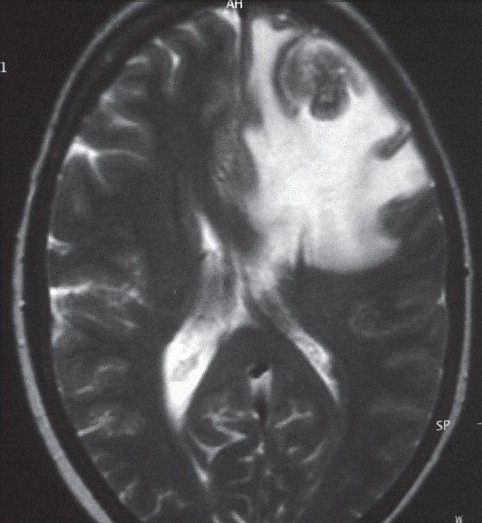
- MRI brain T2WI (axial view) showing isointense to hypo intense lesion in the left frontal lobe
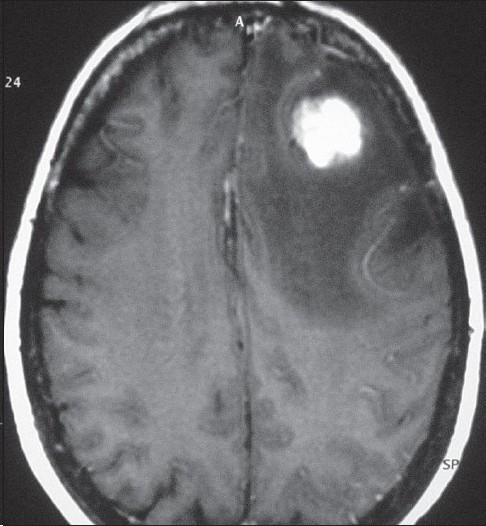
- MRI brain showing uniform enhancement on contrast in the lesion
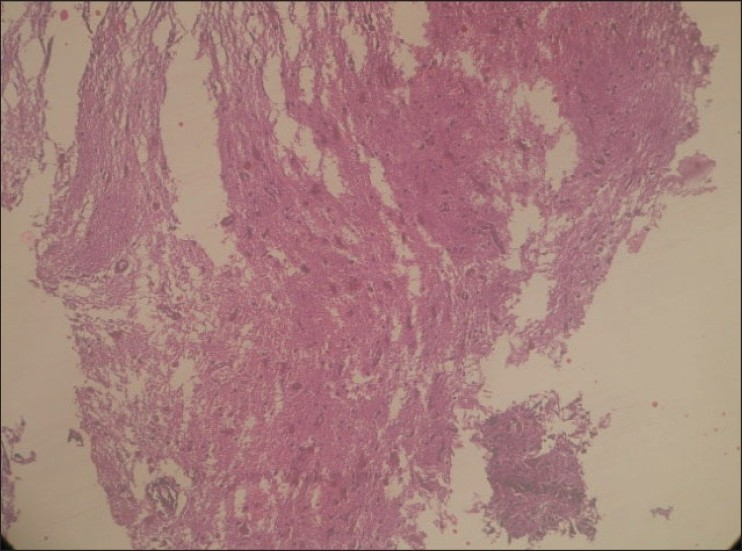
- Cerebral metastasis: well differentiated papillary carcinoma of thyroid (H and E, ×100)
Papillary carcinoma comprises 81.2% of all thyroid malignancies. Incidence of distant metastases at the time of diagnosis is less than 1%.[4] It has less severe clinical course and a favorable long term survival at 10 years (94.9%). Nevertheless, subgroups of patients who develop distant metastasis are known to have a worse prognosis. Age < 20 years and > 60 years, Grade 3 or 4 cancers, thyroid lesion more than 4 cm and extra thyroid lesion at initial examination are associated with a high incidence of distant metastases, which has a serious impact on survival.[3] Average duration between initial diagnosis and distant metastasis to the brain varies from less than a few months to up to 35 years. Signs and symptoms of raised intracranial pressure are the usual presentation and majority of the lesions localize in the frontal, parietal and temporal lobe but some unusual locations are also reported which includes cerebello-pontine angle, cerebellum, pituitary and cavernous sinus.[5] There are no clearly defined guidelines and treatment varies. Available treatment options include conservative treatment, surgical excision, external beam radiation, resection and radioactive iodine, intraoperative implantation of radioactive iodine seeds, thyroxine and radiotherapy, gamma knife radio surgery and radioactive iodine therapy.[6] Therapy must therefore be tailored to each patient. Though several treatment modalities have been used in the treatment of the limited number of cases of intracranial metastatic papillary thyroid carcinoma, results have been equivocal.[7] Although presence of brain metastasis is an overall negative prognostic indicator, Chiu et al. found that surgical resection of brain metastasis may help to significantly prolong survival in patients with differentiated thyroid carcinoma.[8]
References
- Papillary carcinoma of thyroid: A clinicopathological study of 241 cases treated at university of Florence, Italy. Cancer. 1985;5:805-28.
- [Google Scholar]
- A descriptive study of papillary thyroid carcinoma in a teaching hospital in Chennai, India. Asian J Surg. 2002;25:300-3.
- [Google Scholar]
- Distant metastases in papillary thyroid cancer: A review of 91 patients. Cancer. 1988;61:1-6.
- [Google Scholar]
- Papillary thyroid carcinoma: The impact of therapy in 576 patients. Medicine (Baltimore). 1977;56:171-96.
- [Google Scholar]
- Distant metastases in papillary thyroid carcinoma: 100 cases observed at one institution during 5 decades. J Clin Endocrinol Metab. 1995;80:2041-5.
- [Google Scholar]
- Management of brain metastases from thyroid carcinoma: A study of 16 pathologically confirmed cases over 25 years. Cancer. 2003;98:356-62.
- [Google Scholar]
- Unusual brain metastases from papillary thyroid carcinoma: Case report. Neurosurgery. 2001;49:1008-13.
- [Google Scholar]
- Prognosis and treatment of brain metastases in thyroid carcinoma. J Clin Endocrinol Metab. 1997;82:3637-42.
- [Google Scholar]





